Understanding Alcohol Withdrawal: What You Need to Know
Alcohol withdrawal symptoms occur when someone who drinks heavily suddenly stops or significantly reduces their alcohol use. These symptoms can range from mild anxiety and tremors to life-threatening complications like seizures and delirium tremens. Here’s what you need to know:
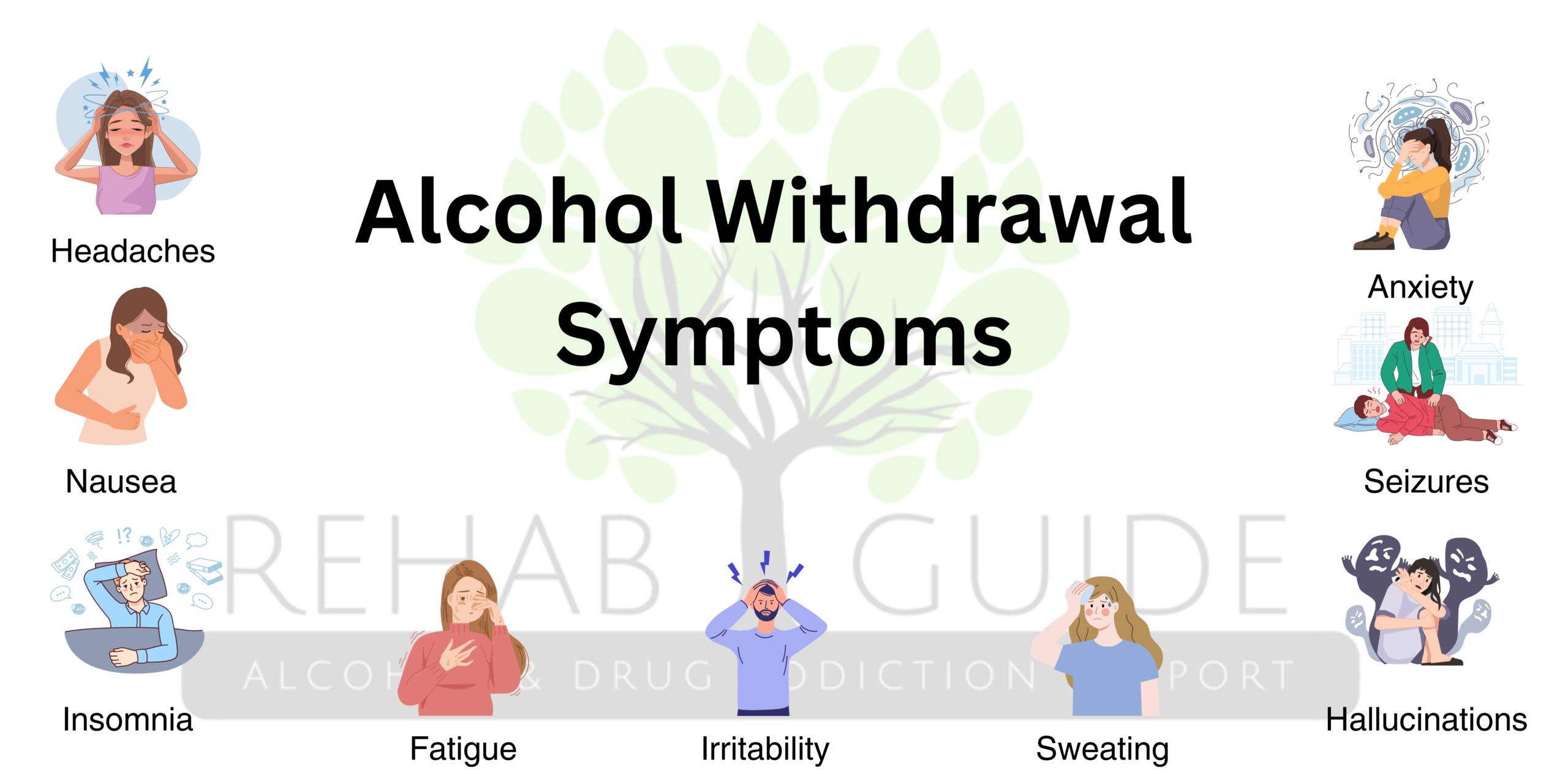
Common Alcohol Withdrawal Symptoms:
- Mild (6-12 hours): Anxiety, insomnia, nausea, headache, hand tremors, sweating
- Moderate (12-48 hours): Increased blood pressure and heart rate, confusion, hallucinations, fever
- Severe (48-72+ hours): Seizures, delirium tremens (DTs), severe disorientation, agitation
Key Facts:
- Symptoms typically begin 6-12 hours after the last drink.
