Understanding Borderline Personality Disorder and the Path to Recovery
Borderline personality disorder therapies offer proven pathways to recovery for individuals experiencing intense emotional pain, unstable relationships, and impulsive behaviors. While BPD was once misunderstood, we now know it is highly treatable.
Evidence-based therapies developed specifically for BPD include:
- Dialectical Behavior Therapy (DBT)
- Mentalization-Based Therapy (MBT)
- Schema Therapy (ST)
- Transference-Focused Psychotherapy (TFP)
People with BPD experience extreme emotional pain, a rollercoaster of relationships, and chronic feelings of emptiness. However, the prognosis is remarkably positive for those who receive proper treatment. Research shows 91% of people with BPD achieve remission after 10 years of treatment, and 99% after 16 years. The journey isn’t quick, but it is possible.
At Addiction Helpline America, we understand the challenges of BPD, especially when it co-occurs with substance use disorders (affecting 50-66% of individuals). Our team connects people with specialized borderline personality disorder therapies that address both mental health and addiction. We’re here to guide you toward compassionate, evidence-based care.
Terms related to borderline personality disorder therapies:
Primary Evidence-Based Borderline Personality Disorder Therapies
Psychotherapy, or talk therapy, is the cornerstone of BPD treatment. Unlike conditions where medication is primary, borderline personality disorder therapies use structured, evidence-based approaches to address core symptoms. The goal is to gain control over intense emotions, build healthier relationships, and create a life worth living. Several proven therapies exist, and finding the right personal fit is key.
Dialectical Behavior Therapy (DBT): The Gold Standard
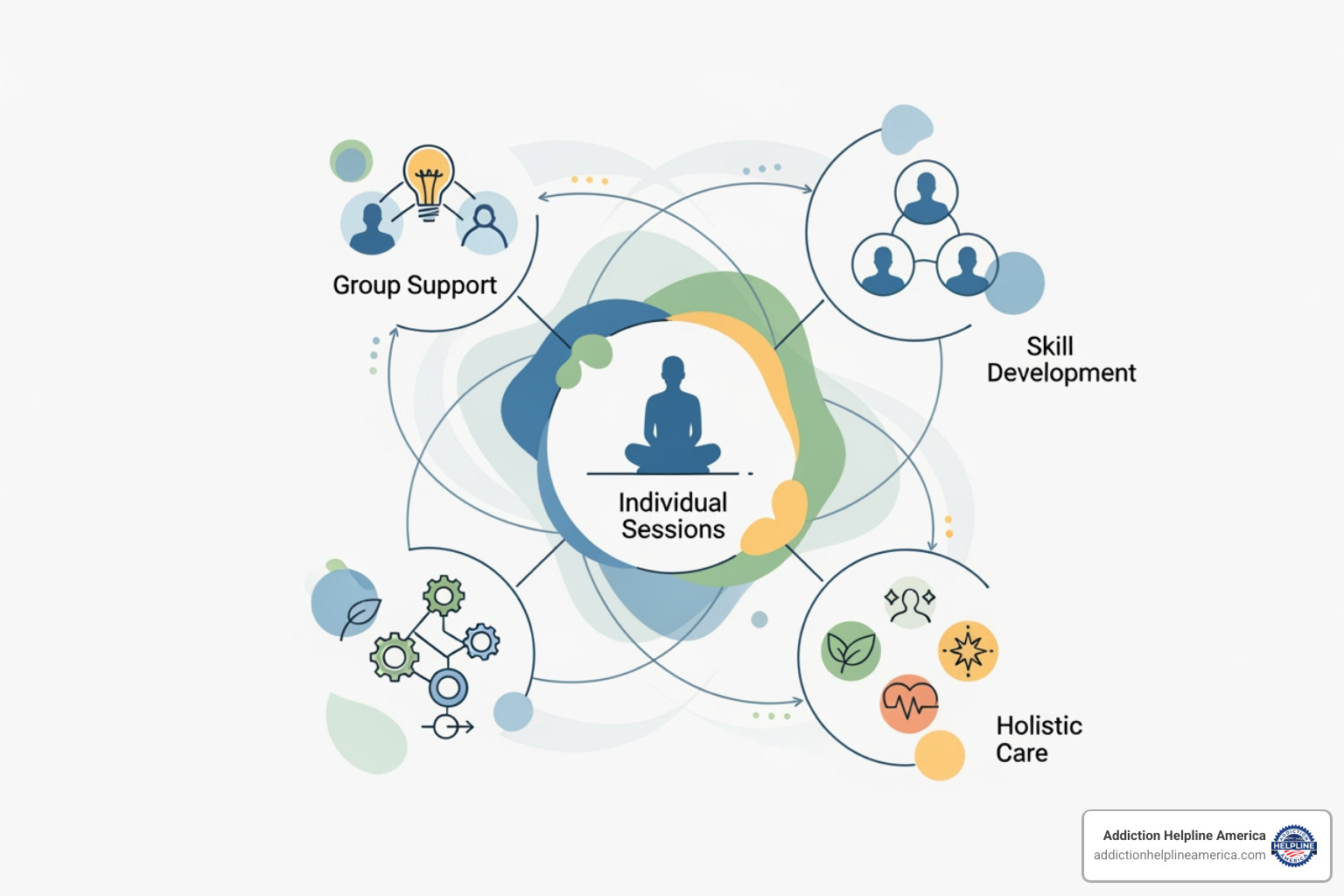
DBT is the most researched BPD treatment and is considered the gold standard. Developed by Dr. Marsha Linehan, DBT is an empirically supported therapy for BPD. It centers on “dialectics”—balancing acceptance of your emotional pain with learning skills for change. This comprehensive therapy teaches four essential skills: mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness. DBT typically involves individual therapy, group skills training, and phone coaching to help you apply these skills in daily life, reducing self-harm and improving stability.
