Limited Availability: Treatment beds filling quickly. Call now for immediate placement – (844) 561-0606
Addiction doesn’t discriminate. It can affect people from all walks of life, including those over the age of 65 and individuals with disabilities. As America faces a growing addiction crisis among older adults, Medicare insurancehas become an essential tool in helping this population access life-saving addiction treatment services.
Medicare is a federally funded health insurance assistance program primarily for seniors and certain individuals with disabilities. But what many don’t realize is that Medicare offers robust coverage for substance use disorders (SUDs), behavioral health services, and co-occurring mental health conditions.
In this comprehensive guide, we’ll explore everything you need to know about Medicare and addiction treatment, including eligibility, coverage details, treatment options, and real-world statistics.

Medicare is a national health insurance programrun by the U.S. federal government. It was established in 1965 and now provides health coverage to more than 65 million Americans.
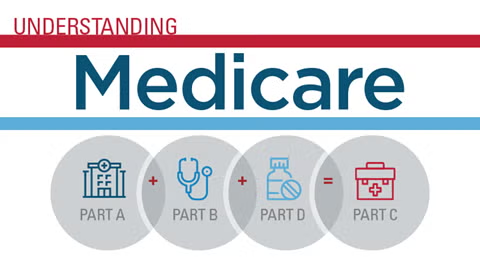
Medicare is divided into four parts, each covering specific aspects of care:
Part | What It Covers |
Part A | Inpatient hospital stays, skilled nursing care, hospice, and some home health care |
Part B | Outpatient care, doctor visits, preventive services, and mental health care |
Part C | Medicare Advantage (private insurance alternative combining A & B, sometimes D) |
Part D | Prescription drug coverage, including medications used in MAT |
Substance use among older adults is a rapidly growing public health concern.
These statistics highlight the critical role that Medicare plays in expanding access to addiction treatment and recovery support for older adults.
Medicare offers extensive coveragefor various forms of addiction treatment, including both inpatient and outpatient services. However, it’s important to understand how each part of Medicare contributes to overall care.
Note:Medicare Part A covers up to 190 days of psychiatric hospital carein a lifetime.
Part B also covers alcohol misuse screening and counselingfor adults who misuse alcohol but aren’t dependent.
These plans may operate as HMOs or PPOs, so your access to specific providers and facilities may depend on your network.
Yes. Medicare provides robust mental health coverage, recognizing that co-occurring disorders(mental illness + addiction) require integrated treatment.
Covered services include:
Partial hospitalization programs (PHPs)
Take the first step towards a brighter future! If you or a loved one is seeking support for substance abuse, we are here to help. Call us today and let our dedicated team guide you to the right treatment options. Your path to recovery starts now!
In most cases, Original Medicare (Parts A and B)covers out-of-state treatment if the facility is:
However, Medicare Advantage plans (Part C)may restrict treatment to in-network providers or local service areas. Always confirm with your plan before seeking treatment out of state.
The actual length of covered treatmentdepends on medical necessity, progress, and the specific Medicare plan.
Original Medicareis not an HMO or PPO. It allows you to visit any doctor or facility in the U.S. that accepts Medicare.
However, Medicare Advantage (Part C)plans may be structured as:
Choosing between Original Medicare and Medicare Advantage depends on your specific treatment needs and preferred provider network.
You can enroll in Medicare:
To check coverage or find a treatment center:
Reach out to Addiction Helpline Americaat (844) 561-0606
Keep documentation:Ensure your treatment is deemed “medically necessary” by a licensed provider.
Medicare can be a vital resource for older adults and individuals with disabilities seeking help for addiction. With access to inpatient and outpatient rehab, behavioral therapies, prescription medications, and mental health services, Medicare ensures that essential treatment is accessible to the people who need it most.
If you or a loved one are navigating addiction recovery and have Medicare, don’t wait. Reach out to licensed professionals who accept Medicare and start your journey toward a healthier, substance-free future today.
For personalized help and support, contact Addiction Helpline Americaat (844) 561-0606.
Yes.Medicare covers both inpatient and outpatient treatment for substance use disorders, including detox, therapy, medication-assisted treatment (MAT), and counseling. Coverage depends on the type of Medicare plan you have and the medical necessity of the treatment.
If you have Original Medicare (Parts A and B), you can receive care at any Medicare-approved facility. If you’re enrolled in a Medicare Advantage plan (Part C), your options may be limited to in-network providers, so it’s important to verify coverage with your plan.
Yes. Medicare Part Dand most Medicare Advantage plans cover prescription medicationsused in addiction treatment, including Suboxone, Naltrexone, and Methadone (when dispensed at a certified clinic).
Medicare Part A covers up to 90 daysof inpatient care per benefit period, plus 60 lifetime reserve days. Outpatient therapy under Part B has no fixed limitas long as it is medically necessary.
Yes. Medicare provides comprehensive mental health coverage, including therapy, psychiatric evaluations, and medicationsfor conditions like depression, anxiety, and bipolar disorder. This is essential for treating co-occurring disordersalongside addiction.
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.
For anyone seeking help for addiction for themselves or a loved one calls to Addiction Helpline America are completely confidential and available 24/7.
Please note: any treatment center listed on our site that receives calls is a paid advertiser.
Calls to a specific treatment center’s listing will be connected directly to that center.
Calls to our general helpline will be answered by treatment providers, all of whom are paid advertisers.
By calling the helpline, you agree to our terms and conditions. These calls are free of charge and carry no obligation to enter treatment. Neither Sober Steps nor anyone answering your call receives a commission or fee based on your choice of treatment provider.
If you’d like to explore additional treatment options or connect with a specific rehab center, you can browse our top-rated listings, visit our homepage, or call us at (844) 561-0606. You may also contact us for further assistance.
Calls to any general helpline will be answered or returned by one of the treatment providers listed, each of which is a paid advertiser:
Our helpline is available 24 hours a day, 7 days a week at no cost to you and with no obligation for you to enter into treatment. We are committed to providing support and guidance whenever you need it.
In some cases, Addiction Helpline America charges our verified partner a modest cost per call. This fee helps us cover the costs of building and maintaining our website, ensuring that we can continue to offer this valuable service to those in need.