For anyone struggling with the profound impact of trauma, understanding PTSD Treatment can feel like a daunting task. The good news is that effective treatments exist, and recovery is not only possible but common.
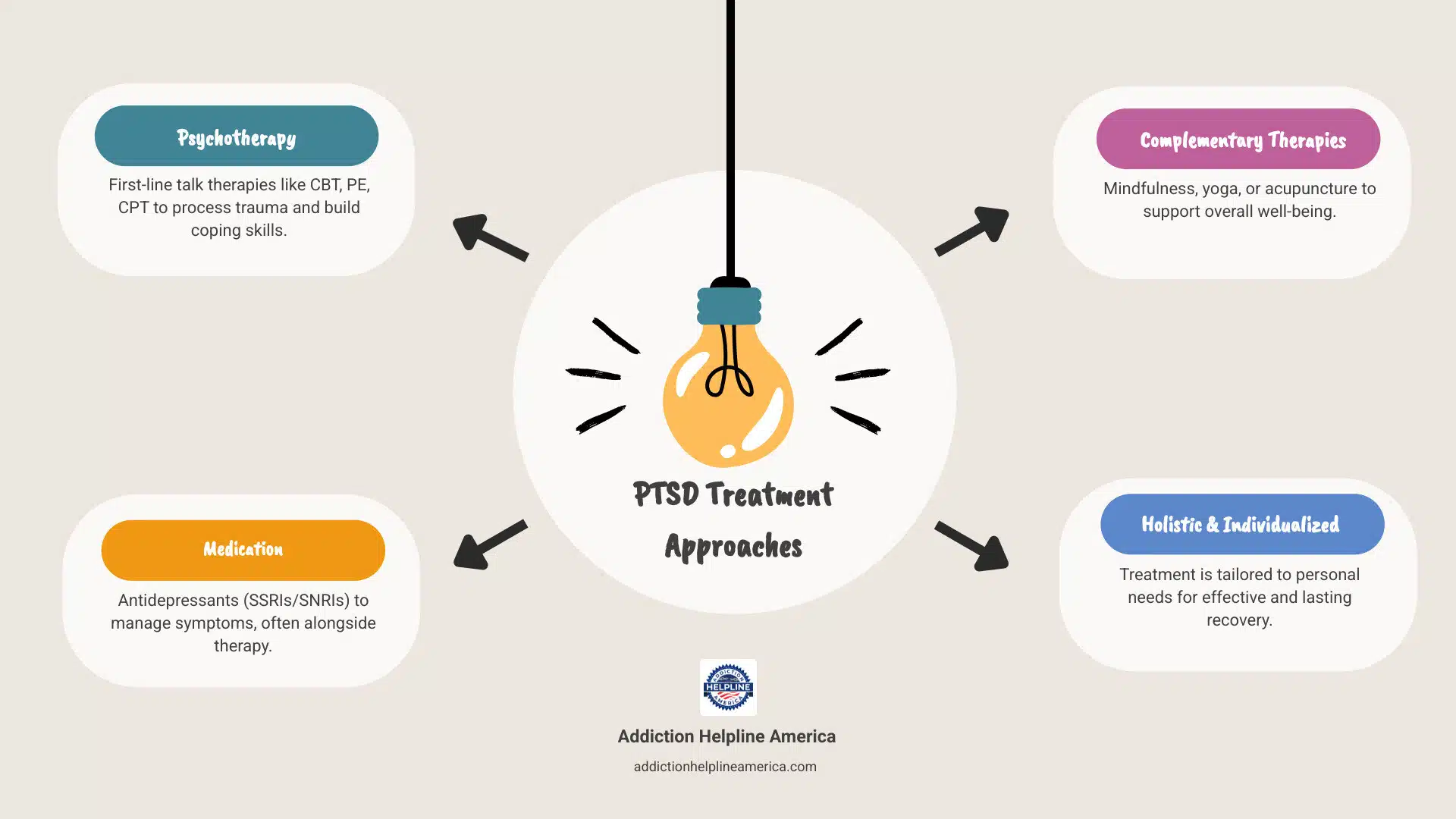
Here are the primary treatment approaches for Post-Traumatic Stress Disorder:
Over the course of a lifetime, as many as seven in 10 adults in the United States will directly experience or witness harrowing events. For some, these experiences can lead to Post-Traumatic Stress Disorder (PTSD), a mental health condition marked by intense, intrusive thoughts and feelings related to the event. While the journey to healing can be challenging, a holistic and individualized approach to care offers a clear path toward reclaiming your life and finding stability. This guide will help you understand the most effective options available.