Mentalization-Based Therapy (MBT)
Mentalization-Based Therapy focuses on improving your ability to “mentalize”—to understand the thoughts, feelings, and intentions behind your own and others’ behavior. When intense emotions take over, this ability can shut down, leading to misunderstandings and conflict. MBT helps you step back from overwhelming emotions to reflect on what’s happening, leading to improved self-awareness and better relationships. Research shows that MBT can be as effective as other therapies in treating BPD.
Schema Therapy (ST)
Schema Therapy explores how unmet childhood needs create “early maladaptive schemas”—deeply ingrained negative patterns about yourself and the world. These schemas act like scripts that drive your reactions. ST helps you connect current struggles to past experiences and heal old wounds through cognitive, behavioral, and experiential techniques. A key component is “limited reparenting,” where the therapist provides the validation and security that was missing in early life. Pilot studies on group ST show promise, especially for those with a history of trauma.
Transference-Focused Psychotherapy (TFP)
Transference-Focused Psychotherapy is a psychodynamic approach that uses the relationship between you and your therapist as the primary tool for change. It focuses on “transference”—the unconscious projection of past relationship patterns onto the therapist. By identifying and exploring these patterns as they emerge in sessions, TFP helps you integrate “split” views of yourself and others (all good or all bad). This process leads to a more stable sense of identity and more balanced relationships.
At Addiction Helpline America, our team can help you understand which of these borderline personality disorder therapies might be the best fit and connect you with qualified specialists.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Other and Adjunctive Therapeutic Approaches
The four primary borderline personality disorder therapies form the foundation of treatment, but a comprehensive approach often includes additional support. These adjunctive modalities can help address specific symptoms, build practical skills, and create a robust support network for recovery.

At Addiction Helpline America, we connect clients with comprehensive programs that combine multiple therapeutic approaches. Explore our Mental Health Resources at Addiction Helpline America for more information.
