Understanding How Wellpoint Can Help Pay for Addiction Treatment
Wellpoint Health Insurance Coverage for Addiction Treatment includes a wide range of services designed to help individuals recover from substance use disorders. Here’s a quick overview of what’s typically covered:
Quick Answer: What Does Wellpoint Cover?
- Detoxification services – Medically supervised withdrawal management
- Inpatient/residential treatment – 24/7 care at treatment facilities
- Outpatient programs – Intensive (IOP), partial hospitalization (PHP), and standard outpatient care
- Medication-Assisted Treatment (MAT) – Medications like Suboxone, methadone, and Vivitrol
- Therapy and counseling – Individual, group, and family sessions
- Dual diagnosis treatment – Care for co-occurring mental health conditions
- Aftercare services – Ongoing support following primary treatment
Coverage varies by plan type (Medicaid, Medicare, or commercial insurance) and your location. Pre-authorization is often required, and staying in-network significantly reduces out-of-pocket costs.
If you or a loved one is struggling with addiction, understanding your insurance benefits can feel overwhelming. The good news is that federal law requires Wellpoint (also known as Anthem, Elevance Health, and Amerigroup) to cover addiction treatment as an essential health benefit. This means that financial barriers don’t have to stand between you and recovery.
Wellpoint plans offer coverage for everything from emergency detox to long-term outpatient therapy, including dual diagnosis treatment for co-occurring mental health conditions. At Addiction Helpline America, we specialize in helping people steer their Wellpoint benefits to find and pay for the right treatment program. Our team is here to walk you through every step, from verifying your coverage to connecting you with a quality care provider.
Understanding Your Wellpoint Addiction Treatment Benefits
If you’ve heard the names Anthem, Elevance Health, or Amerigroup, you’re already familiar with Wellpoint—they’re all part of the same family serving approximately 47 million Americans. Understanding your Wellpoint Health Insurance Coverage for Addiction Treatment is the first step toward recovery. While federal laws guarantee coverage for substance use disorders, the specifics—what you’ll pay and what’s covered—vary based on your plan and state.
The good news is that Wellpoint plans typically include comprehensive behavioral health benefits. Whether you have Medicaid, Medicare, or a commercial plan, addiction treatment is part of your coverage.
Wellpoint Plan Types: Medicaid, Medicare, and Commercial
Knowing your plan type is key to understanding your benefits.
Medicaid plans serve individuals and families with limited income. Wellpoint offers Medicaid in Georgia, Iowa, Maryland, New Jersey, Tennessee, Texas, Washington, and Washington, D.C. These plans are highly affordable, with co-pays often ranging from $0 to $15 for outpatient care and $0 to $100 for inpatient treatment, depending on income.
Medicare plans are for eligible seniors and certain individuals with disabilities. Wellpoint provides Medicare options in Arizona, Iowa, New Mexico, New Jersey, Tennessee, Texas, and Washington. Depending on your plan, you may have no deductibles or co-pays for addiction treatment. You can explore options on the Wellpoint Medicare Plans & Coverage page.
Commercial plans are typically obtained through an employer or the marketplace. They come in metal tiers that determine cost-sharing: Bronze (60% covered), Silver (70%), Gold (80%), and Platinum (90%). Higher-tier plans have lower out-of-pocket costs but higher monthly premiums.
Our team at Addiction Helpline America can help you understand the nuances of your specific plan and find treatment options that work with your coverage.
How Federal Law Ensures Your Coverage
Your right to Wellpoint Health Insurance Coverage for Addiction Treatment is legally protected. The Affordable Care Act (ACA) classifies mental health and substance use disorder services as essential health benefits, meaning most plans must cover them. The ACA also prevents insurers from denying coverage or charging more for pre-existing conditions, including addiction.
The Mental Health Parity and Addiction Equity Act requires that benefits for addiction treatment be comparable to those for medical and surgical care. This means your plan can’t have more restrictive deductibles, co-pays, or treatment limits for addiction services than it does for physical health conditions. You can learn more about these protections on HealthCare.gov’s mental health and substance abuse coverage page.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Comprehensive Care for Dual Diagnosis
It’s common for substance use disorders to co-occur with mental health conditions like depression, anxiety, bipolar disorder, and PTSD. This is known as a dual diagnosis. Treating both conditions simultaneously is crucial for lasting recovery.
