Understanding Antisocial Personality Disorder and Your Treatment Options
Antisocial personality disorder treatments focus on managing symptoms and reducing harmful behaviors through psychotherapy, medication for co-occurring conditions, and long-term support. While there is no cure, effective treatment can help individuals lead more stable lives.
Key Treatment Approaches:
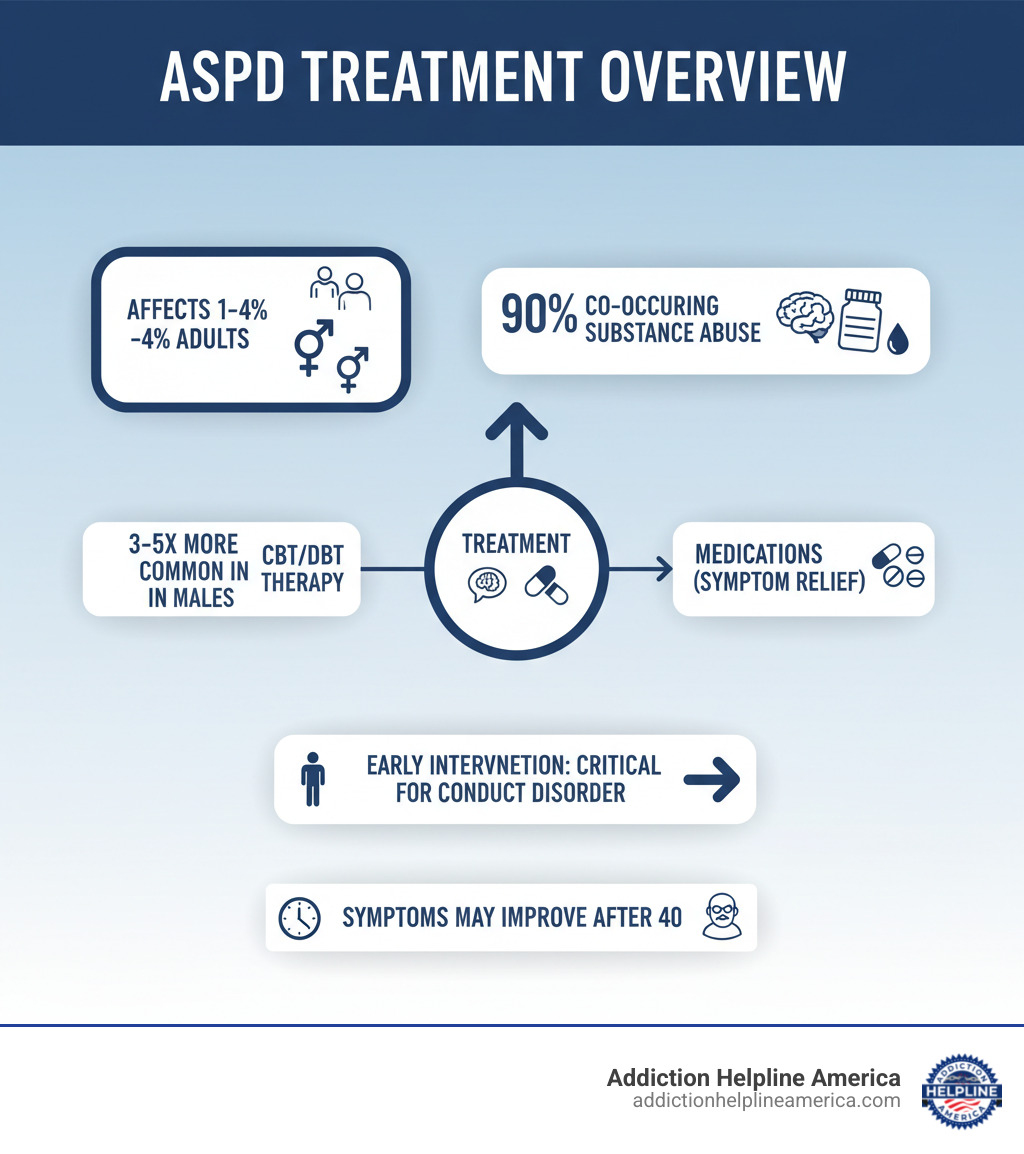
- Psychotherapy: Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT) help address distorted thinking and improve impulse control.
- Medication: Mood stabilizers, antipsychotics, and antidepressants manage aggression, depression, and anxiety.
- Structured Programs: Residential treatment and therapeutic communities provide intensive support.
