
When we talk about effective drug and treatment plans, we start from one crucial place: addiction is a treatable brain condition, not a moral weakness. Recovery is all about healing the brain’s hijacked reward pathways. It’s a journey that demands professional guidance, real compassion, and strategies that are proven to work.
Understanding the Path to Addiction and Recovery
Now, imagine an addictive substance entering the picture. It’s not a gentle stream; it’s a massive, destructive flood. It carves a brand-new, deep riverbed right through the landscape, bypassing all the natural routes. This new pathway is so powerful that the brain starts to see it as the only path that matters.
How a New Pathway Forms
The brain is a fast learner. It quickly figures out this new “river” is a shortcut to an overwhelming sense of reward. Before long, the original, gentle streams start to dry up because they simply can’t compete. This is why someone struggling with addiction might lose interest in hobbies or relationships that once brought them joy—their entire reward geography has been forcefully remapped.
The core challenge in recovery isn’t just stopping the substance. It’s about rerouting the brain’s reward signals back to their healthy, natural channels, which takes conscious effort and a strong support system.
This rewiring is the very essence of chemical dependency. The brain isn’t just chasing a high anymore; it’s trying to function inside this new, altered landscape. The substance becomes essential just to feel “normal,” creating a powerful cycle that’s nearly impossible to break alone. Grasping this process is the first step toward understanding why a structured drug and treatment program is so critical. You can get a deeper look at how addiction changes the brain in our guide on what drug addiction is.
The Stages of Developing Dependency
This hijacking of the brain doesn’t happen all at once. It’s a gradual process that unfolds in stages, with each step carving that unhealthy riverbed a little deeper.
- Initial Use and Experimentation: This is the first time the “flood” hits the landscape, often sparked by curiosity, peer pressure, or a desire to escape.
- Regular Use: The substance becomes a more consistent presence. The new riverbed deepens, and the brain starts to favor it as the main route for feeling good.
- Dependency and Addiction: At this point, the brain has come to rely on the substance just to function. The old, healthy pathways are all but abandoned, and trying to stop triggers intense withdrawal as the brain panics without its new primary reward source.
Understanding this progression is key. It shows that recovery isn’t a matter of willpower; it’s about physically and chemically rebuilding the brain’s natural landscape. And the good news is, with the right therapeutic tools and support, it is absolutely possible to carve new, healthy pathways and find lasting recovery.
Common Substances and Their Impact
To find the right kind of drug and treatment, you first have to understand the substance you’re dealing with. Not all drugs are created equal; their effects on the brain, body, and spirit can be wildly different. Think of it like this: some substances are like a wildfire, burning through your life with terrifying speed, while others are more like a slow, creeping flood, causing damage so gradually you might not notice until it’s too late.
Because each substance causes its own unique kind of harm, a one-size-fits-all approach to recovery just doesn’t work. The treatment has to be tailored to the specific drug and the person using it.
This overview gives you a snapshot of different drug classifications, how they’re used, and the typical timelines for initial treatment.