At Addiction Helpline America, we understand the complexities of mental health challenges, including those related to PTSD Treatment. Our compassionate team offers confidential support and guidance, connecting individuals and families with vital resources and treatment options for substance abuse and co-occurring mental health conditions.
Post-Traumatic Stress Disorder (PTSD) is a mental health condition that can emerge after someone experiences or witnesses a traumatic event. These aren’t just difficult moments—they’re events that deeply threaten your safety or shake the foundation of how you see the world. We’re talking about serious accidents, natural disasters, combat exposure, physical or sexual assault, or the sudden loss of someone you love. What surprises many people is that you don’t have to experience the trauma directly. Learning that something terrible happened to someone close to you can be enough to trigger PTSD.
Here’s something important to understand: feeling scared, sad, angry, or having trouble sleeping after a disturbing event is completely normal. Your brain is processing something overwhelming, and these reactions are part of that process. But if these feelings and reactions stick around for more than a month and start interfering with your daily life—making it hard to work, connect with loved ones, or just get through the day—that’s when professional help becomes crucial.
Early intervention can genuinely change the trajectory of your recovery. Think of it like this: the sooner you address what’s happening, the less time PTSD has to dig its roots deeper into your life.
PTSD symptoms fall into four main categories, and to receive a formal diagnosis, you’d need to experience symptoms from each cluster for at least a month. Let’s walk through what these actually look like in everyday life.
Intrusion symptoms are perhaps the most recognizable. These are the unwanted memories that force their way into your day, whether you’re ready for them or not. You might experience flashbacks that make you feel like the trauma is unfolding all over again, right now. Nightmares can rob you of restful sleep, bringing the trauma back night after night. Intrusive thoughts—those unwanted images or memories that pop up when you’re trying to focus on something else—can be exhausting. Your body might even react physically when something reminds you of the trauma, with sweating, a racing heart, or that sick feeling in your stomach.
Avoidance is your brain’s attempt to protect you, but it can become its own prison. You might find yourself steering clear of places, people, activities, or even conversations that remind you of what happened. Some people describe feeling emotionally numb, like they’re watching life from behind glass, unable to feel joy or connection the way they used to.
Negative changes in thinking and mood can be particularly isolating. You might develop persistent negative beliefs—thinking you’re somehow bad or broken, that others can’t be trusted, or that danger lurks everywhere. Some people struggle to remember important parts of the trauma itself. Activities that once brought happiness might feel pointless now. You might feel detached from the people who care about you most, or experience ongoing fear, anger, guilt, or shame that colors everything.
Changes in arousal and reactivity mean your nervous system is stuck in high gear. You might find yourself snapping at loved ones or experiencing sudden anger outbursts. Some people engage in reckless or self-destructive behavior. Hypervigilance—that constant sense of being on guard, scanning for danger—is exhausting but feels impossible to turn off. You might jump at sudden noises or movements. Concentration becomes difficult, and sleep feels elusive.
It’s worth noting that children with PTSD sometimes show different symptoms. They might appear restless or fidgety, which can unfortunately be mistaken for ADHD, delaying the help they actually need.