- Early Intervention: Treating conduct disorder in childhood can reduce the risk of developing ASPD.
Antisocial personality disorder (ASPD), affecting an estimated 1% to 4% of adults in the U.S., is a mental health condition marked by a persistent disregard for others’ rights, manipulation, and a lack of remorse. This deeply ingrained pattern of thinking and acting typically begins before age 15.
Research shows that up to 90% of individuals with ASPD also struggle with substance use disorders. Many don’t seek help voluntarily, often entering treatment through the legal system or at the urging of family.
However, treatment can help. While ASPD is a lifelong condition, symptoms often become less severe after age 40. With the right therapy, medication for co-occurring issues, and consistent support, individuals can learn to manage their impulses and build more stable lives.
At Addiction Helpline America, we connect individuals and families with evidence-based antisocial personality disorder treatments that address both personality disorders and addiction. Our team understands that recovery requires a comprehensive, personalized approach.
Easy antisocial personality disorder treatments glossary:
Understanding Antisocial Personality Disorder (ASPD)
Antisocial personality disorder (ASPD) is a serious mental health condition characterized by a consistent disregard for the rights and feelings of others. It is a deeply rooted pattern of thinking and behaving, not just an occasional moment of poor judgment. People with ASPD often lack empathy and may manipulate others to get what they want, making it one of the most challenging conditions to address.
ASPD belongs to the Cluster B personality disorders, which are characterized by dramatic, emotional, or unpredictable behaviors. The hallmark traits of ASPD—a pervasive disregard for others, lack of empathy, and manipulative behavior—create significant challenges for the individual and those around them.
Diagnostic Criteria and Common Symptoms
An ASPD diagnosis requires meeting specific criteria from the DSM-5. The individual must be at least 18 years old, with clear evidence of conduct disorder before age 15. The diagnosis requires at least three of the following seven characteristics:
- Deceitfulness: Persistent lying or conning others for personal gain.
- Impulsivity: Acting without thinking about consequences.
- Irritability and aggressiveness: Repeated fights or assaults.
- Failure to follow laws and social norms.
- Reckless disregard for the safety of self or others.
- Consistent irresponsibility: Inability to maintain a job or honor financial obligations.
- Lack of remorse: Indifference to hurting or mistreating others.
Other common signs include a sense of entitlement, an inflated self-view, and a superficial charm used for manipulation. Maintaining stable relationships, friendships, or employment is often impossible over time. For more details on diagnosis, resources like Mind’s website offer comprehensive information.
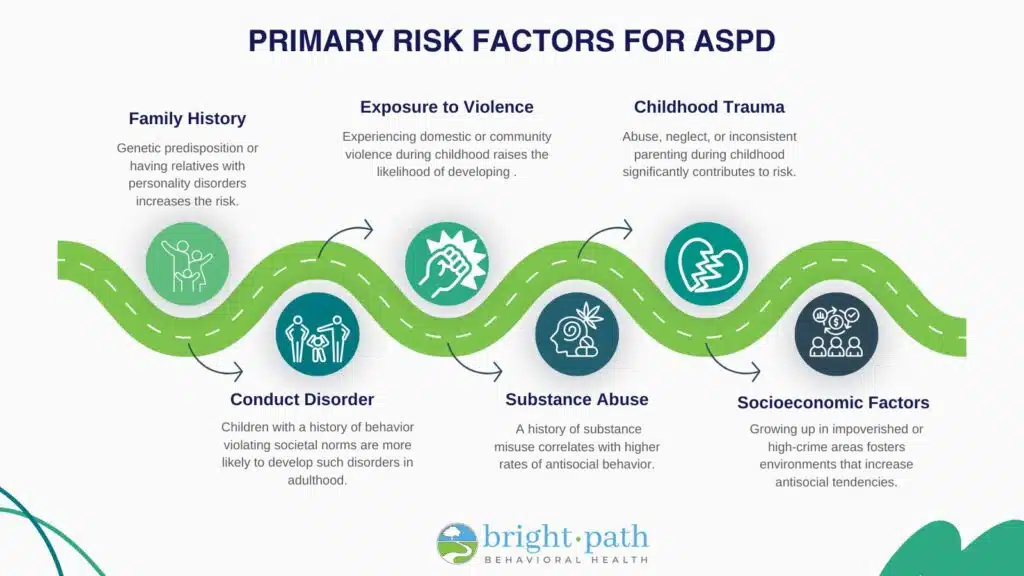
Causes, Risk Factors, and Early Intervention
ASPD develops from a combination of genetic predisposition, environmental factors, and brain differences. Genetics play a significant role, with risk increasing if a biological relative has ASPD. Specific genes, like variations in the MAO-A gene, may be involved, especially when combined with adverse childhood experiences.
