
Why Understanding Your Options for Major Depression Treatments Matters
Major depression treatments have come a long way, and the good news is that they work. In fact, approximately 80% to 90% of people with depression who seek treatment eventually respond well to it. If you or someone you love is struggling with major depressive disorder (MDD), you’re not facing this alone—and you don’t have to figure it out by yourself.
Quick Answer: What Are the Main Treatment Options?
The primary major depression treatments include:
- Antidepressant Medications – SSRIs, SNRIs, and other classes that help restore brain chemistry balance
- Psychotherapy – Evidence-based talk therapy like Cognitive Behavioral Therapy (CBT) and Interpersonal Therapy (IPT)
- Combination Treatment – Medication plus therapy, often most effective for moderate to severe depression
- Brain Stimulation Therapies – ECT, TMS, or VNS for severe or treatment-resistant depression
- Lifestyle Changes – Exercise, healthy diet, sleep, and stress management to support recovery
Timeline: Most people start feeling better within 1-2 weeks, with full effects typically seen in 4-8 weeks.
Major depressive disorder is much more than simple unhappiness. It’s a serious medical condition that affects your whole body—your mood, your thoughts, your energy, and your ability to function in daily life. Depression touches every part of your life, but here’s what matters most: it is treatable.
The path forward isn’t always straightforward. Finding the right treatment often involves some trial and error, working closely with healthcare providers, and giving treatments time to work. But with proper diagnosis and treatment, the vast majority of people with depression find relief and reclaim their lives.
This can feel overwhelming when you’re in the thick of it. Depression has a way of making everything seem hopeless, including the idea that treatment could help. But that hopeless feeling is a symptom of the condition, not a reflection of reality. Treatment works, recovery happens, and you deserve support on this journey.
As Addiction Helpline America, we’ve helped thousands of individuals and families steer the complex landscape of major depression treatments, especially when addiction and mental health challenges intersect. We understand that finding the right help can feel impossible when you’re struggling, which is why we’re here to break down your options in clear, actionable terms.
Major depression treatments terms you need:
Understanding and Diagnosing Major Depression
Here’s something important to know right from the start: depression isn’t just feeling sad after a bad day or grieving a loss. Major depression is a medical condition that affects your brain chemistry, your body, and your entire life. It’s not a sign of weakness, and it’s certainly not something you can just “snap out of.”
The difference between normal sadness and clinical depression comes down to intensity, duration, and impact. We all feel down sometimes—that’s part of being human. But when that heavy feeling settles in and won’t leave, when it shows up practically every day for at least two weeks, and when it brings along other symptoms that interfere with your daily life, that’s when we’re talking about major depression.

Getting a proper diagnosis involves a careful evaluation by a mental health professional. They’ll conduct a psychiatric evaluation, asking detailed questions about what you’re experiencing, your personal and family history, and how symptoms are affecting your life. A physical exam and lab tests often come next—not because your doctor doesn’t believe you, but to rule out other medical conditions that can masquerade as depression.