Getting a proper diagnosis starts with a comprehensive evaluation from a healthcare professional. This typically includes a physical exam to rule out any medical conditions that might be causing your symptoms, and a detailed mental health evaluation where you’ll discuss what happened, how it’s affecting you, and what symptoms you’re experiencing.
Mental health professionals use the DSM-5-TR criteria to determine whether what you’re experiencing meets the threshold for PTSD. If you’re wondering whether you should seek help, you can start with a brief self-screening test online. It won’t replace a professional evaluation, but it can help you decide whether reaching out for PTSD Treatment makes sense.
Here’s something that often surprises people: while most adults (somewhere between 61% and 80%) will experience a traumatic event at some point in their lives, only about 5% to 10% develop PTSD. Why some people develop it and others don’t remains something of a mystery, but we do know certain factors increase vulnerability.
Military personnel and veterans face significantly higher risk due to combat exposure. About 11% to 20% of veterans who served in Iraq or Afghanistan live with PTSD—a sobering reminder of the invisible wounds of war.
Gender plays a role too. In the general population, PTSD affects roughly 4% of men and 8% of women. This difference isn’t random—women are more likely to experience sexual assault, a type of trauma that carries particularly high risk for developing PTSD.
Previous trauma can make you more susceptible, as can pre-existing mental health conditions like anxiety or depression. A lack of social support after trauma can make recovery much harder—we’re not meant to heal in isolation. Researchers are also exploring how genetics might influence both vulnerability to PTSD and response to treatment, though this field is still evolving.
Sometimes people experience Acute Stress Disorder (ASD) immediately after trauma. It looks a lot like PTSD, with similar symptoms, but there’s an important difference: timing. ASD symptoms last between 3 days and 1 month. If symptoms continue beyond that month mark, the diagnosis typically shifts to PTSD. Think of ASD as your brain’s initial response to overwhelming trauma—sometimes those symptoms resolve, but sometimes they settle in for the long haul.
While PTSD typically stems from a single traumatic event, Complex PTSD (CPTSD) develops when trauma is prolonged or repeated over months or years. This might include ongoing abuse, long-term domestic violence, or extended captivity. The symptoms tend to be more severe and far-reaching, affecting not just your reactions to reminders of trauma but also your ability to regulate emotions, your sense of self, your relationships, and how you view the world. We’ll explore the distinctions between PTSD and CPTSD more thoroughly in our FAQ section.


Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Left untreated, PTSD doesn’t just stay contained—it ripples outward, affecting every corner of someone’s life. The burden grows heavier over time, creating complications that can feel overwhelming.
Co-occurring disorders are incredibly common. PTSD rarely travels alone. Many people develop depression, with its persistent sadness and loss of interest in life. Anxiety disorders often tag along too, whether that’s generalized anxiety, panic attacks, or social anxiety.
Substance use disorder is particularly concerning. When you’re living with intense distress every day, the temptation to self-medicate with alcohol or drugs can be powerful. It offers temporary relief but creates a dangerous cycle. More than 2 in 10 Veterans with PTSD also struggle with substance use disorder, and nearly 1 in 3 Veterans seeking treatment for addiction also have PTSD. The good news is that integrated treatment—addressing both conditions simultaneously—is now the standard of care.
Relationship problems emerge as PTSD symptoms strain connections with the people who care about you most. Irritability, emotional numbness, and avoidance can create distance where there used to be closeness. Family and friends may struggle to understand why you’ve changed, which can lead to conflict and painful isolation.
Impaired daily functioning means PTSD starts interfering with work, school, and social activities. Concentration problems make it hard to focus. Hypervigilance is exhausting. Avoidance shrinks your world. Tasks that used to feel routine can suddenly feel impossible.
Physical health issues develop as chronic stress takes its toll on your body. We’re seeing links between untreated PTSD and cardiovascular disease, chronic pain, and digestive problems. Your mental and physical health are deeply connected.