- Peak severity occurs between 24-72 hours.
- About 50% of people with alcohol use disorder experience withdrawal.
- Delirium tremens affects 5-10% of those withdrawing and can be fatal without treatment.
- Medical supervision is critical for safe withdrawal.
Alcohol withdrawal happens because your brain adapts to constant alcohol exposure. To compensate for alcohol’s depressive effects, your brain’s chemistry changes. When alcohol is removed, your central nervous system becomes hyperactive, causing withdrawal symptoms.
You should never attempt to detox from alcohol alone. Withdrawal can become a medical emergency within hours. Complications like seizures and delirium tremens require immediate professional intervention. The mortality rate for severe withdrawal can be as high as 5-10% without medical care, but drops to around 1% with treatment.
At Addiction Helpline America, we’ve supported thousands through the challenges of alcohol withdrawal symptoms. Our team is here 24/7 to connect you with life-saving medical detox and comprehensive treatment options.
Quick look at alcohol withdrawal symptoms:
What Causes Alcohol Withdrawal and Who Is at Risk?
When you drink heavily over time, your brain makes significant adjustments to compensate. Understanding why alcohol withdrawal symptoms occur shows why medical supervision is essential.
Alcohol is a central nervous system depressant, acting like a brake on your brain. With chronic heavy drinking, your brain adapts by pressing harder on its internal “gas pedal” to maintain normal function. It rewires its chemistry to expect alcohol’s presence.
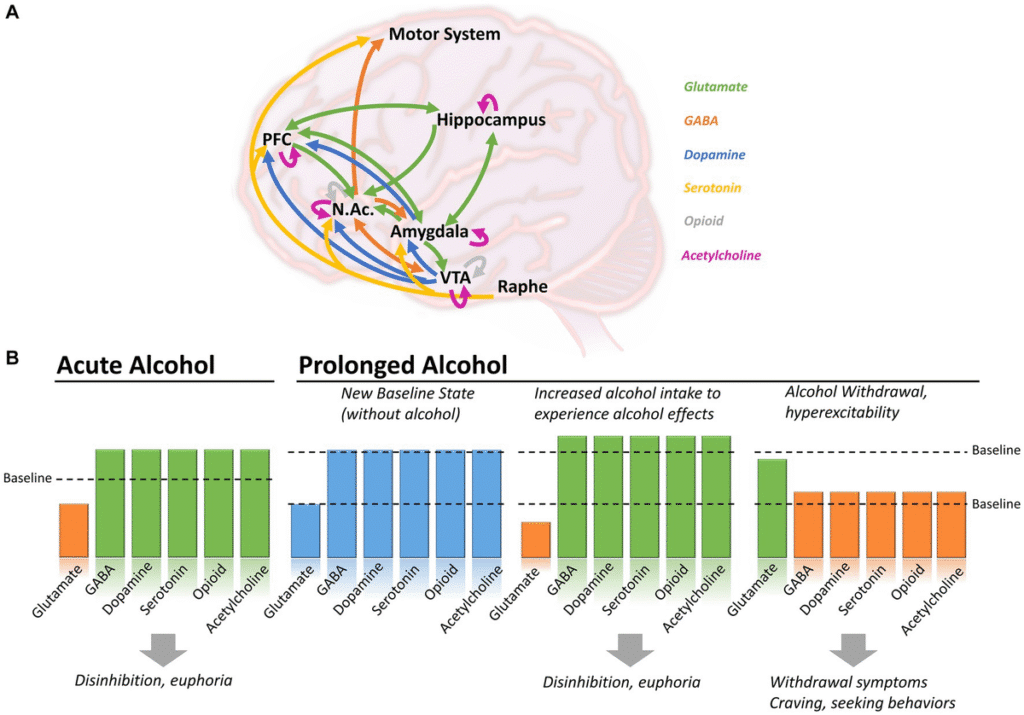
The Science Behind Withdrawal
Your brain uses neurotransmitters to communicate. The main calming one is GABA, while glutamate is excitatory. Chronic alcohol use makes the brain less responsive to GABA and more sensitive to glutamate. This adaptation, called tolerance, allows a person to function with high blood alcohol levels.