Childhood abuse and neglect are strongly linked to ASPD. Traumatic events, exposure to violence, or an unstable home life dramatically increase risk. Brain imaging studies have also revealed brain differences in people with ASPD, such as reduced gray matter in the prefrontal cortex, which is involved in impulse control. Altered serotonin levels have also been linked to impulsive aggression.
Fortunately, early intervention makes a real difference. Treating conduct disorder in childhood can change a person’s trajectory. While nearly 40% of boys and 25% of girls with conduct disorder may develop ASPD, most do not, especially with proper treatment. Parent-training programs and family therapies are critical, particularly when substance use is a factor. We offer comprehensive information about adolescent substance abuse because conduct disorder is one of the strongest predictors of ASPD, making early treatment essential.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
How ASPD Differs from Other Personality Disorders
ASPD shares its Cluster B classification with Borderline Personality Disorder (BPD) and Narcissistic Personality Disorder (NPD). While they all involve interpersonal difficulties, their core motivations and behaviors differ, requiring unique antisocial personality disorder treatments.
- ASPD is driven by a desire for personal gain and power, with a disregard for others’ rights.
- BPD is driven by a fear of abandonment and a need to escape intense emotional pain.
- NPD is driven by the need to maintain an inflated self-image and seek admiration.
These differences in motivation, emotional stability, and empathy are crucial for diagnosis and treatment planning. The table below highlights these distinctions.
| Feature | Antisocial Personality Disorder (ASPD) | Borderline Personality Disorder (BPD) | Narcissistic Personality Disorder (NPD) |
|---|---|---|---|
| Core Motivation | Personal gain, power, manipulation; disregard for others’ rights | Avoidance of abandonment; relief from intense emotional pain; desire for connection | Maintaining inflated self-image; seeking admiration; avoiding perceived flaws |
| Emotional Stability | Often appears cold, callous, lacking genuine emotion; can feign emotions | Highly unstable, intense mood swings; chronic feelings of emptiness; intense anger | Fluctuates between grandiosity and intense shame/fragility when challenged |
| Interpersonal Relations | Exploitative, manipulative; views others as objects; superficial charm; unstable | Intense, unstable, and conflict-ridden; fear of abandonment; idealization/devaluation | Superficial, exploitative; lacks empathy; expects special treatment; envious of others |
| Empathy | Profound lack of empathy; indifferent to suffering of others | Can experience empathy, but often overshadowed by own emotional distress | Lacks empathy; unable to recognize or identify with others’ feelings and needs |
| Self-Perception | Often grandiose, entitled, sees self as superior; blames others | Unstable sense of self; identity disturbance; chronic emptiness | Grandiose sense of self-importance, uniqueness, and superiority |
| Impulsivity | High impulsivity, especially in actions that benefit self (e.g., lawbreaking) | High impulsivity, often self-damaging (e.g., self-harm, reckless spending, substance use) | Less overt impulsivity, but can be impulsive in seeking validation or rage outbursts |
Evidence-Based Antisocial Personality Disorder Treatments
Treating ASPD is a significant challenge in mental healthcare, largely because individuals with the disorder often don’t believe they have a problem. However, antisocial personality disorder treatments can be effective in improving lives.

Treatment goals focus on managing symptoms like aggression and impulsivity, reducing harmful behaviors such as criminal activity and substance abuse, and helping individuals build more stable lives. This is a long-term commitment, as most people with ASPD lack insight into their condition (a state known as anosognosia) and often enter treatment only when mandated by courts or family.
At Addiction Helpline America, we connect people with specialized care that addresses these complex needs, often including co-occurring substance use disorders. For a broader look at therapeutic options, explore these Types of Addiction Therapy.
Psychotherapy: The Cornerstone of Antisocial Personality Disorder Treatments
Psychotherapy is the primary treatment for ASPD, but it requires a skilled therapist who can build a trusting relationship while remaining firm and consistent. Therapy focuses on key areas like anger management and impulse control, teaching individuals to recognize triggers and consider consequences before acting.
- Cognitive Behavioral Therapy (CBT) is widely used to help individuals identify and challenge the distorted thinking that justifies harmful behavior (e.g., “Rules don’t apply to me”). CBT has been shown to be effective in reducing aggression and substance use.
