Bipolar Disorder Treatment typically involves a combination of medication, psychotherapy, and lifestyle changes. Here’s what you need to know:
Primary Treatment Components:
Treatment is lifelong and requires patience, as finding the right medication combination can take weeks to months.
Bipolar disorder creates intense shifts in mood, energy, and behavior. One moment, a person might feel on top of the world—racing thoughts, bursting with energy, needing little sleep. This is mania. The next, they might plunge into deep depression—exhausted, hopeless, unable to find joy in anything.
These aren’t just mood swings. They’re episodes that can last days, weeks, or even months. They disrupt work, relationships, and daily life. Without treatment, the cycle continues, often getting worse over time.
But here’s the good news: bipolar disorder is manageable. With the right combination of medication, therapy, and support, people with bipolar disorder can achieve stability and live fulfilling lives. Treatment doesn’t cure the condition, but it does bring symptoms under control and significantly reduces the risk of relapse.
The key is getting started—and staying with it. Treatment for bipolar disorder is a long-term commitment, but it works. Studies show that people who stick with their treatment plan experience fewer episodes, better functioning, and improved quality of life.
At Addiction Helpline America, we understand the challenges that come with bipolar disorder, especially when it co-occurs with substance use issues. Our team has extensive experience guiding individuals and families toward comprehensive Bipolar Disorder Treatment options that address both mental health and addiction. We’re here to help you find the right path forward.
Getting the right diagnosis is the first step toward effective Bipolar Disorder Treatment. But understanding what you’re dealing with—and how doctors figure it out—can feel overwhelming at first. Let’s break it down.
Bipolar disorder is a serious mental health condition that causes dramatic shifts in mood, energy, and behavior. These aren’t your everyday ups and downs. We’re talking about episodes that can last days, weeks, or even months. During a manic episode, someone might feel invincible, need almost no sleep, talk rapidly, and make impulsive decisions. During a depressive episode, that same person might struggle to get out of bed, lose interest in everything they once loved, and feel utterly hopeless.
The condition typically shows up in adolescence or early adulthood, though it can appear at any age. It affects people differently, but one thing’s consistent: it has a profound impact on daily life, relationships, and overall functioning.
Globally, research shows that about 0.6% of people experience Bipolar I disorder, while about 0.4% have Bipolar II disorder. Another 1.4% experience what’s called subthreshold bipolar disorder—symptoms that don’t quite meet the full diagnostic criteria but still cause significant problems. Many people live with residual symptoms even between major episodes, which is why ongoing treatment and monitoring are so important.
There are several types of bipolar disorder, and understanding which one you have matters for treatment:
Bipolar I Disorder involves at least one full manic episode. These episodes are severe—they can include psychotic features like hallucinations or delusions, and they often require hospitalization. Major depressive episodes usually happen too, though they’re not required for the diagnosis.
Bipolar II Disorder is characterized by at least one major depressive episode and at least one hypomanic episode, but never a full-blown manic episode. Don’t let the “II” fool you—this isn’t a milder version of the illness. The depressive episodes in Bipolar II are often longer and more debilitating.
Hypomania is a less intense form of mania. Your mood is liftd, you have more energy than usual, and you might feel unusually productive or creative. But unlike full mania, hypomania doesn’t typically involve psychosis or require hospitalization. Still, it can lead to poor judgment and create problems in your life.
Mixed episodes are particularly challenging. Imagine feeling the racing thoughts and agitation of mania while simultaneously experiencing the hopelessness and sadness of depression. It’s as distressing as it sounds, and many people describe mixed episodes as the worst part of having bipolar disorder. The risk of suicide is especially high during these periods.
Cyclothymia is a milder, chronic form of the condition. Over at least two years, you experience ongoing mood swings between hypomania and mild depression, but the symptoms aren’t severe enough to meet the full criteria for manic or major depressive episodes.

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
There’s no blood test or brain scan that can diagnose bipolar disorder. Instead, doctors rely on a thorough evaluation that looks at your symptoms, history, and patterns over time.