When alcohol is suddenly removed, the brain is left in a hyper-excitable state. The calming systems are weak, and the excitatory systems are in overdrive. This rebound effect causes alcohol withdrawal symptoms, from shakes and anxiety to seizures. This imbalance also affects dopamine and serotonin, explaining mood swings and cravings. The resulting autonomic hyperactivity causes a racing heart, high blood pressure, and profuse sweating.
Are You at Risk for Withdrawal?
Anyone with a physical dependence on alcohol is at risk. Alcohol Use Disorder (AUD) is the medical term for being unable to control your drinking despite negative consequences. According to the National Institute on Alcohol Abuse and Alcoholism, a majority of people with AUD may experience some form of withdrawal.
Several factors increase your risk for severe alcohol withdrawal symptoms:
- Drinking History: The longer and more heavily you’ve been drinking, the higher your risk. Your brain has had more time to adapt, making the rebound effect more intense.
- Previous Detox Experiences: Each withdrawal episode can be more severe than the last, a phenomenon known as “kindling.” This is especially true for seizure risk.
- Age and Health: Being over 65 or having co-occurring medical conditions like heart or liver disease complicates withdrawal and increases the danger.
- Nutritional Deficiencies: Heavy drinking depletes essential vitamins like thiamine (B1), magnesium, and folate. A thiamine deficiency can lead to Wernicke-Korsakoff syndrome, a severe brain disorder.
- Binge Drinking: Regular binge drinking (5+ drinks for men, 4+ for women in about two hours) can also lead to physical dependence.
- Other Factors: A personal or family history of severe withdrawal, seizures, or co-occurring mental health conditions like anxiety, depression, or PTSD also increases your risk.
There is no way to predict exactly how withdrawal will affect you. Your unique body chemistry, drinking patterns, and overall health all play a role. This complexity is why detoxing alone is so dangerous and why medical supervision can save your life.
At Addiction Helpline America, we understand that recognizing your risk is the first step. We’re here 24/7 to connect you with medical professionals who can assess your situation and provide the safest path forward.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
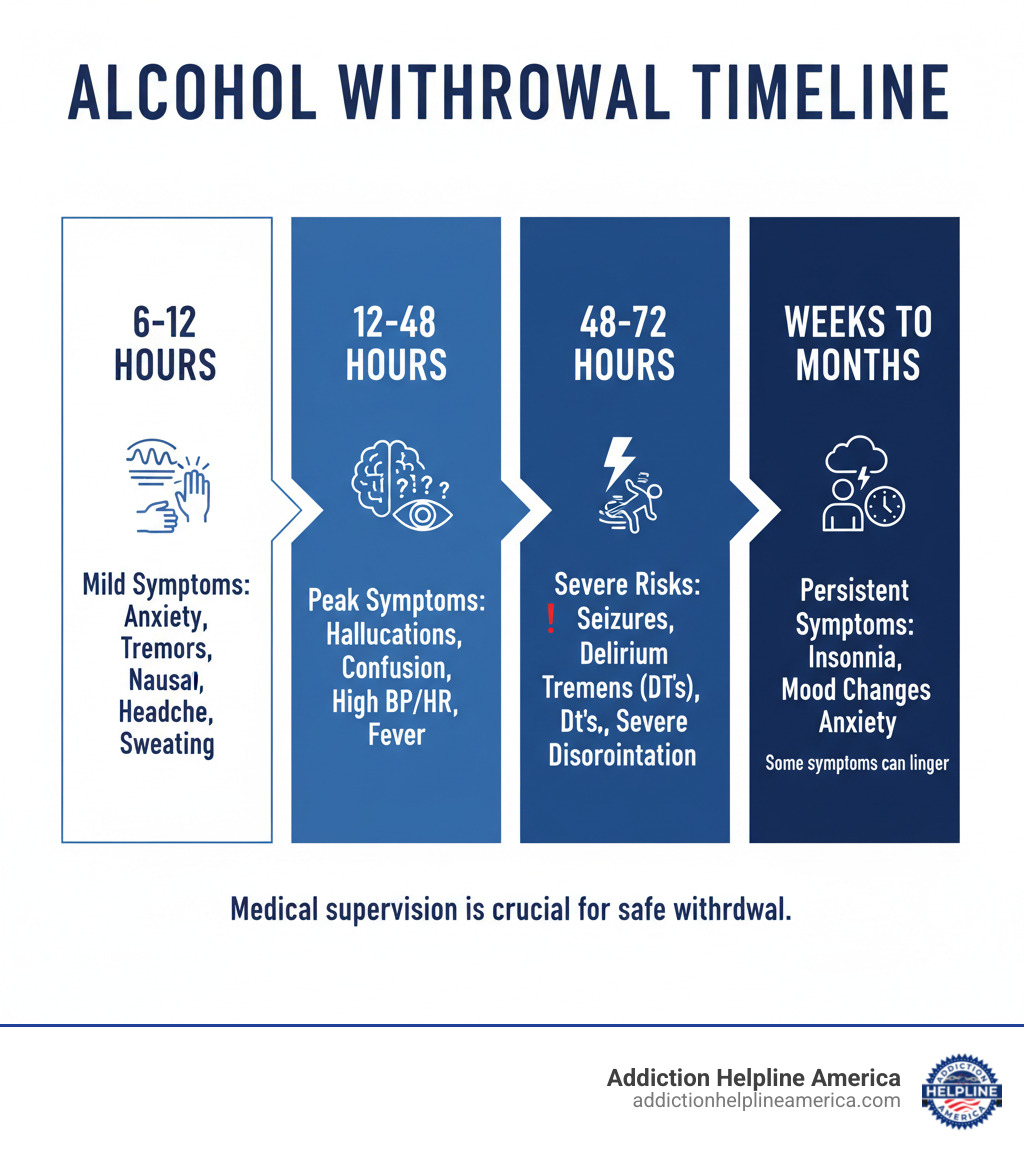