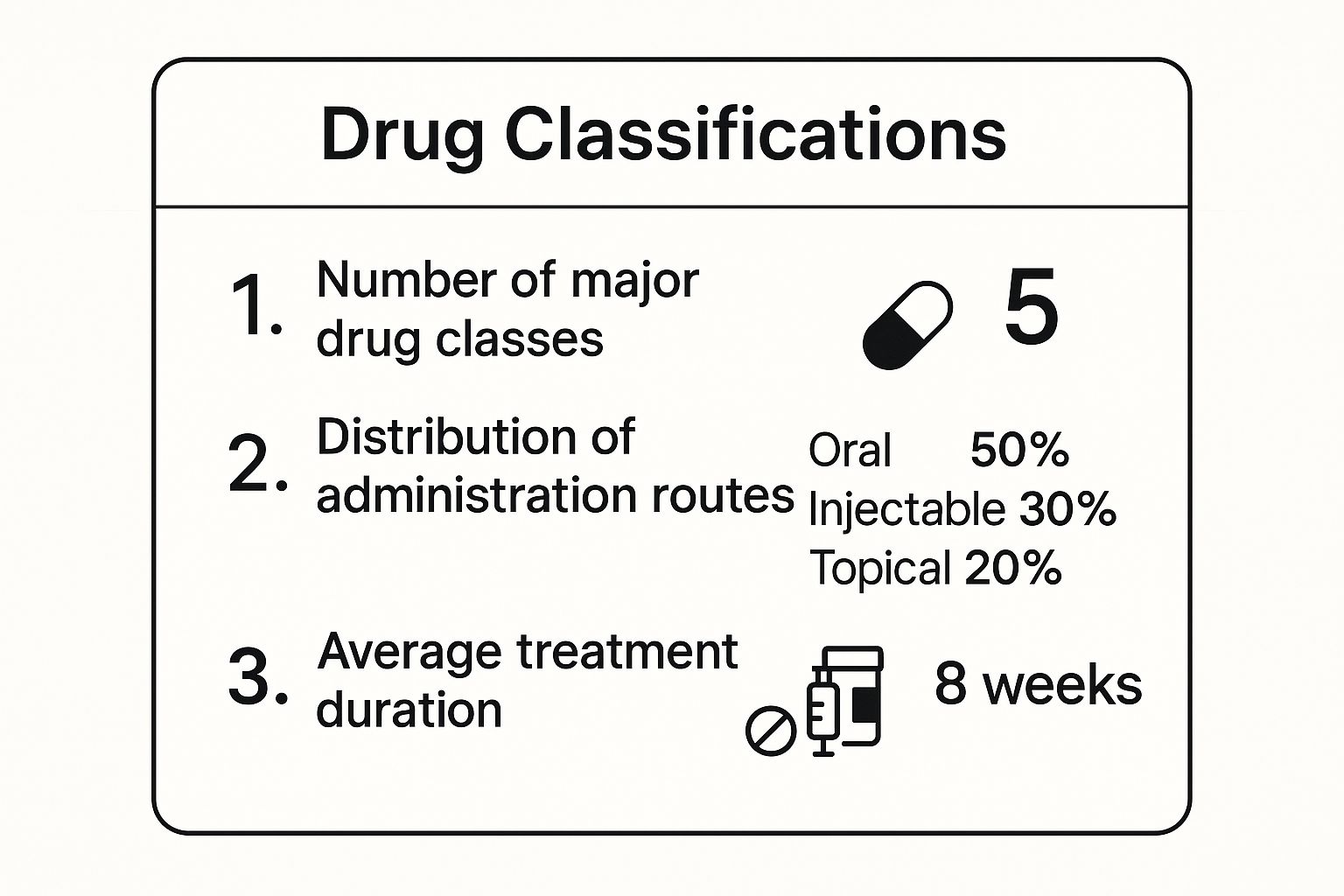
As you can see, the diversity in both substances and treatment paths makes specialized, professional care absolutely essential.
Depressants: Slowing Everything Down
Depressants are a class of drugs that slow down your central nervous system. This doesn’t mean they make you feel emotionally depressed—instead, they reduce brain activity, slow your breathing, and lower your heart rate. The most common examples are opioids (like heroin and fentanyl), benzodiazepines (like Xanax and Valium), and, of course, alcohol.
Imagine your brain is a bustling city. Depressants turn down the lights and quiet the noise, creating a temporary sense of calm and euphoria. But this forced relaxation is incredibly dangerous.
The long-term risks are devastating, including deep physical dependence, respiratory failure, and fatal overdose. The opioid crisis is a tragic example of this, with more than 75% of drug overdose deaths in 2021 involving an opioid. To understand more about the powerful grip of these substances, check out our guide on the most addictive drugs.
Stimulants: Speeding Everything Up
On the opposite end of the spectrum, stimulants send the central nervous system into hyperdrive. We’re talking about substances like cocaine, methamphetamine, and prescription drugs like Adderall. They flood the brain, creating an intense rush of energy, focus, and alertness.
If depressants are a dimmer switch, stimulants are like flipping a power surge through the grid. The user feels on top of the world, full of confidence and euphoria. But what goes up must come crashing down.