Wellpoint recognizes this and provides comprehensive coverage for integrated treatment. Their behavioral health benefits are designed to address both mental health and substance use disorders together. For example, if you’re dealing with bipolar disorder and addiction, your plan is designed to cover simultaneous treatment for both. This integrated approach leads to better outcomes. You can explore their resources on the Wellpoint Mental Health Resources & Coverage page.
What Addiction Treatment Services Are Covered by Wellpoint?
Wellpoint Health Insurance Coverage for Addiction Treatment includes a full range of services to support every stage of recovery. Coverage is based on “medical necessity,” meaning a healthcare professional must recommend the appropriate level of care for your situation. Many plans use the American Society of Addiction Medicine (ASAM) criteria to guide these decisions, ensuring you get the right treatment at the right time.

A Full Spectrum of Care: From Detox to Outpatient
Wellpoint covers a full continuum of care to meet you where you are:
Medical Detoxification: The safe, medically supervised process of removing substances from your body. This is a critical first step for safety and comfort. We can connect you with emergency detox services that accept Wellpoint.
Inpatient Residential Treatment: Provides 24/7 care in a dedicated facility for those with severe addiction or who need a structured environment. Treatment lengths of 30, 60, or 90 days are typically approved based on medical necessity. We can help you find inpatient drug rehab options that work with your plan.
Partial Hospitalization Programs (PHP): Intensive day treatment where you attend therapy and receive medical monitoring for several hours a day, five to seven days a week, while returning home at night.
Intensive Outpatient Programs (IOP): Structured treatment for a few hours per session, several days a week, offering flexibility to maintain work or family life.
Standard Outpatient Programs (OP): The most flexible option, with therapy sessions once or twice a week. Ideal for milder issues or as a step-down from more intensive care.
Therapy and Counseling: The foundation of recovery, including individual, group, and family therapy, is covered across all levels of care.
Virtual Rehab: Many Wellpoint plans now cover online addiction services, allowing you to connect with a therapist via phone or video chat.
Medication-Assisted Treatment (MAT)
For opioid or alcohol addiction, Medication-Assisted Treatment (MAT) combines FDA-approved medications with counseling. Wellpoint plans typically cover MAT programs, which are proven to reduce cravings and support recovery. Covered medications may include:
- Buprenorphine (Suboxone): Reduces opioid cravings and withdrawal symptoms. Wellpoint may cover Buprenorphine-Naloxone therapy.
- Naltrexone (Vivitrol): Blocks the euphoric effects of opioids and reduces alcohol cravings.
- Methadone: Stabilizes patients and reduces illicit opioid use.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Coverage for Various Substance Use Disorders
Wellpoint’s coverage is not limited to a specific substance. If a medical professional deems treatment medically necessary, your plan is designed to cover care for a wide range of addictions, including:
- Alcohol Use Disorder: Find alcohol abuse treatment programs that accept your insurance.
- Opioid Use Disorder: Comprehensive treatment for addiction to prescription painkillers, heroin, or fentanyl.
- Stimulant Addiction: Specialized care for addiction to substances like cocaine and methamphetamines. Get help to wean off methamphetamines.
- Prescription Drug Addiction: Treatment for dependence on benzodiazepines (Xanax, Valium) or prescription stimulants (Adderall, Ritalin).