Your doctor will start with a physical exam and lab tests. They’ll want to rule out other medical conditions that can mimic bipolar symptoms. For example, thyroid problems can cause mood swings, fatigue, and changes in energy levels. Blood work helps make sure something else isn’t causing your symptoms.
Next comes a detailed mental health assessment. A psychiatrist or mental health professional will ask about your thoughts, feelings, and behaviors. They’ll want to know when your symptoms started, how your moods change, and whether your symptoms interfere with work, relationships, or daily activities. They’ll also assess whether you’ve had thoughts of suicide—a critical question, since up to one-third of people with bipolar disorder will attempt suicide at some point, and 6-7% complete it.
Mood charting is an incredibly useful tool. You’ll keep a daily record of your moods, sleep patterns, energy levels, and any triggers you notice. Over time, patterns emerge that help both you and your doctor understand what’s happening. This information also helps track how well treatments are working.
Mental health professionals use the DSM-5 criteria—the Diagnostic and Statistical Manual of Mental Disorders—to make an accurate diagnosis. They’re looking for specific patterns of manic, hypomanic, and depressive episodes that meet certain duration and severity requirements.
Family history is another important piece of the puzzle. Bipolar disorder is one of the most heritable psychiatric conditions. More than two-thirds of people with bipolar disorder have at least one close biological relative with the condition. If bipolar disorder runs in your family, your doctor needs to know.
Co-occurring conditions complicate the picture. Three-quarters of people with bipolar disorder have a history of at least three additional mental health conditions. ADHD, anxiety disorders, and substance use disorders are especially common. These overlapping conditions can make diagnosis trickier and require an integrated treatment approach that addresses everything at once.
Diagnosing children and teens presents unique challenges. Adolescents naturally experience mood swings as part of development, so distinguishing normal teenage behavior from bipolar disorder takes expertise. Symptoms may also present differently in younger people, and co-occurring conditions like ADHD are common, which can muddy the waters.
At Addiction Helpline America, we understand how confusing and overwhelming the diagnostic process can feel. We’re here to help you steer it and connect you with professionals who specialize in accurate assessment and comprehensive Bipolar Disorder Treatment.
Both Bipolar I and Bipolar II involve significant mood shifts, but the differences between them matter—a lot—when it comes to treatment.
| Feature | Bipolar I Disorder | Bipolar II Disorder |
|---|---|---|
| Manic Episodes | At least one full manic episode (lasting 7+ days or requiring hospitalization) | No full manic episodes; only hypomanic episodes |
| Hypomanic Episodes | May occur, but not required for diagnosis if a full manic episode is present | At least one hypomanic episode (lasting 4+ consecutive days) |
| Depressive Episodes | Common, often severe, and can be more frequent than manic episodes | Required for diagnosis, often more frequent, longer, and debilitating than in Bipolar I |
| Psychosis | Can occur during manic or severe depressive episodes | Does not occur during hypomanic episodes; can occur during severe depressive episodes |
| Impact on Functioning | Manic episodes cause marked impairment, may require hospitalization, or include psychotic features | Hypomanic episodes do not cause marked impairment or psychosis, but depressive episodes do |
| Treatment Implications | Antidepressants used with extreme caution, always with mood stabilizers/antipsychotics | Antidepressants may be used, sometimes alone, but still require careful monitoring |
The severity of mania is the key difference. Bipolar I involves severe, potentially dangerous manic episodes that can include psychotic features and often require hospitalization. Bipolar II features less intense hypomanic episodes that don’t cause the same level of impairment or include psychosis.
The presence of psychosis—hallucinations or delusions—can occur in Bipolar I during manic or severe depressive phases. In Bipolar II, psychosis doesn’t happen during hypomanic episodes, though it can occur during severe depression.
Here’s something that surprises many people: depressive episodes are often more common, longer, and more debilitating in Bipolar II than in Bipolar I. This is why Bipolar II is sometimes misdiagnosed as major depression—the hypomanic episodes might be brief or feel good enough that they’re not reported or recognized.
The impact on functioning differs significantly. Manic episodes in Bipolar I cause marked impairment and can be dangerous. Hypomanic episodes in Bipolar II might actually feel productive or even enjoyable, though they can still lead to poor judgment and relationship problems. However, the depressive episodes in Bipolar II are just as serious and impairing as those in Bipolar I.