Skills-Based Group Programs for BPD
Skills-based group programs like Systems Training for Emotional Predictability and Problem Solving (STEPPS) offer a structured environment to learn coping skills alongside peers. STEPPS helps individuals manage emotions and improve problem-solving, and it actively involves your support network (family and friends) in the process. A comparison of group skills programs and DBT effectiveness found that both significantly reduced BPD symptoms, making programs like STEPPS a valuable component of a treatment plan.
The Role of Group Therapy and Creative Therapies
Group therapy provides a unique space to practice interpersonal skills in real time, reducing the shame and isolation that often accompany BPD. Hearing from others with similar struggles is powerfully validating. For times when words fail, creative therapies like art, music, and drama therapy offer non-verbal outlets for expression. They allow you to process complex feelings and trauma without having to articulate every detail, serving as a powerful complement to core psychotherapy.
The Role of Medication in BPD Treatment
It’s important to know there are no FDA-approved medications specifically for BPD. Medication is an adjunctive—or supporting—treatment, not a standalone solution. It should be time-limited and symptom-focused, targeting issues like severe mood swings, anxiety, or impulsivity that interfere with your ability to engage in psychotherapy. Mood stabilizers, antipsychotics, or antidepressants may be used, but they do not treat the core issues of BPD. The American Psychiatric Association guidelines recommend a careful approach, always combining medication with therapy.
If you’re considering medication, we can help you understand your options. Learn about medication and inpatient rehab options at Addiction Helpline America.
Diagnosis, Prognosis, and Choosing the Right Therapy
Understanding the BPD diagnosis, treatment options, and long-term outlook empowers you to make informed decisions about your care. This knowledge puts you in the driver’s seat of your recovery journey.

How BPD is Diagnosed and Its Challenges
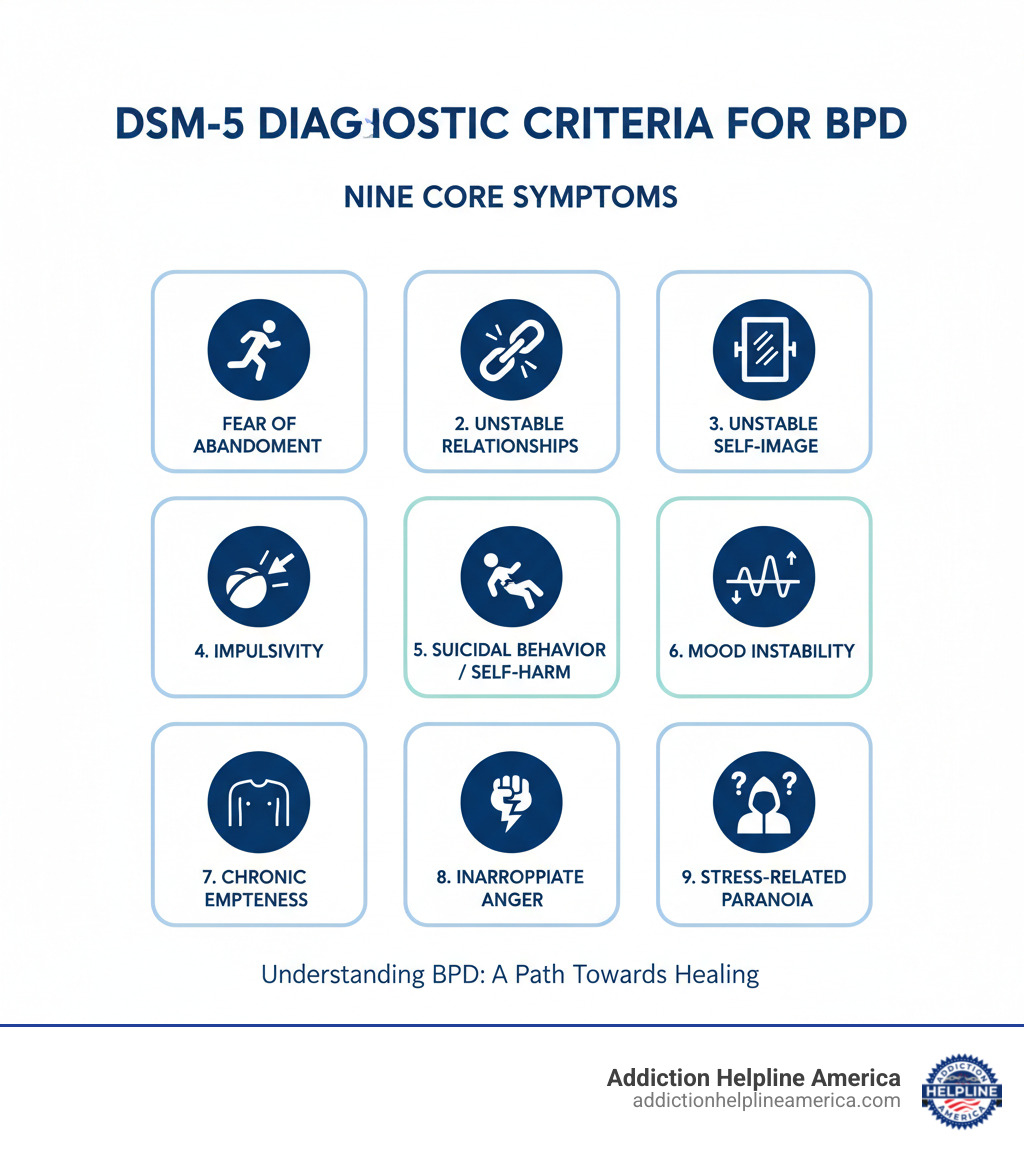
BPD is diagnosed through a thorough clinical interview with a mental health professional. There is no blood test; diagnosis is based on the DSM-5, which requires a person to meet at least five of nine specific criteria related to emotional instability, relationship patterns, self-image, and impulsivity. Diagnosis can be challenging due to significant symptom overlap with other conditions like PTSD, bipolar disorder, and depression, which can lead to misdiagnosis. Stigma and outdated beliefs have also been barriers, though this is improving as research highlights BPD’s treatability. Furthermore, recent research shows it affects men and women equally, challenging old gender biases in diagnosis.