- Dialectical Behavior Therapy (DBT), adapted from its use in BPD, teaches practical skills for emotional regulation and impulse control. It focuses on mindfulness, distress tolerance, and interpersonal effectiveness to help manage intense feelings and communicate more constructively.
- Mentalization-Based Treatment (MBT) helps individuals understand their own and others’ behavior in terms of underlying mental states (thoughts, feelings, intentions). Research shows promise for MBT, especially when ASPD co-occurs with Borderline Personality Disorder.
Medication Management in Antisocial Personality Disorder Treatments
While there are no FDA-approved medications specifically for ASPD, medication plays a crucial role in managing co-occurring conditions and specific symptoms.
- Mood stabilizers (e.g., Lithium, Carbamazepine) can help reduce impulsivity, aggression, and mood swings.
- Antipsychotics may be used to manage severe aggression or violent behaviors.
- Antidepressants (SSRIs) can treat co-occurring depression and anxiety and may also help with impulsivity and anger.
Anti-anxiety medications like benzodiazepines are generally avoided due to a high risk of abuse and dependency. All medication plans require careful monitoring by a healthcare professional. If you’re dealing with co-occurring depression, we offer a guide on Depression Treatment.
The Role of Holistic and Residential Programs
For individuals with severe ASPD, especially those with co-occurring substance use or legal issues, structured environments like residential programs can be transformative. These settings provide the intensive support and consistent boundaries needed for behavioral change.
Therapeutic communities are long-term residential programs where the community itself is part of the treatment. Clients follow a structured routine of therapy and vocational training, learning responsibility and accountability within a peer group.
At Addiction Helpline America, we advocate for comprehensive approaches. We can connect you with Holistic Drug Rehab options and provide information on In Patient Rehab for Depression for those needing immersive support. We connect people with programs nationwide that provide the structured environment where change is possible.
Challenges, Complications, and Co-Occurring Conditions
Living with or caring for someone with ASPD is incredibly difficult. The disorder creates numerous barriers for the individual, their families, and even healthcare providers.
The biggest obstacle is anosognosia, or a lack of insight. Most people with ASPD don’t believe their behavior is a problem, which explains their reluctance to seek help. They typically enter antisocial personality disorder treatments only when forced by external pressures like a court order or family ultimatum.
The connection to substance abuse is staggering: up to 90% of people with ASPD also struggle with addiction. The impulsivity of ASPD leads to substance use, which in turn worsens every symptom, creating a vicious cycle. This is why dual diagnosis treatment is often necessary.
Legal system involvement is common, with studies showing up to 80% of male inmates meeting criteria for ASPD. Furthermore, stigma within the medical community can be a barrier, as some providers struggle to work with manipulative behaviors and a lack of remorse, hindering the therapeutic process.
Associated Health Risks and Complications
The consequences of untreated ASPD are severe and wide-ranging:
- Physical Safety: Impulsivity and aggression lead to frequent accidents, fights, and injuries.
- Violence and Suicide: The risk of violence, both toward others and self-directed, is high. Suicide attempts are common, especially when combined with substance abuse.
- Instability: Consistent irresponsibility makes holding a job difficult, often leading to chronic unemployment, debt, and homelessness.
- Relationships: Manipulation and lack of empathy make genuine connection nearly impossible, resulting in broken family ties, failed romantic relationships, and profound isolation.
- Physical Health: Reckless behavior increases the risk of sexually transmitted infections like HIV. General self-neglect allows chronic health conditions to worsen.
- Substance Use Disorders: Addiction is a primary complication, compounding every other risk. Understanding the warning signs of relapse is critical for families.
With the right support and structured treatment, many of these complications can be reduced or prevented.
Prognosis, Recovery, and Support Systems

While ASPD is a lifelong condition with no “cure,” antisocial personality disorder treatments focus on management and symptom reduction, and many people experience meaningful improvement over time.
Research shows that symptoms often improve with age, with the most volatile behaviors peaking between ages 20 and 40 before diminishing. Studies report remission rates from 12% to 27%, often linked to stabilizing factors like stable employment and committed relationships. Many individuals eventually learn to avoid harmful behaviors to escape negative consequences, a pragmatic shift that still represents progress.
Coping Strategies for Individuals and Families
For individuals in treatment, developing practical skills is key. This includes learning to recognize emotional triggers, setting personal boundaries, practicing non-manipulative communication, and finding healthy outlets for stress.