These distinctions directly influence treatment implications. In Bipolar I, antidepressants must be used with extreme caution—they can trigger manic episodes and should always be combined with mood stabilizers or antipsychotics. In Bipolar II, antidepressants may sometimes be used alone, though careful monitoring is still essential.
Understanding which type of bipolar disorder you have helps your treatment team create the most effective plan for you. The right diagnosis leads to the right treatment, and that’s what brings stability and hope.
When you’re navigating Bipolar Disorder Treatment, it’s important to understand that you’re not just treating a single symptom—you’re managing a complex condition that requires a comprehensive approach. Think of it like managing diabetes or heart disease. You wouldn’t rely on just one intervention. The same is true here.
The most effective treatment combines medication with psychotherapy. This isn’t just our opinion—it’s backed by solid research. Studies consistently show that people taking medication for bipolar disorder recover faster and stay well longer when they also participate in therapy. Scientific research on psychotherapy effectiveness confirms what we’ve seen time and again: the combination works better than either approach alone.
Our focus with treatment centers on three essential goals: symptom control to stabilize your moods and reduce the intensity of episodes, relapse prevention to help you identify triggers and avoid future episodes, and functional improvement so you can rebuild stability in your work, relationships, and everyday life.
At Addiction Helpline America, we’ve helped countless individuals find treatment programs that address both bipolar disorder and co-occurring substance use issues. We understand that these conditions often go hand-in-hand, and we’re here to connect you with providers who can treat both effectively.
Medication forms the foundation of Bipolar Disorder Treatment, especially when you’re in the middle of an acute episode and need to regain stability. Here’s something important to understand right from the start: finding the right medication takes time. What works for one person might not work for another. You might need to try several options before finding the combination that gives you the best results with the fewest side effects.
This process requires patience and close partnership with your psychiatrist. It’s not a sign that treatment isn’t working—it’s just how we find what works best for your unique brain chemistry.
Mood stabilizers are typically the first line of defense. These medications work to even out the highs and lows that define bipolar disorder. Lithium is the oldest mood stabilizer we have, and it remains one of the most effective, particularly for classic euphoric mania and preventing future episodes.
It also has proven anti-suicidal properties, which is crucial given the high risk of suicide in bipolar disorder. Your doctor will aim for therapeutic serum levels between 0.6-1.0 meq/litre during acute episodes and 0.6-0.8 meq/litre for long-term prevention.
Regular blood tests aren’t optional with lithium—they’re essential to keep levels in the safe zone and prevent toxicity, which can happen if levels rise above 1.5 meq/litre. You might experience side effects like tremors, increased thirst, or kidney concerns.
Here’s an important tip: anything that lowers your sodium levels (like a low-sodium diet, heavy sweating, vomiting, or diarrhea) can cause lithium to build up to toxic levels. Lithium is also not recommended during pregnancy due to potential risks to the developing baby.
Valproic acid (Depakote) is an anticonvulsant that doubles as a mood stabilizer. It’s particularly effective for mixed episodes and rapid cycling, where moods shift quickly. Therapeutic levels typically range from 50-100µg/ml. Side effects can include drowsiness, nausea, and potential liver problems. Like lithium, it carries pregnancy risks.
Lamotrigine (Lamictal) is another anticonvulsant with both antidepressant and anti-manic properties. It’s especially useful for preventing bipolar depression, which is often the more debilitating phase for many people. The main concern with lamotrigine is a skin rash, which you need to report to your doctor immediately if it develops.
Carbamazepine (Tegretol) is yet another anticonvulsant used as a mood stabilizer, particularly helpful for rapid cycling. Therapeutic levels are commonly 4-12 µg/ml, and your doctor will monitor your liver function and blood counts regularly.