In severe cases, untreated PTSD can lead to suicidal thoughts. If you or someone you know is having thoughts of self-harm, please reach out immediately—call or text 988 in the US, or go to your nearest emergency department. Help is available, and you don’t have to face this alone.
These long-term effects make one thing clear: seeking PTSD Treatment isn’t just about feeling better—it’s about preventing these complications from taking root. With proper care, you can regain control of your life, rebuild relationships, and find your way back to yourself.
When it comes to PTSD Treatment, we truly believe in a whole-person approach. This means we look at your unique needs and preferences, creating a treatment plan that fits you like a glove. Effective care always starts with making sure you feel safe—both physically and emotionally—and helping with any immediate challenges, like feelings of despair. Sometimes, this even means helping you find basic necessities like food, shelter, or financial support, because a stable foundation is key to healing.
Our recommendations are always guided by what the science tells us works best. In fact, new guidelines for PTSD Treatment were released in 2024 by experts from the U.S. Department of Veterans Affairs and Department of Defense. These guidelines offer clear evidence for and against specific therapies, and they apply to both civilians and military personnel. You can learn more about these new guidelines here.
When we look at psychotherapy (talk therapy) versus pharmacotherapy (medication), studies often show that talk therapies have a bigger impact. They also tend to come with fewer unwanted side effects and are often what people prefer. However, both are excellent first choices, and often, combining the two works wonders. The main goal of any PTSD Treatment is to help you feel safe in your world again and equip you with strong tools to handle stress.

Finding the right medication and dosage can take time and requires close collaboration with your doctor.
SSRIs (Selective Serotonin Reuptake Inhibitors) and SNRIs (Serotonin and Norepinephrine Reuptake Inhibitors) are the most commonly prescribed medications for panic disorder. They work by balancing brain chemicals like serotonin to reduce the frequency and severity of panic attacks. Common examples include fluoxetine (Prozac), sertraline (Zoloft), and venlafaxine (Effexor XR).
These medications take 2 to 8 weeks to reach full effect, so patience is key. They are not addictive, but you should not stop taking them abruptly. Treatment typically continues for at least six months to prevent relapse.
Benzodiazepines, like alprazolam (Xanax), work quickly by calming the nervous system. They are useful for acute panic attacks or as a short-term bridge while waiting for an SSRI to work. However, they are habit-forming, and tolerance can develop quickly. Abruptly stopping them can be dangerous, and they can interfere with the learning process in CBT. Due to the high risk of misuse and addiction, they are generally not a long-term solution, especially for those with a history of substance use.
While professional Panic Disorder Treatment is essential, your daily choices can significantly support your recovery. These self-help strategies are practical tools to help you regain control.
When a panic attack occurs, try to stay where you are (if safe) and use grounding techniques. Focus on your breathing and remind yourself that the attack is temporary and not harmful. The FAQ section of this guide provides more detailed steps for managing an attack.
Psychotherapy, often known as “talk therapy,” is widely seen as the most effective first step in PTSD Treatment. These therapies offer a safe, understanding space where you can gently explore and process traumatic experiences. They help you challenge unhelpful thought patterns that may have taken root and build new, healthier coping skills. The most effective psychotherapies for PTSD are generally “trauma-focused,” meaning they directly address those difficult memories and feelings tied to the traumatic event.
Let’s look at the different types of psychotherapy commonly recommended for PTSD:
Cognitive Behavioral Therapy (CBT) is a big umbrella of therapies that looks at how your thoughts, feelings, and actions are all connected. For PTSD, CBT helps you spot, understand, and change those negative ways of thinking and behaving that developed after the trauma. It’s an active process where you’ll often practice new skills between sessions.
Prolonged Exposure (PE) gently guides you to face your fears by repeatedly and safely confronting trauma-related memories, feelings, and situations. The main idea is to help you realize that these reminders aren’t actually dangerous, and that avoiding them isn’t necessary anymore. PE involves:
You can find More on prolonged exposure therapy for a deeper dive into this approach.