These drugs force the brain to release massive, unnatural amounts of its “feel-good” chemicals like dopamine. Over time, the brain’s natural ability to produce these chemicals is shot, leading to a profound inability to feel pleasure, crippling depression, and exhaustion without the drug.
Long-term use can wreck the cardiovascular system, leading to heart attacks and strokes. It can also trigger severe psychological issues, from deep-seated paranoia to full-blown psychosis. This vicious cycle of soaring highs and crushing lows is what makes stimulants so addictive and so hard to walk away from alone.
Hallucinogens: Distorting Reality
Hallucinogens do exactly what their name implies: they profoundly alter a person’s perception of reality. This group includes drugs like LSD, psilocybin (magic mushrooms), and PCP. They work by scrambling the communication lines between the brain’s chemical systems.
Unlike other drugs, their effects are notoriously unpredictable. An experience, or “trip,” can feel enlightening or deeply terrifying. A user might see, hear, or feel things that aren’t there, completely losing touch with their surroundings.
While many hallucinogens don’t create the same kind of physical dependence as opioids, the psychological risks are huge. A “bad trip” can lead to dangerous behavior and lasting trauma. Users can also experience flashbacks or develop persistent psychosis, underscoring the need for expert drug and treatment even for substances not typically seen as “addictive” in the classic sense.
To make this easier to digest, here’s a quick summary of the major drug classes we’ve covered.
Overview of Common Drug Classes and Effects
| Drug Class | Examples | Primary Effects on the Brain | Long-Term Health Risks |
|---|---|---|---|
| Depressants | Alcohol, Opioids (Heroin, Fentanyl), Benzodiazepines (Xanax) | Slows down central nervous system activity, creating sedation and euphoria. | Severe physical dependence, respiratory failure, liver damage, overdose. |
| Stimulants | Cocaine, Methamphetamine, Adderall, Ritalin | Speeds up the central nervous system, increasing alertness, energy, and dopamine levels. | Cardiovascular damage (heart attack, stroke), severe depression, psychosis, malnutrition. |
| Hallucinogens | LSD, Psilocybin (Mushrooms), PCP, Ketamine | Alters perception, mood, and thought; disrupts serotonin communication pathways. | Flashbacks (HPPD), persistent psychosis, potential for psychological trauma. |
This table is just a starting point. Each substance has its own profile, and the way it affects an individual can vary based on genetics, mental health, and many other factors.
A Look at Evidence-Based Treatment Methods
Think of it like a master mechanic’s toolbox. You wouldn’t use a wrench to fix a flat tire or a screwdriver to change the oil. A professional selects the right tool for the specific job. In addiction treatment, therapists combine different approaches to address each person’s unique challenges, helping them develop healthy coping skills and build a new life from the ground up.
A big piece of this puzzle is learning to recognize and rewire the harmful thought patterns that keep the cycle of substance use going. This is where behavioral therapies are incredibly powerful.
Cognitive Behavioral Therapy
One of the most trusted and effective tools in the box is Cognitive Behavioral Therapy, or CBT. It’s built on a straightforward but profound idea: your thoughts, feelings, and actions are all linked. If you can change your thinking, you can change your behavior.
Imagine that addiction has installed a faulty GPS in your mind, constantly rerouting you toward destructive habits. CBT helps you take back control and recalibrate that system. A therapist will work with you to pinpoint your specific triggers—the people, places, emotions, or situations that spark cravings.
From there, you learn to challenge the automatic thoughts that pop up. For instance, the thought “I’ve had a horrible day; I need a drink to relax” can be intercepted and reframed to, “This was a tough day, and drinking will only make tomorrow worse. I can call a friend or go for a walk instead.” It’s about creating new, healthier pathways in the brain.
Motivational Interviewing
Sometimes the biggest obstacle isn’t the substance itself, but the deep internal conflict about whether to change. That’s where Motivational Interviewing (MI) comes in. Rather than lecturing someone on why they have to change, MI is a collaborative partnership.
The therapist acts as a guide, asking thoughtful questions that help the person find their own motivation. It’s a deeply respectful process that puts you in the driver’s seat of your recovery. This approach helps build the genuine, internal resolve needed to truly commit to a drug and treatment plan.