Atypical antipsychotics (also called second-generation antipsychotics) have become increasingly important in treating bipolar disorder. These medications—including olanzapine (Zyprexa), risperidone (Risperdal), quetiapine (Seroquel), aripiprazole (Abilify), cariprazine (Vraylar), and lurasidone (Latuda)—are often used alongside mood stabilizers to treat acute mania, bipolar depression, and for ongoing maintenance. They’re particularly helpful if you experience psychotic symptoms during manic or severe depressive episodes. These medications have a broader mood-stabilizing effect than their name suggests. Common side effects include weight gain, metabolic changes, and drowsiness.
Now, here’s where things get complicated: antidepressants. Their use in bipolar disorder is controversial and requires extreme caution. They should never be used alone for bipolar depression because they can trigger manic or hypomanic episodes, especially in Bipolar I disorder. If your doctor does prescribe an antidepressant, it will always be combined with a mood stabilizer or antipsychotic to prevent a “switch” to mania. Bupropion has a lower risk of causing this switch compared to other antidepressants.
One FDA-approved combination is Symbyax, which combines olanzapine and fluoxetine specifically for treating bipolar depression.
While medication stabilizes your brain chemistry, psychotherapy gives you the tools to manage your life with bipolar disorder. It’s not just “talk therapy”—it’s skill-building, education, and support all rolled into one. Research shows that therapy works best when combined with medication, creating a powerful one-two punch against bipolar disorder.
Cognitive Behavioral Therapy (CBT) helps you identify and change negative thought patterns and behaviors that can trigger or worsen mood episodes. In bipolar disorder, CBT focuses specifically on managing symptoms, recognizing and avoiding triggers, and developing problem-solving skills for daily challenges.
Interpersonal and Social Rhythm Therapy (IPSRT) operates on a fascinating principle: your daily routines (social rhythms) directly affect your biological rhythms, which in turn affect your mood. This therapy helps you develop consistent daily schedules for sleeping, eating, and exercising. By keeping these routines stable, you can minimize mood fluctuations. It sounds simple, but the impact can be profound.
Family-Focused Therapy recognizes an important truth: bipolar disorder doesn’t just affect you—it affects everyone who cares about you. This therapy educates family members about the condition, improves communication, and teaches problem-solving skills so your support system can help you manage the illness more effectively.
Psychoeducation might sound basic, but it’s incredibly powerful. Studies show that when paired with medication, psychoeducation improves medication adherence and reduces hospitalizations. Simply understanding what’s happening in your brain, what to watch for, and how to respond can make an enormous difference.
Dialectical Behavior Therapy (DBT) was originally developed for borderline personality disorder, but research indicates it can also help with bipolar disorder. It’s particularly effective for managing intense emotions and reducing suicidal behaviors. One clinical trial found DBT helpful in decreasing suicide attempts in teens with bipolar disorder.
Through these therapies, you’ll develop crucial skills: mood monitoring to catch early warning signs, coping strategies for stress and difficult emotions, problem-solving for relationship and work challenges, communication skills to improve your interactions, relapse prevention through identifying triggers and creating action plans, mindfulness to develop awareness without judgment, and routine establishment to maintain consistent daily schedules.
These aren’t just abstract concepts—they’re practical tools you’ll use every single day to maintain your stability and build the life you want.
Medication and therapy are absolutely essential, but they’re only part of the picture. The daily choices you make—how you sleep, eat, move, and manage stress—can be just as powerful in keeping your moods stable. Think of Bipolar Disorder Treatment like tending a garden: you need the right tools (medication and therapy), but you also need consistent care, the right environment, and a little help from friends.

A predictable routine is protective. Waking, eating, and sleeping at the same times helps regulate your brain’s internal clock. Sleep is especially critical; aim for 7-9 hours per night on a consistent schedule, as too little sleep can trigger mania and too much can worsen depression.
A healthy diet and regular exercise also support brain health. Scientific research on exercise for mood disorders shows that physical activity can reduce depressive symptoms. Aim for 30-40 minutes of moderate exercise a few times a week. Learning to manage stress through techniques like yoga, meditation, or deep breathing is also key.
It is critical to avoid alcohol and drugs, as they interfere with medications and can trigger severe mood episodes. An estimated 60% of people with bipolar disorder also struggle with substance dependence, making integrated treatment essential.
You don’t have to manage bipolar disorder alone. A strong support network of family, friends, and peers is a vital resource.