The Timeline and Stages of Alcohol Withdrawal Symptoms
When someone with a physical dependence stops drinking, alcohol withdrawal symptoms usually follow a predictable pattern, though the experience varies. The timeline depends on how much and how long you’ve been drinking, plus your overall health.
Medical professionals use the Clinical Institute Withdrawal Assessment for Alcohol, Revised (CIWA-Ar) scale to measure symptom intensity. This helps them provide the right level of care. Understanding this timeline highlights why immediate medical supervision is critical. The National Institute on Alcohol Abuse and Alcoholism offers extensive resources on this topic.
Stage 1: Early Alcohol Withdrawal Symptoms (6-12 Hours)
The first signs typically appear within 6 to 12 hours of the last drink. These are a warning signal that your body is undergoing a significant change. Symptoms include:
- Anxiety and nervousness
- Insomnia
- Nausea and vomiting
- Headaches
- Heart palpitations
- Hand tremors (“the shakes”)
- Excessive sweating
- Irritability and mood swings
These early symptoms can escalate quickly without medical care.
Stage 2: Peak Symptoms & Hallucinations (12-48 Hours)
Symptoms usually peak between 24 and 72 hours. During this stage, the physical and psychological effects become more pronounced.
- Physical Symptoms: Blood pressure and heart rate increase, and body temperature may rise, causing a fever.
- Psychological Symptoms: Confusion, disorientation, and agitation often intensify.
- Alcoholic Hallucinosis: Some people experience hallucinations, seeing, hearing, or feeling things that aren’t there. While different from delirium tremens, it’s a serious warning sign.
- Seizures: The risk of generalized tonic-clonic seizures is highest between 24 and 48 hours. Seizures are a medical emergency and a primary reason why detoxing alone is so dangerous.
Stage 3: Severe Alcohol Withdrawal Symptoms and Complications (48-72+ Hours)
This is the most dangerous period of withdrawal and represents a medical emergency. It can sometimes be delayed for a week or more.
Delirium Tremens (DTs) is the most severe form of withdrawal, affecting 5-10% of people in withdrawal. It involves sudden, severe confusion, extreme agitation, vivid hallucinations, and dangerous instability in vital signs. Without treatment, the mortality rate for DTs can be 5-10%. With medical care, that rate drops to less than 1%.