The core idea behind Motivational Interviewing is that lasting change comes from within. The therapist’s role is to help unlock and strengthen a person’s intrinsic motivation to build a better, healthier life.
This client-centered method is especially helpful in the early stages, when someone might feel uncertain or ambivalent about taking the first step.
Dialectical Behavior Therapy
Originally created to help people with borderline personality disorder, Dialectical Behavior Therapy (DBT) has become a game-changer for anyone struggling with overwhelming emotions and self-destructive behaviors—two common features of addiction. DBT teaches four essential skills:
- Mindfulness: Learning how to stay grounded in the present moment without judgment.
- Distress Tolerance: Finding ways to get through painful situations without turning to substances.
- Emotion Regulation: Gaining control over intense feelings instead of letting them control you.
- Interpersonal Effectiveness: Learning how to communicate your needs and set healthy boundaries with others.
These are just a few of the many powerful tools available. You can discover more in our guide to the different types of addiction therapy. The best recovery plans often blend elements from several therapies to create a program tailored to the whole person—mind, body, and spirit.
The field of addiction treatment is always evolving. Excitingly, new technologies are accelerating progress. Experts estimate that by 2025, 30% of new drugs could be discovered with the help of artificial intelligence, which promises to usher in an era of more personalized and effective medicines.
The Role of Medication in the Recovery Process
While therapy is absolutely critical for healing the psychological side of addiction, some substances hijack the brain so intensely that counseling alone can feel like an uphill battle. This is especially true for opioid and alcohol addiction, where a comprehensive drug and treatment plan often needs another powerful tool: Medication-Assisted Treatment (MAT).
MAT is a science-backed approach that uses specific, FDA-approved medications to help rebalance brain chemistry, ease the agony of withdrawal, and shut down overwhelming cravings.
Think of it like this: if addiction is a house on fire, therapy is the long-term work of learning fire safety and fireproofing the structure. MAT is the fire extinguisher. It puts out the immediate blaze so you have the safety and stability to actually do that deeper, more permanent work. It creates a window of calm, allowing you to fully engage in counseling and build a real foundation for your recovery.
How Medications Pave the Way for Healing
The medications used in MAT aren’t a “cure” for addiction, but they are incredibly effective at managing the physical grip it has on the body. They work in a few different ways to get those hijacked brain circuits back on track. For many, this medical support is a complete game-changer, particularly in the fragile, early days of recovery when relapse risk is at its highest.
Here are a few of the most trusted and effective medications:
- Buprenorphine (Suboxone): This medication gently activates the brain’s opioid receptors—just enough to stop cravings and withdrawal, but without producing a dangerous high. It’s a way of stabilizing the brain so the real healing can start.
- Naltrexone (Vivitrol): This one works differently. It completely blocks the euphoric effects of opioids and alcohol. If someone relapses while on Naltrexone, they simply won’t feel the “reward,” which helps short-circuit the entire cycle of addiction.
- Methadone: As a long-acting opioid agonist, Methadone has been a cornerstone of treatment for decades. It effectively reduces cravings and withdrawal and must be provided through a specialized clinic.
This kind of biological support is what allows therapies like CBT to take root and flourish. Our guide digs deeper into what Medication-Assisted Treatment is and how it fits into a complete recovery plan.
One of the most damaging myths about MAT is that it’s just “swapping one drug for another.” This couldn’t be further from the truth. MAT involves using prescribed, FDA-approved medications under close medical supervision to treat a diagnosed medical condition—no different than a person with diabetes using insulin.
The pharmaceutical world is always working on solutions to major health crises. To put it in perspective, in 2024, a company like Merck & Co. brought in roughly $64.17 billion in revenue, with its cancer drug, Keytruda, making up about 46% of that. This drive to create life-changing medicines is what fuels the development of better treatments for complex diseases, including addiction. You can learn more about the leading pharmaceutical companies of 2025 and their work.
An Integrated Approach to Healing
It’s crucial to remember that medication is only one piece of the puzzle. The most successful drug and treatment programs always combine MAT with consistent counseling and behavioral therapies.