Types of Depression and Related Mood Disorders
When most people say “depression,” they’re usually referring to Major Depressive Disorder (MDD). But depression actually comes in different forms, each with its own patterns and characteristics. The DSM-5 criteria help mental health professionals distinguish between these types.
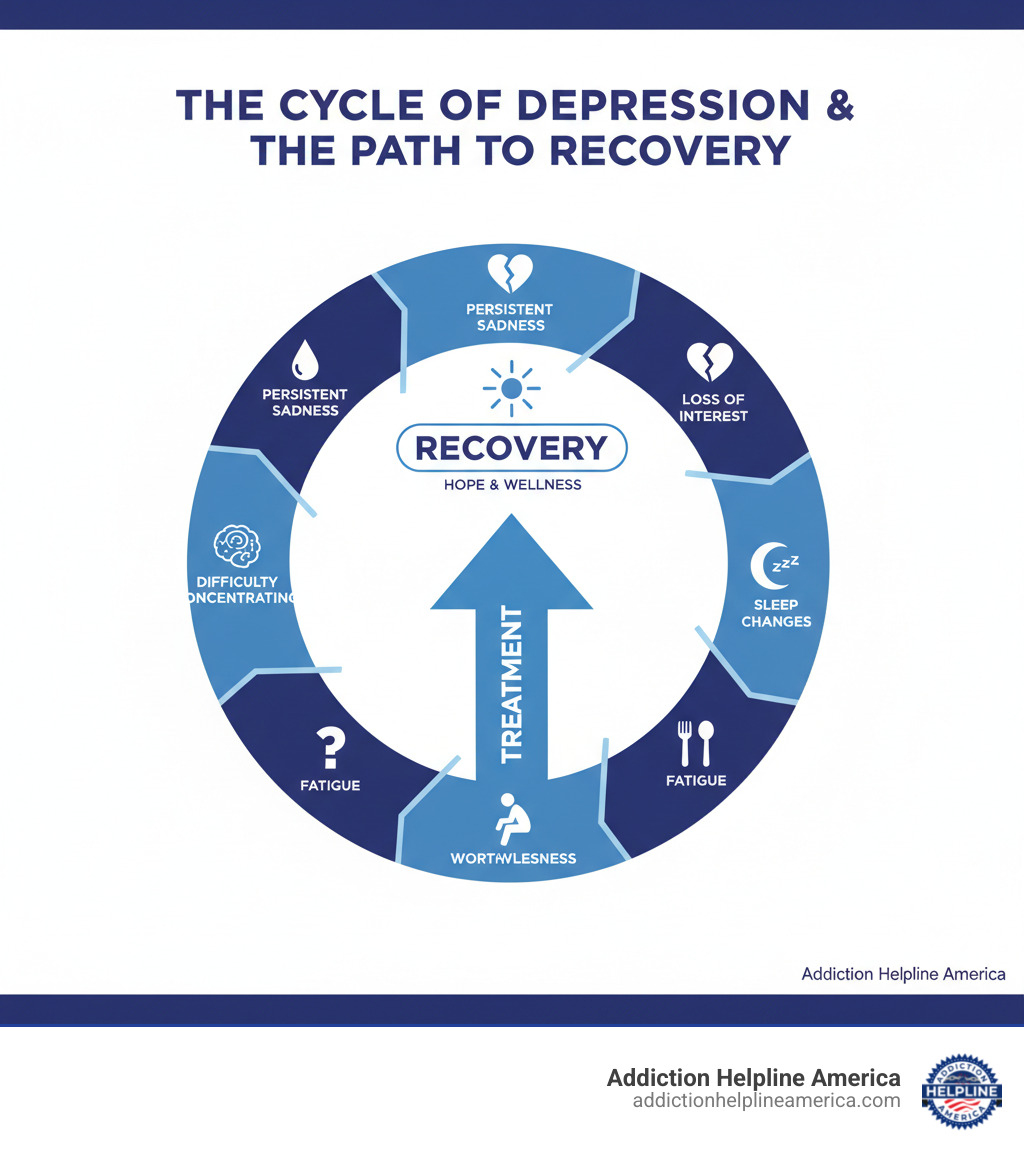
Major Depressive Disorder (MDD) is the main focus when we talk about major depression treatments. It involves significant symptoms—persistent sadness, loss of interest in life, changes in sleep and appetite—that last at least two weeks and seriously disrupt your ability to function.
Persistent Depressive Disorder, also called dysthymia, is like depression’s quieter cousin. The symptoms are generally milder than MDD, but they stick around for at least two years. It’s a chronic, low-grade sadness that becomes your unwelcome companion.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Postpartum depression affects new parents—yes, both mothers and fathers—after childbirth. This isn’t the “baby blues” that resolve in a few days. About 10% of women experience true postpartum depression, which can be severe and requires treatment.
Seasonal Affective Disorder (SAD) follows the calendar. Understanding how seasonal changes can impact mood helps explain why some people struggle more during winter months when natural light is scarce. This isn’t just “hating winter”—it’s a diagnosable pattern of depression that lifts when seasons change.
Psychotic depression represents severe depression that includes breaks from reality. Someone might experience hallucinations (seeing or hearing things that aren’t there) or delusions (fixed, false beliefs). This form requires immediate professional attention.
Here’s where diagnosis gets tricky: Bipolar Disorder includes depressive episodes that can look identical to major depression. The difference? People with bipolar disorder also experience periods of liftd mood called mania or hypomania. This distinction matters enormously because the treatments differ significantly. A thorough medical history helps rule out any history of mood elevation.
Recognizing the Signs and Symptoms Across Age Groups
Depression shows up as a cluster of changes that persist for at least two weeks. The most common signs include persistent sadness—that heavy, empty feeling that won’t lift—and anhedonia, which is the clinical term for losing interest in activities you once enjoyed. It’s not just being less excited about your hobbies; it’s a profound inability to feel pleasure at all.
Sleep changes go both ways. Some people with depression can’t sleep (insomnia), lying awake at 3 AM with racing thoughts. Others sleep too much (hypersomnia), unable to drag themselves out of bed even after 12 hours. Similarly, appetite or weight changes vary—you might lose interest in food entirely or find yourself eating compulsively. Significant, unintentional weight changes (up or down) often accompany depression.
Fatigue is nearly universal. You feel exhausted all the time, even when you’ve done nothing physical. Simple tasks feel overwhelming. Many people describe feelings of worthlessness or excessive guilt—a harsh inner voice constantly criticizing, blaming, telling you you’re not good enough.