Educating your loved ones helps them understand the illness and how to offer effective support. Support groups connect you with others who have similar experiences, providing practical advice and hope. National organizations like the National Alliance on Mental Illness (NAMI) and the Depression and Bipolar Support Alliance (DBSA) offer local and online groups, educational programs, and valuable resources.
Sticking with treatment can be difficult. Up to 60% of people with bipolar disorder struggle with adherence for several reasons:
Ongoing monitoring with your healthcare team is a partnership that helps steer these challenges and ensures your treatment remains effective.
When standard Bipolar Disorder Treatment isn’t enough, specialized and intensive options are available. These are not a sign of failure but additional tools for complex situations.
For treatment-resistant bipolar disorder, where multiple medication trials have been unsuccessful, advanced interventions can offer hope. Hospitalization may be necessary during severe episodes to ensure safety, provide 24/7 monitoring, and rapidly adjust medications. Intensive outpatient programs (IOPs) offer a step-down level of care, providing structured treatment for several hours a day while allowing you to live at home.

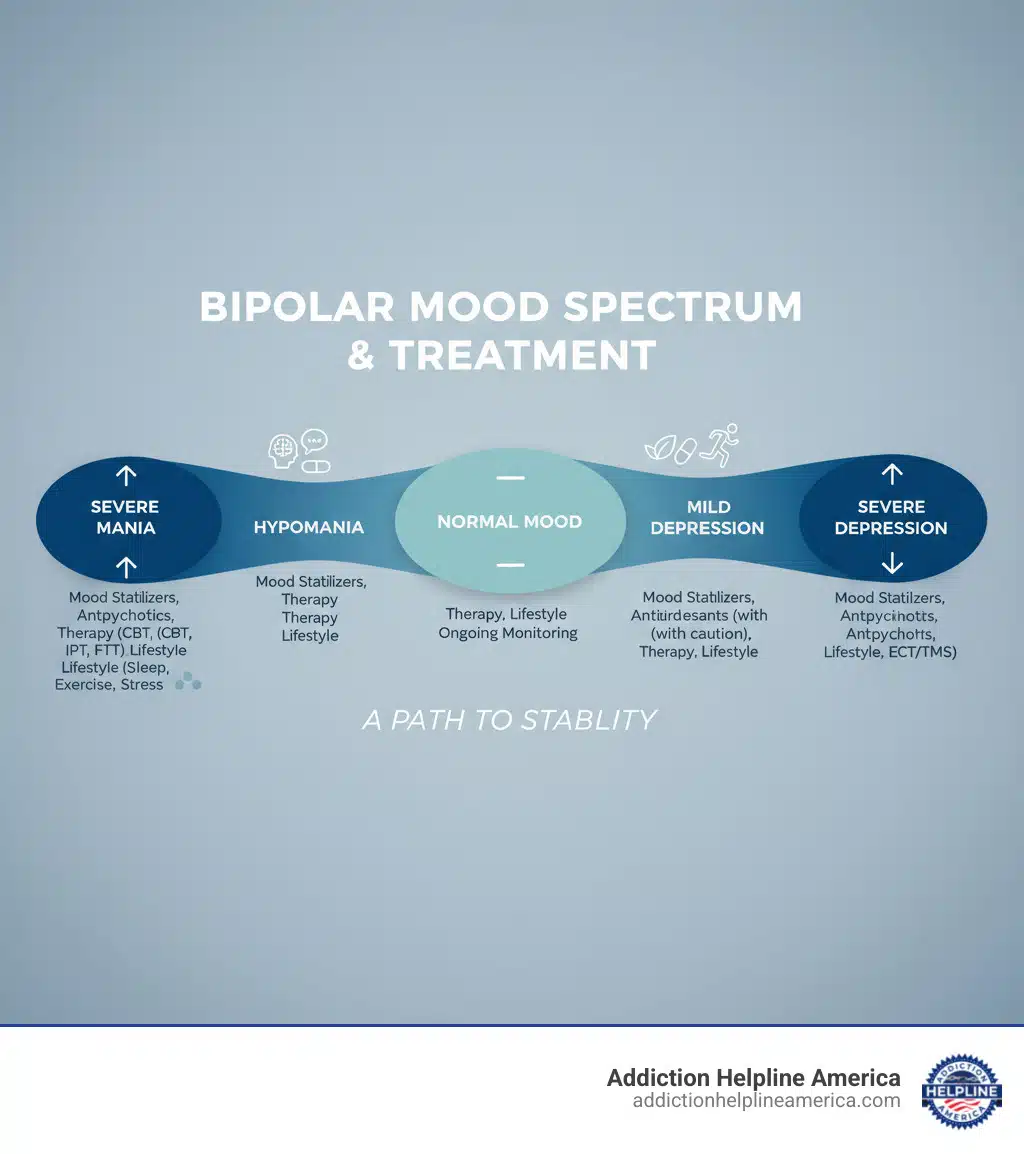
Treatment must be adapted to the type of mood episode:
When first-line treatments fail, these options may be considered:
If standard approaches aren’t working, Addiction Helpline America can help you explore these advanced options and connect you with specialized providers.