Your Step-by-Step Guide to Using Wellpoint Health Insurance Coverage for Addiction Treatment
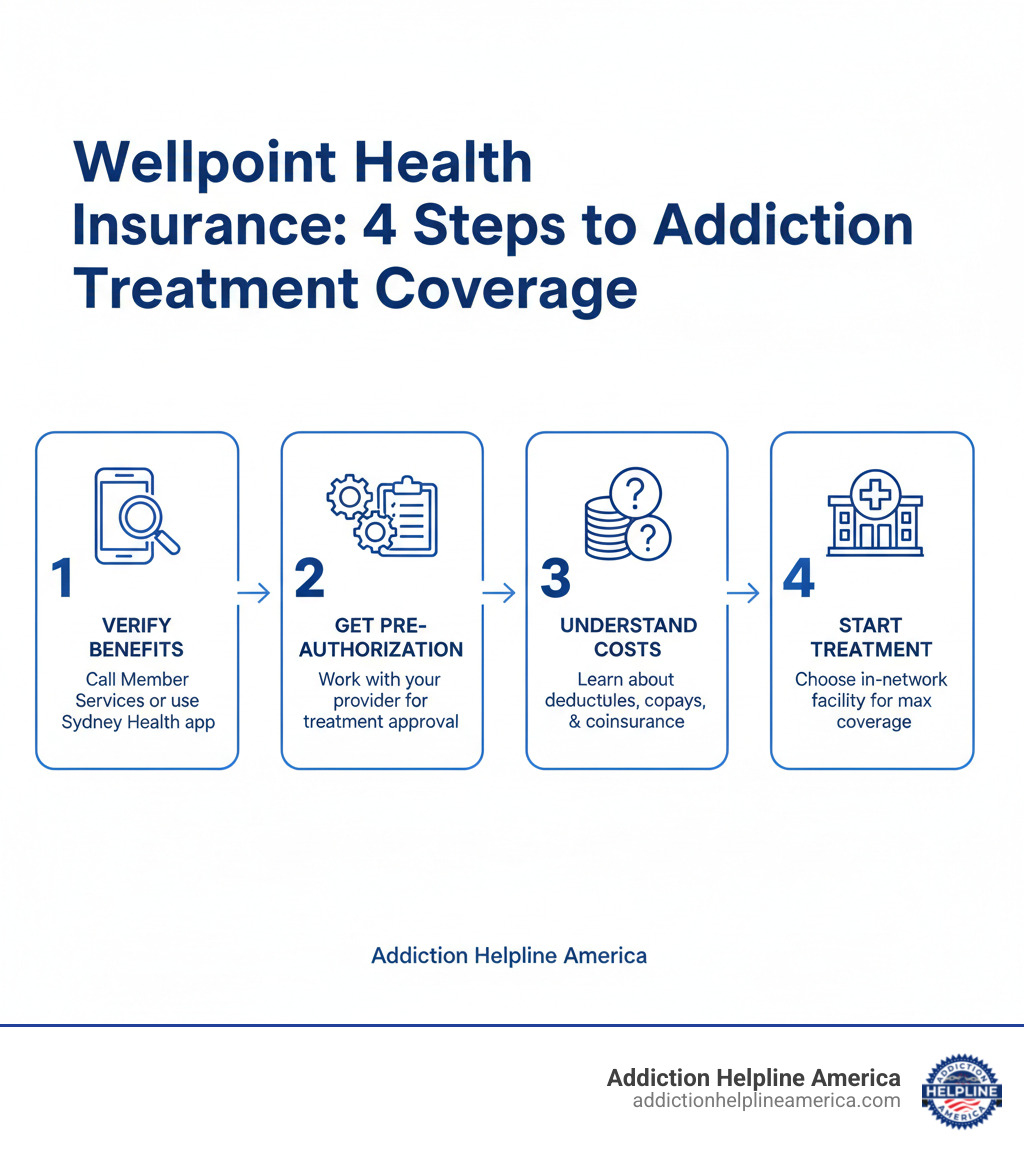
Navigating your Wellpoint Health Insurance Coverage for Addiction Treatment doesn’t have to be complicated. Here’s a simple, step-by-step guide to get you started.