Choosing Among Borderline Personality Disorder Therapies
There is no single “best” therapy for everyone with BPD. The right choice depends on your specific symptoms, co-occurring conditions, and which approach resonates with you. The relationship you build with your therapist is also a critical factor.
| Therapy | Primary Focus | Key Techniques | Typical Structure | Best Suited For |
|---|---|---|---|---|
| DBT | Balancing acceptance and change; managing intense emotions | Mindfulness, distress tolerance, emotion regulation, interpersonal effectiveness | Individual therapy, group skills training, phone coaching | High emotional reactivity, self-harm, suicidal thoughts, impulsivity |
| MBT | Understanding your own and others’ mental states | Reflection on thoughts and feelings, improving mentalizing capacity | Individual and/or group therapy over 18 months | Relationship difficulties, identity confusion, emotional misunderstandings |
| Schema Therapy | Healing childhood wounds and changing deep patterns | Identifying schemas, limited reparenting, experiential techniques | Individual therapy, sometimes group | History of childhood trauma or neglect, PTSD comorbidity |
| TFP | Using the therapeutic relationship to heal | Analyzing transference, integrating split self-images, confrontation techniques | Intensive individual therapy (2x/week) | Severe relationship problems, identity disturbance, willingness for intensive work |
The therapeutic alliance—the trust and rapport between you and your therapist—is one of the strongest predictors of success. Research consistently shows its importance, so finding a therapist you feel safe and respected by is paramount.
Prognosis: Can BPD Be Cured?
While we talk about “remission” rather than “cure,” the answer to “Can you get better?” is a resounding yes. The long-term outlook for BPD is remarkably positive. A landmark 16-year study found that 99% of people with BPD achieved remission after 16 years of treatment. Remission means symptoms subside, and you can live a high-quality life with stable relationships and a clear sense of self. BPD is not a life sentence; it is a treatable condition, and recovery is the expected outcome with proper care.