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
When starting Bipolar Disorder Treatment, many people have the same questions. Here are concise answers to the most common ones.
No, bipolar disorder is a lifelong condition that cannot be cured. However, it is highly manageable. The goal of treatment is not to eliminate the illness but to control symptoms, maintain long-term stability, and prevent relapse. With consistent management, you can live a full and productive life.
The timeline varies. Some medications can reduce acute symptoms within days, but achieving full mood stabilization often takes several weeks to months. Finding the right medication is a process of trial and error that requires patience and open communication with your doctor. Never stop or change your medication dosage without consulting your provider.
Common side effects include weight gain, drowsiness, dizziness, nausea, and tremors. Some medications can also cause metabolic changes, which is why regular blood tests are necessary. While side effects can be frustrating, many can be managed. It is crucial to discuss any side effects with your doctor rather than stopping your medication. They can adjust your dosage, switch medications, or find other ways to minimize discomfort while maintaining mood stability.
Living with bipolar disorder requires a commitment to lifelong management, but recovery and stability are entirely possible. The most effective Bipolar Disorder Treatment integrates several pillars: medication for biological balance, therapy to build coping skills, lifestyle routines to support stability, and a strong support network.
The path isn’t always straight, but with consistent treatment, people with bipolar disorder can and do live full, joyful lives.
We know that bipolar disorder often co-occurs with substance use—about 60% of individuals with the condition also face addiction. This complicates recovery and makes integrated treatment essential. Addiction Helpline America specializes in this area. We have a nationwide network of treatment centers that are experts in handling co-occurring disorders.
Our guidance is free, confidential, and personalized. We listen to your story and connect you with the right program for your specific needs, insurance, and circumstances. We are not here to pressure you, but to provide options and support.
If you or a loved one are ready to explore treatment, we are here to help you take the next step. You deserve stability and support, and you don’t have to find it alone.
Find personalized mental health and addiction treatment options
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.
For anyone seeking help for addiction for themselves or a loved one calls to Addiction Helpline America are completely confidential and available 24/7.
Please note: any treatment center listed on our site that receives calls is a paid advertiser.
Calls to a specific treatment center’s listing will be connected directly to that center.
Calls to our general helpline will be answered by treatment providers, all of whom are paid advertisers.
By calling the helpline, you agree to our terms and conditions. These calls are free of charge and carry no obligation to enter treatment. Neither Sober Steps nor anyone answering your call receives a commission or fee based on your choice of treatment provider.
If you’d like to explore additional treatment options or connect with a specific rehab center, you can browse our top-rated listings, visit our homepage, or call us at (844) 561-0606. You may also contact us for further assistance.
Calls to any general helpline will be answered or returned by one of the treatment providers listed, each of which is a paid advertiser:
Our helpline is available 24 hours a day, 7 days a week at no cost to you and with no obligation for you to enter into treatment. We are committed to providing support and guidance whenever you need it.
In some cases, Addiction Helpline America charges our verified partner a modest cost per call. This fee helps us cover the costs of building and maintaining our website, ensuring that we can continue to offer this valuable service to those in need.