Difficulty concentrating makes work, school, or even following a TV show feel impossible. Your mind feels foggy, decisions become paralyzing, and memory suffers. Most seriously, suicidal thoughts can emerge—recurring thoughts of death, wishing you wouldn’t wake up, or actively planning to end your life. These thoughts always require immediate professional help. If you or someone you know is in crisis, you can connect with people who can support you by calling or texting 988 anytime in the US and Canada, or by visiting the 988 Suicide & Crisis Lifeline.
Depression doesn’t look identical across all ages. Symptoms in teens often include irritability and anger more than obvious sadness. Adolescents might withdraw from friends, show declining school performance, or turn to substance use. Younger children might complain of physical illness, refuse to go to school, or become clingy with parents.
Symptoms in older adults frequently present as physical complaints—unexplained aches, pains, digestive issues, or fatigue—rather than emotional distress. Memory problems and confusion can be prominent, sometimes mistaken for dementia. This makes depression in elderly individuals particularly easy to miss or misdiagnose.
How Professionals Arrive at a Diagnosis
The diagnosis process starts with a comprehensive psychiatric evaluation. Your mental health professional will ask questions about your symptoms, when they started, how severe they are, and whether you’ve experienced them before. They’ll explore your family history, since depression tends to run in families, and discuss your personal circumstances, stressors, and support system.
A physical exam and lab tests come next. Why? Because several medical conditions can cause symptoms identical to depression. Thyroid tests are especially important—both overactive and underactive thyroid can trigger mood changes. Heart disease, Parkinson’s disease, certain cancers, and vitamin deficiencies can all masquerade as depression. Ruling out other conditions ensures we’re treating the right problem.
To confirm major depression, professionals look for at least five of the common symptoms present most of the day, nearly every day, for at least two weeks. Critically, these symptoms must cause significant distress or impair your ability to function at work, school, home, or in relationships.
Using diagnostic tools helps standardize assessment. The Patient Health Questionnaire (PHQ-9) is a widely-used self-assessment tool that asks nine questions about depressive symptoms. A score of 10 or higher suggests possible MDD and indicates the need for further evaluation. Many doctors use the PHQ-9 not just for diagnosis but also to track how well treatments are working over time.
The diagnostic process might feel exhausting when you’re already struggling, but it’s essential. Accurate diagnosis leads to effective treatment, and effective treatment leads to recovery. At Addiction Helpline America, we help people steer this process, connecting them with qualified professionals who can provide thorough evaluations and personalized treatment plans.
Primary Major Depression Treatments: Medication and Psychotherapy
Here’s something that gives us real hope: major depression treatments work incredibly well for most people. The most effective approach usually combines medication and psychotherapy, custom specifically to your situation. Think of it like this—we’re not looking for a one-size-fits-all solution. We’re looking for your solution.

When medication and therapy work together, they address depression from two powerful angles at once. Medication helps restore the chemical balance in your brain, while therapy gives you practical tools to manage your thoughts, feelings, and daily challenges. For moderate to severe depression, this combination therapy approach is often considered the first-line treatment, and research consistently shows it delivers better results than either treatment alone.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
The Role of Antidepressant Medications
Antidepressants aren’t “happy pills” that artificially change who you are. Instead, they work by helping restore your brain’s natural emotional balance through specific neurotransmitter activity. These neurotransmitters—chemical messengers in your brain—play a crucial role in regulating mood, and when they’re out of balance, depression can take hold.
The main neurotransmitters involved are serotonin (which helps regulate mood, sleep, and appetite), norepinephrine (which affects alertness and energy), and dopamine (which influences motivation and pleasure). Antidepressants typically work by increasing the availability of one or more of these chemicals in your brain, giving your mind the resources it needs to function properly again.
Finding the right medication can sometimes feel frustrating. We wish we could predict exactly which medication would work perfectly for you from day one, but the truth is, it often involves some trial and adjustment. Your doctor will consider your specific symptoms, any other medical conditions you have, potential side effects, and even your family history—if a close relative responded well to a particular antidepressant, there’s a decent chance you might too.
Genetic testing considerations are becoming more available as well. While still an emerging tool, these tests can sometimes offer helpful clues about how your body might metabolize certain medications, potentially helping us narrow down the options more quickly.
Here’s the part that requires patience: antidepressants need time to work. Most people start noticing some improvement within one to two weeks, but the full therapeutic effect typically takes 4 to 8 weeks to develop. This waiting period can feel endless when you’re struggling, but it’s a normal part of how these medications work. Your brain needs time to adjust to the chemical changes and establish new patterns. Keep taking your medication as prescribed, even if you don’t see immediate results, and stay in close contact with your healthcare provider about what you’re experiencing.
Psychotherapy: A Cornerstone of Major Depression Treatments
If medication helps restore your brain chemistry, therapy gives you the roadmap for navigating life differently. Psychotherapy—often called talk therapy—is just as important as medication in treating depression, and research shows it’s about as effective as antidepressants for many people. Even better, the benefits of therapy often last longer, potentially reducing your risk of relapse even after treatment ends.