Step 1: Verify Your Benefits and Find In-Network Providers
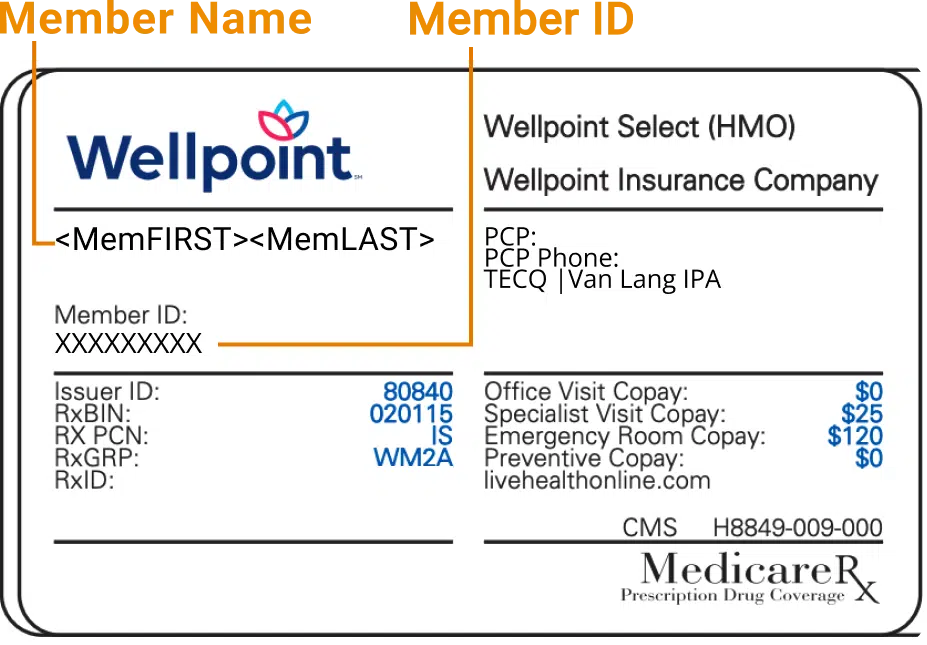
First, confirm what your specific plan covers to avoid surprise bills. Use the Member Services phone number on your insurance card, log into the Wellpoint member portal, or use the Sydney Health app to review your benefits and search for providers.
To save money, it’s crucial to use in-network providers. These are doctors and facilities that have agreed to set rates with Wellpoint, resulting in lower costs for you. Using out-of-network care is significantly more expensive. You can learn more about knowing your health plan’s network on Wellpoint’s site.
Our team at Addiction Helpline America can also help you quickly find a rehab center near you that accepts your Wellpoint plan.
Step 2: Navigating the Pre-Authorization Process
For most intensive services—like inpatient care, PHP, IOP, and detox—Wellpoint requires pre-authorization (or prior authorization). This is the process of confirming that your treatment is medically necessary before it begins. Without this approval, Wellpoint may refuse to pay for your care.
Typically, your chosen treatment facility will handle the pre-authorization request for you. They will submit the necessary medical information to Wellpoint for review. While they manage the process, it’s always a good idea to confirm that approval has been granted before you start treatment. For more information on this process, you can review resources from the American Medical Association on what is prior authorization or our guide on pre-rehab addiction intervention.
Understanding Your Potential Out-of-Pocket Costs with Wellpoint Health Insurance Coverage for Addiction Treatment
Even with insurance, you will likely have some out-of-pocket expenses. Understanding these terms will help you plan:
- Deductible: The amount you must pay for covered services before your insurance starts paying. This amount varies by plan.
- Copayment (Copay): A fixed amount you pay for a service after your deductible is met. Wellpoint Medicaid plans often have very low copays ($0-$15 for outpatient, $0-$100 for inpatient).
- Coinsurance: The percentage of costs you pay for a covered service after you’ve met your deductible. For example, with a Gold plan that covers 80%, your coinsurance would be 20%.
- Out-of-Pocket Maximum: The absolute most you will have to pay for covered services in a plan year. Once you reach this limit, Wellpoint pays 100% of covered costs for the rest of the year.
These costs vary widely, so always verify them for your specific plan. Our team can help you understand the cost of rehab and explore financial assistance options.
What to Do If Your Wellpoint Claim is Denied
Receiving a claim denial for addiction treatment can be disheartening, but it’s not the final word. You have the right to appeal, and many denials are overturned. Mistakes happen, and challenging the decision is often successful. Stay organized, keep copies of all correspondence, and don’t give up.