Cognitive Processing Therapy (CPT) is a specific type of CBT. It helps you look at and change upsetting thoughts and beliefs that came from the traumatic experience. CPT focuses on how the trauma changed your view of yourself, others, and the world. By challenging distorted thoughts (like self-blame or guilt), CPT helps you build a more balanced and realistic perspective. Details on cognitive processing therapy show it often follows a structured 12-week plan.
Eye Movement Desensitization and Reprocessing (EMDR) is a unique, VA-approved therapy. In EMDR, you focus on trauma memories while experiencing bilateral stimulation—things like following a therapist’s hand with your eyes, tapping, or listening to sounds. The idea is that this process helps your brain reprocess traumatic memories, making them feel less intense and less vivid. While experts are still learning exactly how EMDR works, studies clearly show it can reduce PTSD symptoms. For more information, you can explore VA-approved Eye movement desensitization and reprocessing resources.
Stress Inoculation Training (SIT) is often part of CBT. It teaches you various coping skills to handle the anxiety and stress linked to trauma. These skills might include relaxation techniques, breathing exercises, and positive self-talk, all designed to help you feel more in control when faced with triggers.
Here’s a quick comparison of some key trauma-focused psychotherapies:
| Therapy | Modality | Duration (Typical) | Focus | | CPT | Individual or Group sessions | ~12 weeks | Focuses on understanding and changing thoughts related to the trauma, reducing emotional distress. | | PE | Individual sessions (can be adapted for group) | 8-15 sessions | Helps individuals gradually approach trauma-related memories, feelings, and situations they’ve been avoiding to reduce fear. | | EMDR | Individual sessions | Varies (8-12 sessions common) | Reprocesses traumatic memories using bilateral stimulation to reduce their emotional intensity and vividness. |
While psychotherapy is often the first and most powerful line of defense, medication can also play a very helpful role in PTSD Treatment. It’s primarily used to manage symptoms, making it easier for you to engage in therapy and improve your overall quality of life. Think of it as a supportive teammate to your therapy, not a solo player.
The medications typically recommended for PTSD primarily work by helping to balance brain chemicals. These include:
Finding the right medication and dosage can take some time, and your doctor will work closely with you to monitor any side effects.
On the flip side, some medications are generally not recommended for long-term PTSD treatment due to their potential harms. Benzodiazepines, for example (like Xanax or Klonopin), might offer quick relief for anxiety, but they aren’t effective for treating core PTSD symptoms. They can also be highly addictive and potentially worsen certain symptoms over time. Your healthcare provider will always discuss the pros and cons of any medication with you, ensuring the safest and most effective path forward.
Find personalized PTSD Treatment and addiction treatment options today
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.
For anyone seeking help for addiction for themselves or a loved one calls to Addiction Helpline America are completely confidential and available 24/7.
Please note: any treatment center listed on our site that receives calls is a paid advertiser.
Calls to a specific treatment center’s listing will be connected directly to that center.
Calls to our general helpline will be answered by treatment providers, all of whom are paid advertisers.
By calling the helpline, you agree to our terms and conditions. These calls are free of charge and carry no obligation to enter treatment. Neither Sober Steps nor anyone answering your call receives a commission or fee based on your choice of treatment provider.
If you’d like to explore additional treatment options or connect with a specific rehab center, you can browse our top-rated listings, visit our homepage, or call us at (844) 561-0606. You may also contact us for further assistance.
Calls to any general helpline will be answered or returned by one of the treatment providers listed, each of which is a paid advertiser:
Our helpline is available 24 hours a day, 7 days a week at no cost to you and with no obligation for you to enter into treatment. We are committed to providing support and guidance whenever you need it.
In some cases, Addiction Helpline America charges our verified partner a modest cost per call. This fee helps us cover the costs of building and maintaining our website, ensuring that we can continue to offer this valuable service to those in need.