Grand mal seizures are another serious risk. Up to 30% of withdrawal seizures can progress to DTs. People in this stage may also experience severe disorientation and a persistent high fever, both of which require immediate medical attention.
These severe alcohol withdrawal symptoms are why medical supervision is essential. For anyone who has been drinking heavily, professional medical detox is the safest option and can be the difference between life and death. Addiction Helpline America is available 24/7 to connect you with medically supervised detox facilities to keep you safe through every stage.
The Dangers of Withdrawal and When to Seek Help
To be clear: alcohol withdrawal symptoms can be fatal. This isn’t to scare you, but to protect you. Alcohol is one of the few substances where withdrawal can be life-threatening. Attempting to detox alone is a risk not worth taking.
When you stop drinking after long-term heavy use, your body enters a period of dangerous instability. Things can go wrong quickly, which is why medical supervision is life-saving. Detox facilities provide 24/7 monitoring and can intervene immediately if complications arise, using medications and equipment to keep you safe.
Potential Complications
Understanding the risks explains why professional detox is critical. Major complications include:
- Seizures: Occurring 6 to 48 hours after the last drink, they can cause injury, neurological damage, or progress to a non-stop seizure state (status epilepticus), which is a medical emergency.
- Delirium Tremens (DTs): The most severe form of withdrawal, DTs involves extreme confusion, a racing heart, high blood pressure, and terrifying hallucinations. The mortality rate is 5-10% without treatment but drops to less than 1% with medical care.
- Dehydration and Electrolyte Imbalances: Withdrawal can deplete essential minerals, leading to unstable heart rhythms (cardiac arrhythmias) and other cardiac risks.
- Aspiration Pneumonia: Inhaling stomach contents into the lungs during vomiting or a seizure can cause a serious, potentially fatal lung infection.
- Wernicke-Korsakoff Syndrome: Caused by a severe thiamine (Vitamin B1) deficiency, this neurological condition can lead to permanent memory loss and other cognitive impairments. It is preventable with proper medical care during detox.
When to Call for Medical Help Immediately
Knowing the warning signs of a medical emergency can save a life. If you or someone else experiences any of the following alcohol withdrawal symptoms, call 911 or go to the nearest emergency room immediately:
- Hallucinations (seeing, hearing, or feeling things that aren’t there)
- Seizures of any kind
- Severe confusion or disorientation
- High fever
- Chest pain or pressure
- Uncontrollable shaking
- Extreme agitation or restlessness
Even if your symptoms seem mild, seek medical advice if you have a history of heavy drinking or previous severe withdrawal. Symptoms can escalate unpredictably. What starts as mild anxiety can become a seizure hours later.
At Addiction Helpline America, we’ve seen many people try to “tough it out” at home, only to end up in a dangerous situation. We’ve also helped thousands make the safer choice of professional medical detox. We’re available 24/7 to help you find the right medical services. You shouldn’t go through this alone.
How Is Alcohol Withdrawal Diagnosed and Treated?
Seeking help at a medical detox facility is the most important step toward safely managing alcohol withdrawal symptoms. The process begins with a thorough assessment to provide the right support to keep you safe and comfortable.
Diagnosis and Assessment
Diagnosing withdrawal starts with a conversation. A healthcare team will ask about your drinking history: how much you drink, for how long, and when you had your last drink. This helps predict the potential severity of your symptoms. It’s also crucial to share any past withdrawal experiences, as each episode can be worse than the last (a phenomenon called “kindling”).
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
A physical exam will check your vital signs (heart rate, blood pressure, temperature) and look for signs like tremors or sweating. Blood tests are used to check electrolyte levels, liver and kidney function, and nutritional deficiencies, especially thiamine.
Clinicians use the Clinical Institute Withdrawal Assessment for Alcohol, Revised (CIWA-Ar) scale to objectively measure the severity of ten common symptoms. The score helps guide medication decisions and ensures you receive the appropriate level of care. This careful diagnostic process also rules out other conditions that might mimic alcohol withdrawal symptoms.
Medical Treatment Options
The goal of treatment is to keep you safe and minimize discomfort. Your plan will be customized to your needs.