Therapy isn’t just venting to someone who nods sympathetically (though having a compassionate listener certainly helps). It’s active work that helps you develop coping skills, identify and change unhelpful thinking patterns, and steer challenging life situations with new tools. You learn to recognize the warning signs when depression tries to creep back in, and you build strategies to push back against it.
The benefits of psychotherapy extend across many areas. Through therapy, you can adjust to current difficulties or crises in your life, identify and replace negative beliefs and behaviors that keep you stuck, explore how your relationships and past experiences shape your present, and develop healthy coping and problem-solving skills. You’ll work on regaining a sense of control and satisfaction in your life, set realistic goals that feel achievable, and learn effective ways to manage stress before it becomes overwhelming.
Several evidence-based therapy approaches have proven particularly effective for depression. Cognitive Behavioral Therapy (CBT) focuses on the connection between your thoughts, feelings, and behaviors. It helps you spot and challenge the negative thought patterns that fuel depression—things like “I’m worthless” or “Nothing will ever get better”—and replace them with more balanced, realistic thinking. CBT also helps you change behaviors that keep depression going, like isolating yourself or avoiding activities you used to enjoy.
Interpersonal Therapy (IPT) takes a different angle, focusing on your relationships and social circumstances. Depression doesn’t happen in a vacuum—it’s often connected to relationship problems, major life transitions, grief, or social isolation. IPT helps you improve communication skills, resolve conflicts, and build healthier relationship patterns that support your mental health.
Behavioral Activation is beautifully straightforward: it helps you start doing things again. When you’re depressed, you naturally withdraw and stop engaging in activities that used to bring you joy or satisfaction. This creates a vicious cycle—the less you do, the worse you feel, and the worse you feel, the less you do. Behavioral Activation breaks this cycle by helping you schedule and participate in positive, rewarding activities, even when you don’t feel like it at first. Over time, these activities start lifting your mood naturally.
Psychodynamic Therapy goes deeper, exploring unconscious thoughts, early life experiences, and patterns that might be contributing to your current struggles. It helps you develop greater self-awareness and understand how past experiences shape your present reactions, supporting the development of more adaptive ways of functioning.
Your therapist will work with you to determine which approach—or combination of approaches—makes the most sense for your unique situation.
Common Antidepressants and Potential Side Effects
Let’s break down the main classes of antidepressants you might encounter. Selective Serotonin Reuptake Inhibitors (SSRIs) are often prescribed first because they tend to have fewer side effects than older antidepressants. They work by increasing serotonin levels in your brain. Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs) target both serotonin and norepinephrine, which can be helpful if SSRIs alone don’t provide enough relief. Atypical Antidepressants work through various mechanisms and can be good options if the other classes don’t work well for you.
| Class | How They Work | Common Examples | Common Side Effects |
|---|---|---|---|
| SSRIs | Increase serotonin by blocking its reabsorption | Fluoxetine (Prozac), Sertraline (Zoloft), Escitalopram (Lexapro), Citalopram (Celexa), Paroxetine (Paxil) | Nausea, dry mouth, insomnia, sexual dysfunction, weight changes, drowsiness |
| SNRIs | Increase both serotonin and norepinephrine | Venlafaxine (Effexor), Duloxetine (Cymbalta), Desvenlafaxine (Pristiq) | Similar to SSRIs, plus increased blood pressure, sweating |
| Atypical Antidepressants | Various mechanisms (dopamine, norepinephrine, serotonin) | Bupropion (Wellbutrin), Mirtazapine (Remeron), Trazodone | Varies by medication; bupropion may cause anxiety or insomnia but less sexual dysfunction; mirtazapine may cause drowsiness and weight gain |
Most side effects are manageable and often decrease after the first few weeks as your body adjusts. If side effects become troublesome, don’t suffer in silence—talk to your doctor. Often, adjusting the dose or switching to a different medication can make a significant difference.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
There’s an important black box warning on all antidepressants regarding an increased risk of suicidal thoughts and behaviors in children, adolescents, and young adults (up to age 24), especially during the first few months of treatment or when doses are changed. This doesn’t mean antidepressants cause suicide—untreated depression itself carries significant suicide risk. It means close monitoring is essential, especially early in treatment. If you or someone you love is taking antidepressants, stay in close contact with your healthcare provider and report any worsening symptoms immediately.
Finally, never stop taking antidepressants abruptly without medical guidance. The risks of stopping suddenly can include uncomfortable withdrawal symptoms and a rapid return of depression symptoms. Your doctor will help you taper off gradually if and when the time comes to discontinue medication.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Discover Effective Major Depression Treatment Options & Support
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.