Common Reasons for Claim Denials
Understanding why a claim was denied is the first step to fixing it. Common reasons include:
- Lack of pre-authorization: The required approval was not obtained before treatment began.
- Not medically necessary: The insurer’s review team disagreed with your provider’s recommendation.
- Out-of-network provider: The facility used was not part of Wellpoint’s network.
- Clerical errors: Simple mistakes like a wrong billing code or a missing signature.
- Coverage limits: The plan’s maximum for a certain service (e.g., number of inpatient days) was reached.
- Experimental treatment: The service was deemed investigational and not covered.
The Appeals Process: A How-To Guide for Wellpoint Health Insurance Coverage for Addiction Treatment
When you get a denial letter, read it carefully. It will explain the reason for the denial and outline the steps to appeal.
Gather Your Evidence: Collect the denial letter, your policy documents, all relevant medical records, and a letter of medical necessity from your healthcare provider explaining why the treatment is essential.
File an Internal Appeal: Submit a formal appeal directly to Wellpoint. In a letter, explain why the denial should be reversed, referencing your policy and the medical necessity of the care. Attach all your supporting documents. Wellpoint has specific deadlines to respond (usually 30-60 days).
Request an External Review: If Wellpoint upholds the denial, you can request an external review from an independent third party. This is done through your state’s Department of Insurance or a designated review organization. The reviewer’s decision is legally binding. The National Association of Insurance Commissioners offers guidance on this process.
This process can be daunting. The team at Addiction Helpline America has extensive experience with insurance appeals and can help you steer the process and advocate for the coverage you deserve.
Frequently Asked Questions About Wellpoint Coverage
Here are concise answers to common questions about Wellpoint Health Insurance Coverage for Addiction Treatment.
Does Wellpoint cover sober living or aftercare programs?
Coverage for sober living homes depends on the situation. Wellpoint may cover them if they are part of a formal, medically necessary step in your treatment plan and are connected to a licensed provider. Standalone sober living homes, often considered housing rather than medical treatment, are typically not covered. Always verify with your plan first.
Aftercare services, however, are generally covered. Most Wellpoint plans include benefits for ongoing support like individual and group therapy, which are crucial for maintaining long-term recovery.
Is addiction treatment for adolescents covered by Wellpoint?
Yes, Wellpoint provides coverage for adolescent addiction treatment. Federal law requires that substance use disorder services be covered as essential health benefits for all ages. However, covered programs, treatment limits, and costs will vary by plan. It is essential to verify the specific benefits for adolescent substance abuse before starting treatment.
What other support resources does Wellpoint offer?
Wellpoint provides several resources to complement your insurance benefits:
- Carelon Behavioral Health: Wellpoint’s partner for managing mental health and substance use care, helping connect members to appropriate services.
- NAMI (National Alliance on Mental Illness): A recommended resource for education, support groups, and advocacy, which is helpful for dual diagnosis.
- Community Resource Link by findhelp: A tool to connect members with local resources for needs like housing, food, and transportation that support stable recovery.
Addiction Helpline America can also help you connect with the right combination of treatment and support services.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Your Path to Recovery Starts Here
Understanding your Wellpoint Health Insurance Coverage for Addiction Treatment is a powerful first step. The most important takeaway is that Wellpoint provides real, comprehensive coverage for addiction treatment, and federal law ensures you have a right to this care. From detox to outpatient therapy, your plan is a lifeline designed to remove financial barriers to healing.
While navigating benefits, pre-authorizations, and in-network providers can seem complex, each step brings you closer to affordable, effective care. And if a claim is denied, remember you have the right to appeal.
At Addiction Helpline America, we specialize in this process. We’ve helped countless individuals and families use their Wellpoint benefits to access life-saving treatment. Our service is free, confidential, and designed to eliminate the stress of finding help. We work with a nationwide network of treatment centers and can quickly find a quality program that accepts your plan.
Recovery is possible. You don’t have to figure this out alone.
Get help navigating your insurance coverage today
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.