- Benzodiazepines: Medications like lorazepam and diazepam are the cornerstone of treatment. They calm the overactive central nervous system to reduce anxiety and, most importantly, prevent seizures and delirium tremens.
- Nutritional Support: Thiamine (Vitamin B1) is given to prevent Wernicke-Korsakoff syndrome, a serious brain condition. You will also receive other essential vitamins and minerals.
- IV Fluids and Electrolytes: Fluids are often given intravenously to correct dehydration and restore electrolyte balance, which is crucial for heart function.
- Supportive Care: A calm, quiet environment with continuous monitoring of vital signs and emotional support is key. Other medications may be used to control specific symptoms like a racing heart or high blood pressure.
With proper medical treatment, the prognosis for alcohol withdrawal is excellent. The mortality rate drops from as high as 10% to less than 1%. This stark difference shows why medical detox is essential.
For more information, the Substance Abuse and Mental Health Services Administration provides valuable resources.
At Addiction Helpline America, we connect you with facilities that provide this comprehensive care, ensuring your safety from the very first step of recovery.
Finding Support for Long-Term Recovery
Successfully navigating alcohol withdrawal symptoms with medical detox is a critical first step, but it’s just the beginning. Lasting recovery involves understanding the root causes of your drinking and learning to live without alcohol by addressing the underlying Alcohol Use Disorder (AUD).
Recovery is an ongoing process that requires support, tools, and professional guidance long after detox. While setbacks can happen, research shows that most people with AUD can significantly improve their lives with sustained effort. The importance of aftercare—what happens after detox—cannot be overstated.
Support Groups and Resources
Building a strong support system is fundamental to maintaining sobriety. At Addiction Helpline America, we connect you with a comprehensive network of resources to support every step of your journey.
- Individual Therapy: Approaches like Cognitive Behavioral Therapy (CBT) help you identify triggers, develop coping skills, and change the thought patterns that fuel drinking.
- Outpatient Programs: Intensive Outpatient Programs (IOPs) and Partial Hospitalization Programs (PHPs) offer structured therapy while you live at home, bridging the gap between inpatient care and independent living.
- Family Support: Family therapy helps repair relationships and teaches loved ones how to best support your recovery. Resources like Al-Anon provide support specifically for family and friends.
- Community and Mutual Support Groups: Connecting with peers who understand is invaluable. Options include Alcoholics Anonymous (AA), SMART Recovery, LifeRing Secular Recovery, and Women for Sobriety (WFS). Many offer virtual meetings for easy access.
- Medication-Assisted Treatment (MAT): FDA-approved medications like Naltrexone, Acamprosate, and Disulfiram can help reduce cravings and support abstinence. These are medical tools that address the brain chemistry of addiction.
Addiction Helpline America support services are here to guide you. We connect individuals nationwide to addiction and mental health treatment centers across all 50 states, from California and Florida to Texas and New York. Our service is free, confidential, and personalized to help you find the right program from our vast network, including telehealth options. Recovery is possible, and you don’t have to figure it out alone.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Conclusion
Facing alcohol withdrawal symptoms is an immense challenge. We’ve seen that when the body is deprived of alcohol after long-term use, it can go into overdrive, leading to symptoms that range from tremors and anxiety to life-threatening seizures and delirium tremens. This is a serious medical event that should never be handled alone.
The science is clear: this is a biological process, not a test of willpower. It requires medical attention.
But there is immense hope. Recovery is not only possible—it happens every day. With professional medical supervision, the risk of dying from severe alcohol withdrawal symptoms drops from as high as 10% to less than 1%. Medical detox provides a critical safety net, making the process manageable and giving you the best possible chance at success.
At Addiction Helpline America, we know how frightening it is to ask for help. Making that call is one of the bravest things you can do. We offer free, confidential guidance to connect you with the right treatment for your unique situation. Our network spans the entire United States, and we are dedicated to matching you with a program that can save your life.
The journey to recovery doesn’t end with detox, but it cannot begin without it. If you or a loved one is struggling, please don’t wait. The window for safe intervention is often short.
You deserve a life free from alcohol dependence. It starts with one phone call.
Find personalized treatment options that fit your unique needs. Our team is standing by 24/7, ready to help you take the first step toward the healthier life you deserve.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.