For families, who often bear the heaviest burden, the following strategies are essential for survival and well-being:
- Set Clear, Consistent Boundaries: Decide what behaviors you will not tolerate, communicate these limits, and enforce consequences every time.
- Understand the Disorder: Recognizing that the behaviors stem from a mental health condition can help you respond more strategically. Guidance on helping someone with a personality disorder from trusted mental health resources can offer valuable perspective.
- Prioritize Personal Safety: If there is any risk of physical or severe emotional harm, seek professional intervention immediately. Your safety is paramount.
- Join Support Groups: Connecting with others who share your experience provides validation, practical advice, and a reminder that you are not alone.
- Practice Self-Care: Dealing with a loved one with ASPD is emotionally draining. Make time for your own therapy, hobbies, and supportive friendships to maintain your own strength.
Latest Research and Future Directions
The field of antisocial personality disorder treatments is continually evolving. Current research focuses on several key areas:
- Neurobiological Research: Brain imaging is helping scientists map the neural pathways involved in empathy and impulse control, opening doors for targeted interventions.
- Epigenetics: This field explores how early life experiences can influence gene expression, highlighting the importance of early intervention to mitigate risk.
- Targeted Therapies: Researchers are refining approaches like Mentalization-Based Treatment (MBT), which shows promise in helping individuals with ASPD develop better interpersonal understanding.
- Dimensional Models: Psychiatry is moving toward viewing personality traits on a spectrum rather than as rigid categories, which may lead to more personalized treatments.
Each advance brings us closer to more effective interventions. At Addiction Helpline America, we stay current with these developments to connect people with the most evidence-based care available.
Frequently Asked Questions about ASPD Treatment
Here are straightforward answers to the most common questions about ASPD treatment.
Can a person with ASPD be cured?
No, there is no “cure” for ASPD, as it is a deeply ingrained personality structure. However, this does not mean there is no hope. The goal of antisocial personality disorder treatments is management and remission of symptoms. Long-term treatment can help individuals manage their behaviors, improve relationships, and build a more stable life, with many experiencing significant symptom improvement after age 40.
What is the most effective therapy for antisocial personality disorder?
Cognitive Behavioral Therapy (CBT) is one of the most effective and widely used therapies. It directly addresses the distorted thought patterns and harmful behaviors of ASPD. Other promising approaches include Mentalization-Based Treatment (MBT), which helps improve empathy and interpersonal functioning, and Dialectical Behavior Therapy (DBT), which teaches skills for emotional regulation and distress tolerance. The best approach often combines therapies and is delivered by an experienced clinician.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Why is ASPD so difficult to treat?
ASPD is challenging to treat primarily because individuals with the disorder often lack insight into their condition (anosognosia) and do not believe they have a problem. This means they rarely seek help voluntarily. Other challenges include:
- A lack of remorse, which removes a key motivator for change.
- A tendency to be highly manipulative, even with therapists.
- A profound distrust of authority figures and helping professionals.
Effective treatment requires a skilled therapist who can set firm boundaries while building a working therapeutic alliance.
At Addiction Helpline America, we understand these complexities and connect individuals with programs equipped to handle them, especially when co-occurring with substance use disorders.
Finding Hope and a Path Forward
Living with or loving someone with antisocial personality disorder is a difficult journey, but there is genuine hope for improvement. While there is no cure, real progress is possible when individuals access the right support and commit to the process.
Managing ASPD is a lifelong endeavor. Evidence-based antisocial personality disorder treatments, like Cognitive Behavioral Therapy and Mentalization-Based Treatment, can significantly reduce harmful behaviors and help individuals build more stable lives. Medication can also provide crucial support for co-occurring conditions like depression or anxiety.
Early intervention is our most powerful tool. If you notice signs of conduct disorder in a child—such as persistent lying, cruelty, or lack of remorse—seeking a professional evaluation can alter their life’s trajectory and potentially prevent the development of ASPD.
For families, setting firm boundaries and seeking your own support is not selfish; it is essential for your well-being. You cannot change someone who does not see a need for change, but you can protect yourself and make informed decisions.
At Addiction Helpline America, we understand the intersection of personality disorders and addiction. Finding the right treatment program can feel overwhelming, which is why we are here to provide free, confidential guidance.
Whether you are seeking help for yourself or a loved one, professional support is available now. We can help you understand your options and connect you with treatment programs across our network in Arizona, California, Colorado, Florida, and beyond. You do not have to steer this alone.
Find professional help today. Everyone deserves the chance at a more stable life, and the journey forward can begin with a single call.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.