Understanding Borderline Personality Disorder and the Path to Recovery
Living with Borderline Personality Disorder (BPD) can feel like an endless emotional storm, characterized by intense mood swings, unstable relationships, and frightening impulsivity. This condition, marked by emotional dysregulation, affects millions of people, who often struggle with a fragmented sense of self and chronic feelings of emptiness.
If this sounds familiar, the most important thing to know is that BPD is highly treatable. Outdated stigmas suggested it was a lifelong, untreatable condition, but modern research proves otherwise. Multiple evidence-based borderline personality disorder therapies have been developed to specifically target BPD symptoms, offering real hope for recovery.
The long-term outlook is incredibly positive. Studies show that 91% of people with BPD achieve remission after 10 years of treatment, and 99% after 16 years. Effective therapies include:
- Dialectical Behavior Therapy (DBT)
- Mentalization-Based Therapy (MBT)
- Schema Therapy (ST)
- Transference-Focused Psychotherapy (TFP)
Recovery is a journey, not a quick fix, but it is absolutely possible. At Addiction Helpline America, we understand that BPD often co-occurs with substance use disorders. Our experienced team connects individuals with specialized dual diagnosis programs that treat the whole person. We are here to guide you toward compassionate, evidence-based care.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Terms related to borderline personality disorder therapies:
Primary Evidence-Based Borderline Personality Disorder Therapies
For treating BPD, structured, evidence-based psychotherapy is the foundation of healing. The goal is not just to manage symptoms but to regain control over your life. There is no one-size-fits-all approach, which is why we focus on connecting you with borderline personality disorder therapies that match your unique needs.
Dialectical Behavior Therapy (DBT): The Gold Standard
DBT is often the first therapy mentioned for BPD, and for good reason. Developed by Dr. Marsha Linehan, DBT is an empirically supported therapy for BPD that balances self-acceptance with the need for change. It teaches four core skill sets: mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness. Through a combination of individual therapy, group skills training, and phone coaching, DBT provides a comprehensive structure for building a life worth living. Its effectiveness is backed by extensive research, showing reductions in self-harm and hospitalizations.
Mentalization-Based Therapy (MBT)
Mentalization-Based Therapy helps you develop the ability to “mentalize”—to understand the mental states (feelings, thoughts, intentions) underlying your own and others’ actions. This capacity is often disrupted in BPD, leading to misunderstandings in relationships. MBT teaches you to step back from intense emotions and reflect with curiosity, improving self-awareness and interpersonal insight. A 2019 review found evidence that MBT can be as effective as other therapies for BPD.
Schema Therapy (ST)
Schema Therapy digs into the childhood roots of BPD, focusing on how unmet emotional needs create deeply ingrained negative patterns, or “schemas.” The therapy helps you understand these patterns and heal them through cognitive techniques and experiential exercises, such as imagery and role-playing. A key element is “limited reparenting,” where the therapist provides a corrective emotional experience of safety and validation. Pilot studies on group ST show it is particularly promising for those with co-occurring trauma or PTSD.
Transference-Focused Psychotherapy (TFP)
Transference-Focused Psychotherapy is a psychodynamic approach that uses the patient-therapist relationship as a laboratory for change. It focuses on “transference,” where you unconsciously project past relationship dynamics onto your therapist. By exploring these patterns in the moment, TFP helps you integrate “split” views of yourself and others (e.g., all-good or all-bad). This intensive therapy, typically twice a week, leads to a more stable identity and healthier relationships.
Other and Adjunctive Therapeutic Approaches
While core evidence-based therapies are the foundation of BPD treatment, a comprehensive plan often includes other supportive approaches. These adjunctive treatments help build skills and create a holistic path to recovery.
At Addiction Helpline America, we believe in a multi-faceted approach to mental health. Explore our Mental Health Resources at Addiction Helpline America for more information.