This integrated approach is designed to treat the whole person. It addresses the physical dependency with medication while simultaneously healing the underlying emotional and psychological drivers of the addiction. This combination gives you the power to not only manage physical symptoms but to build new coping skills, mend relationships, and create a truly meaningful life, free from substance use.
Navigating the Different Levels of Care
Recovery from addiction isn’t a one-and-done event. It’s a journey, and like any journey, it has different stages that require different kinds of support. A successful drug and treatment plan is all about meeting you where you are right now, providing the right intensity of care at the right time. This is what we call the continuum of care—a flexible path designed to guide you from a place of crisis toward lasting stability.
I like to use the analogy of learning to ride a bike. You don’t just hop on and pedal away. You start with training wheels for maximum support, then maybe a parent holds the back of the seat, and eventually, you’re off on your own, knowing help is still there if you wobble. Addiction treatment follows a similar path, gradually stepping down the level of support as you gain confidence and build your own recovery skills.
Medical Detox: The First Step
For most people, the very first stop on this journey is medical detoxification. This is the critical, foundational phase where the body is safely cleansed of substances under the watchful eye of medical professionals. Think of this as putting the training wheels on the bike—it creates the stability you need to even think about moving forward.
Withdrawal isn’t just unpleasant; depending on the substance, it can be downright dangerous. A professional detox program is designed to manage these symptoms with medication and 24/7 care, ensuring you are safe and as comfortable as possible. It’s the necessary groundwork for all the real recovery work that comes next.
Residential and Outpatient Programs
With detox complete, it’s time to start the deeper work. The “right” program depends entirely on your unique situation, and choosing the appropriate level of care is a major decision.
- Inpatient or Residential Care: This is the most immersive option, offering round-the-clock support in a highly structured, sober environment. By removing you from the people, places, and things that trigger substance use, it allows you to focus 100% on getting well. It’s like having someone holding onto the bike, offering constant guidance.
- Partial Hospitalization Program (PHP): A step down from residential, a PHP feels a bit like a full-time job. You attend treatment for several hours a day, five to seven days a week, but you can live at home or in a sober living facility. It provides intensive support while reintroducing a bit of independence.
- Intensive Outpatient Program (IOP): This level offers even more flexibility, usually involving a few hours of therapy on several days of the week. An IOP is perfect for people transitioning back into their daily lives who still need a solid, consistent support structure. This is like letting go of the bike but running alongside, ready to catch you if you stumble.
Understanding which of these is the best fit is key. For a more detailed breakdown, check out our guide on inpatient vs. outpatient rehab.
The whole point of stepping down through these levels of care is to gradually hand back responsibility and freedom, reinforcing the new coping skills you’ve learned along the way. Each stage is a deliberate step toward a strong, independent recovery.
Aftercare: The Key to Long-Term Success
Eventually, you’re riding the bike all on your own. Aftercare is the plan that keeps you balanced when you hit the inevitable bumps in the road. It’s not a formal program so much as a personalized strategy to protect the incredible progress you’ve made.
This final, crucial stage can look different for everyone. It might include ongoing individual therapy, joining support groups like Alcoholics Anonymous (AA) or Narcotics Anonymous (NA), or simply staying connected to a strong sober community. Just as a cyclist does regular maintenance on their bike to keep it in top shape, aftercare is the ongoing “tune-up” that keeps your recovery strong and helps prevent relapse.
Finding Your Way to the Right Help
Deciding to seek help for addiction can feel like staring up at a mountain you’re not sure how to climb. It’s a huge, intimidating step, but breaking it down makes the journey manageable. The very first move is simply recognizing when it’s time to ask for professional support.
So, when is that time? It’s often the hardest question to answer. A clear sign is when substance use starts causing problems in your life—whether with your health, your job, your finances, or your relationships. You might have tried to quit on your own and couldn’t, or maybe you notice you need more of the substance to feel the same effects. These aren’t signs of failure or a lack of willpower; they’re symptoms of a health condition that needs professional care, just like any other illness.
Making the Call: What to Ask a Helpline
Picking up the phone is a courageous move. Remember, national helplines are staffed by trained people who understand what you’re going through. Their job is to listen without judgment and guide you toward the resources that can actually help.