Skills-Based Group Programs for BPD
Group programs like Systems Training for Emotional Predictability and Problem Solving (STEPPS) are an excellent complement to individual therapy. STEPPS is a 20-week program that teaches emotion management and problem-solving skills while actively involving a patient’s support system. Research comparing STEPPS with DBT showed that both were effective at significantly reducing BPD symptoms, making it a valuable, structured option for skill-building.
The Role of Group Therapy and Creative Therapies
Group therapy offers a safe space to practice interpersonal skills with peers who understand the struggles of BPD, which helps reduce isolation and shame. When emotions are too intense for words, creative therapies (art, music, drama) provide a non-verbal outlet. These modalities can help you process trauma and regulate emotions by channeling them into a tangible form, adding another dimension to your healing journey alongside core borderline personality disorder therapies.
The Role of Medication in BPD Treatment
It is crucial to understand that no medications are specifically FDA-approved to treat BPD itself. Medication is considered an adjunctive treatment used to manage specific, severe symptoms that may accompany BPD, such as intense mood swings, paranoia, or co-occurring depression and anxiety. Any medication should be time-limited, symptom-focused, and always used in conjunction with psychotherapy, which addresses the core issues of the disorder. The decision to use medication should be made carefully with your mental health professional.
We can help you understand these options. Learn about medication and inpatient rehab options at Addiction Helpline America.
Diagnosis, Prognosis, and Choosing the Right Therapy
Navigating a BPD diagnosis and treatment options can be complex, but understanding the process is the first step toward empowered, person-centered care.
How BPD is Diagnosed and Its Challenges
A BPD diagnosis is made after a thorough clinical interview based on DSM-5 criteria, which require a person to exhibit at least five of nine specific patterns related to emotional instability, relationships, and impulsivity. The diagnosis is challenging due to symptom overlap with other conditions like bipolar disorder or PTSD, often leading to misdiagnosis. Stigma has also been a historical barrier. Importantly, while once thought to be a “women’s disorder,” research shows it affects men and women equally, but gender biases can lead to men’s symptoms being mislabeled.
Choosing Among Borderline Personality Disorder Therapies
Choosing the right therapy is a personal decision made with a professional. Factors include symptom severity, co-occurring conditions, and personal preference. The table below compares the primary borderline personality disorder therapies.
| Therapy | Primary Focus | Key Techniques | Typical Structure |
|---|---|---|---|
| Dialectical Behavior Therapy (DBT) | Emotional regulation, distress tolerance, interpersonal effectiveness | Mindfulness, distress tolerance, emotion regulation, interpersonal effectiveness skills training, phone coaching | Weekly individual and group sessions, homework, crisis support |
| Mentalization-Based Therapy (MBT) | Improving ability to understand own and others’ mental states | Reflective questioning, challenging assumptions, exploring mental states in the therapeutic relationship | Weekly individual and group sessions; often 18 months in duration |
| Schema Therapy (ST) | Identifying and healing early maladaptive schemas from childhood | Cognitive restructuring, experiential techniques (imagery, role-play), limited reparenting | Individual therapy, sometimes group therapy |
| Transference-Focused Psychotherapy (TFP) | Resolving fragmented self and object representations through the therapeutic relationship | Interpretation of transference and countertransference, clarification, confrontation of split affect states | Intensive individual therapy (often 2 sessions per week) |
Above all, the therapeutic alliance—your relationship with your therapist—is a powerful predictor of success. Research on the importance of the therapeutic alliance confirms that a strong, trusting connection is critical for positive outcomes.
Prognosis: Can BPD Be Cured?
While “cure” isn’t the typical term, the prognosis for BPD is overwhelmingly positive. The goal is remission, a sustained period where symptoms are significantly reduced, allowing for a high quality of life. A landmark 16-year longitudinal study provides incredible hope: after 10 years, 91% of participants went into remission, and after 16 years, 99% were in remission. Recovery is not just possible—it’s probable with consistent, evidence-based treatment.
Self-Care, Support Systems, and When to Seek Help
Recovery from BPD extends beyond therapy sessions; it involves building a life that supports your daily well-being. Combining professional borderline personality disorder therapies with self-care and a strong support network is key to lasting recovery.