Think of the person on the other end of the line as a guide. They’re there to hear your story and help you map out the safest, most effective next step. You’re always in control of the conversation.
To make that first call count, it helps to go in with a few questions. This isn’t just about finding any help; it’s about finding the right help for you. Having a list ready can make you feel more confident and ensure you’re connecting with a quality facility.
Here are a few essential things to ask:
- “What accreditations do you have?” You want to hear names like The Joint Commission or CARF. These are stamps of approval that show the facility meets high standards for care.
- “What’s your approach to treatment?” Ask if they use evidence-based methods like Cognitive Behavioral Therapy (CBT) or Medication-Assisted Treatment (MAT). Their philosophy should feel like a good fit.
- “Do you provide a medically supervised detox?” This is non-negotiable for safely getting through withdrawal from substances like alcohol, benzodiazepines, or opioids.
- “How do you address co-occurring disorders?” Addiction often goes hand-in-hand with anxiety, depression, or trauma. A good program will treat both at the same time.
- “Can you tell me about your staff’s qualifications?” You want to know that the doctors, therapists, and other clinical staff are licensed and experienced.
- “Do you work with my insurance?” Get the financial details sorted out early. Ask them to help you verify your insurance coverage so there are no surprises.
This first call is your chance to interview potential partners for your recovery. By asking smart questions, you take control of the process and can feel good about the path you choose.
Frequently Asked Questions About Addiction and Recovery
When you’re facing addiction, whether it’s your own or a loved one’s, questions and uncertainty are completely normal. Getting clear answers is the first step toward finding a path forward. Let’s walk through some of the things people most often ask.
How Long Does Treatment Take?
This is probably the number one question we hear, and the honest answer is: it’s different for everyone. There’s no magic number or one-size-fits-all timeline for recovery.
The right duration really depends on individual factors like:
- The specific substance involved
- How long the addiction has been going on
- Whether there are other mental health challenges to address, like anxiety or depression
You’ve probably heard of the 28-day rehab model. While these shorter programs can be a great starting point, they are often just that—a start. Research from the National Institute on Drug Abuse strongly suggests that programs lasting less than 90 days may not be as effective for long-term success.
It helps to think of recovery as a healing process. It took time for the substance to change the brain’s chemistry, so it naturally takes time to build new, healthier neural pathways. The goal isn’t to rush through it, but to move at a pace that allows for real, lasting change.
Is Addiction Something You Can Actually Cure?
Addiction is best understood as a chronic condition, not unlike diabetes or high blood pressure. Just as you can’t “cure” diabetes, you can’t cure addiction with a one-and-done treatment. But it can be managed incredibly effectively, allowing people to live full, vibrant lives.
The goal of treatment isn’t a “cure” in the traditional sense. Instead, the aim is long-term remission, where the symptoms of addiction are managed, and a person can thrive in their health, work, and relationships.
Shifting your perspective from “cure” to “management” can be empowering. It moves the focus away from the idea of a single battle to be won or lost and toward building a sustainable lifestyle of wellness and support.
What’s the Real Success Rate for Treatment?
Defining a “success rate” for addiction treatment is tricky because success itself is personal. While staying sober is a major goal, it’s far from the only measure of progress.
Success is also:
- Rebuilding damaged relationships with family and friends
- Feeling physically and mentally healthier
- Finding stability in work or school
- Rediscovering a sense of purpose and joy
Many people worry about relapse, but it’s important to know that it’s a common part of the recovery journey—not a sign that treatment has failed. Statistics show that relapse rates for addiction are between 40% and 60%, which is very similar to rates for other chronic illnesses like asthma.
When a relapse happens, it simply means the treatment plan needs to be tweaked. The best drug and treatment programs aren’t just about preventing relapse; they’re about giving you the skills to manage it and get back on track quickly if it occurs.
If these questions have been on your mind, please know you aren’t the only one asking them. The most crucial step you can take is the first one: reaching out for help. The caring and professional team at Addiction Helpline America is here 24/7 to offer a confidential ear and connect you with the right support. Start your journey toward a healthier life by contacting us today.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.