Self-Care Strategies for Managing BPD Symptoms
Effective self-care involves creating a toolkit of healthy coping skills for when emotions become overwhelming. This can include physical outlets for anger (like exercise), grounding techniques for anxiety (like focusing on your five senses), or using strong sensory input (like holding ice) to counter dissociation. Beyond in-the-moment skills, establishing a daily routine, prioritizing sleep, maintaining healthy nutrition, and getting regular exercise form the backbone of emotional stability. For more ideas, consider resources like these self-care tips from Mind.
The Importance of Family and Support Systems
Recovery is rarely a solo journey. When family and loved ones are involved and educated, treatment outcomes improve dramatically. Family psychoeducation helps replace frustration with empathy and understanding. Learning to set healthy boundaries and improve communication can reduce conflict and create a sustainable support network. The American Psychiatric Association emphasizes involving family as a crucial component of comprehensive care.
When and How to Seek Professional Help
It’s time to seek professional help if BPD symptoms are significantly disrupting your daily life, relationships, or work, or if you are experiencing persistent, unmanageable emotional pain. Thoughts of self-harm or suicide require immediate professional intervention.
If you are in crisis, call or text The 988 Suicide & Crisis Lifeline at 988. If you are in immediate danger, call 911.
At Addiction Helpline America, we specialize in connecting people to treatment centers offering specialized care for BPD and co-occurring substance use disorders. Our guidance is free, confidential, and personalized. Let us help you take the first step. Learn more about How to Get Help at Addiction Helpline America.
Frequently Asked Questions about Borderline Personality Disorder Therapies
What is the most effective therapy for BPD?
There is no single “most effective” therapy that fits everyone. Dialectical Behavior Therapy (DBT) is the most researched and often called the gold standard. However, other borderline personality disorder therapies like Mentalization-Based Therapy (MBT), Schema Therapy (ST), and Transference-Focused Psychotherapy (TFP) are also proven to be highly effective. The best therapy for you depends on your specific symptoms, needs, and personal preference. Crucially, the quality of your relationship with your therapist (the therapeutic alliance) is one of the strongest predictors of success.
How long does therapy for BPD take?
Therapy for BPD is a long-term commitment. It is not a quick fix. Most comprehensive programs, such as DBT or MBT, are designed to last for one year or more. This timeframe allows for the deep work of learning new skills, practicing them in real-world situations, and building a stable foundation for lasting change. While it’s a marathon, not a sprint, the investment is worth it, as research shows the vast majority of people achieve long-term remission with consistent treatment.
Is BPD more common in women?
For decades, BPD was thought to be more common in women, but this is a misconception. Recent research shows it affects men and women equally. The diagnostic disparity arose because women are more likely to seek mental health care and because of gender biases in how symptoms are interpreted. For example, a man’s anger or impulsivity might be misdiagnosed as another disorder or dismissed, while the same symptoms in a woman are attributed to BPD. It is vital that everyone receives an accurate diagnosis regardless of gender.
Conclusion: Finding Hope and Healing on the Path to Recovery
If you are struggling with Borderline Personality Disorder, the most important message is one of hope: BPD is treatable. Decades of research have produced proven borderline personality disorder therapies that lead to lasting recovery.
Whether it’s DBT, MBT, ST, or TFP, these approaches help people regain control, build stable relationships, and find fulfillment. The statistics are powerfully encouraging: studies show that up to 99% of people with BPD achieve remission with long-term treatment. Recovery is not just a possibility; it is the expected outcome for those who engage in evidence-based care.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Taking the first step is often the hardest. At Addiction Helpline America, we make it easier. We provide free, confidential, and personalized guidance to connect you with specialized treatment centers across the United States, including those that treat co-occurring substance use disorders. Our network serves every state, from Alabama to Wyoming.
You don’t have to steer this alone. Your path to healing can start today. Find professional help for BPD and related conditions and let us support you on your journey to recovery.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.















