
When you first suspect a loved one is struggling with addiction, it feels like the ground is shifting beneath your feet. It’s a lonely and confusing time, tangled with fear, frustration, and a profound sense of helplessness. The person you know and love starts to disappear behind a wall of secrets and behavior you no longer recognize.
Helping them starts with recognizing the subtle, painful signs. But it also means understanding that you are not alone in this. This is about moving from worry to compassionate action learning about the disease, preparing for tough conversations, and finding professional support for both of you. It’s a marathon, not a sprint, and the goal is support, not control.
Understanding Addiction and Its Impact on Your Loved One

Right now, your job isn’t to be a detective or a doctor. It’s to build a foundation of understanding. This is what allows you to see the situation with more clarity and compassion, shifting your mindset from crisis mode to one of informed concern.
Recognizing the Behavioral and Emotional Shifts
Addiction rarely happens overnight. It’s more like a gradual slide, marked by small but meaningful changes. You might notice things that, by themselves, don’t seem like a big deal. But when you start connecting the dots, a troubling pattern can emerge.
These aren’t just “bad habits.” They’re often signs that something much deeper is going on.
- Unexplained Financial Problems: Is your loved one constantly short on cash? Are they borrowing money without good reason, or have valuables started to go missing? Addiction is expensive, and financial instability is often one of the first and most obvious signs.
- Changing Social Circles: Have they dropped lifelong friends for a new crowd? Are they suddenly avoiding family events or any situation where they can’t use their substance of choice? This kind of self-isolation is a major red flag.
- Growing Secrecy and Defensiveness: Do simple questions like “Where have you been?” trigger an angry or evasive response? Someone struggling with addiction often builds a fortress of lies to protect their use.
“Addiction is a disease of isolation—both for the person using and for the family that loves them. Realizing you’re part of a much larger community facing this challenge can be the first step toward finding your own strength.”
The need to help has never been more critical. The UN Office on Drugs and Crime’s 2025 World Drug Report found that around 316 million people used illicit drugs in 2023. That’s a staggering 20% increase since 2013 and represents nearly 6% of the global population aged 15-64. The most common substances were cannabis, opioids, and amphetamines. You can find more details in the World Drug Report 2025 insights.
Looking Beyond Checklists to See the Whole Picture
While symptom lists are helpful, it’s vital to look at the whole person. Addiction doesn’t just exist in a vacuum; it touches every part of someone’s life, creating a domino effect of negative consequences.
The table below summarizes some of the interconnected shifts you might see. These are just indicators, not definitive proof, but they can help you see the broader impact beyond just the substance use itself.
Common Changes Associated with Substance Use
| Area of Life | Potential Changes to Observe |
|---|---|
| Physical Health | Unexplained weight loss or gain, poor hygiene, visible signs of drug use (like track marks or nasal damage), or constant fatigue. |
| Mental & Emotional State | Drastic mood swings, increased irritability, paranoia, anxiety, or a complete lack of motivation and emotional flatness. |
| Work or School | A sudden drop in performance, frequent absences or lateness, losing interest in career goals, or getting fired. |
| Relationships | Picking fights with family, withdrawing from partners or children, and manipulating loved ones to enable their behavior. |
Seeing these patterns isn’t about gathering evidence to win an argument. It’s about arming yourself with knowledge. This understanding is the bedrock on which you can build a more effective, empathetic, and constructive approach to helping them find their way back.
Preparing for a Difficult Conversation About Addiction

Starting a conversation about a loved one’s potential addiction is probably one of the most intimidating things you’ll ever have to do. The fear is real. You worry about triggering a huge fight, saying the wrong thing, or pushing them even further away. I’ve seen this anxiety stop people in their tracks for months, even years.
But a conversation grounded in love and empathy can be the key that unlocks the door to change. This isn’t about staging a dramatic confrontation or winning an argument. It’s about carefully and calmly expressing your concern in a way that can actually be heard. This requires a bit of planning—it can’t be a spontaneous emotional outburst.
Choose the Right Time and Place
Where and when you have this talk matters. A lot. Never, ever bring up your concerns during a high-stress moment, in front of other people, or when either of you has been drinking or using. That’s a surefire recipe for defensiveness and chaos.
Instead, you need to intentionally create a pocket of quiet and privacy.
- Find a neutral, private space where you both feel relatively comfortable and won’t be interrupted. A quiet room in the house or even a walk in a secluded park can work.
- Pick a calm time when you are both rested and clear-headed. Think weekend morning, not right after a brutal workday.
- Make sure you have enough time. This isn’t a conversation to rush through in 15 minutes before someone has to leave. That just adds unnecessary pressure.
The environment you choose sends a powerful message. A calm, respectful setting shows you’re taking this seriously, which can help your loved one feel less attacked and more open to listening.
Gather Specific Examples, Not General Accusations
Walking in with broad, sweeping statements like, “You’re always drunk,” or “You have a serious problem,” will get you nowhere fast. These feel like personal attacks and immediately throw up a defensive wall.
A much more effective approach is to ground the conversation in specific, factual observations. Your goal is to show them how their behavior has affected you. You’re sharing your reality, not delivering a verdict.
Key Takeaway: “You are not a prosecutor building a case against them. You are a loved one sharing your worries. By focusing on specific events and your feelings, you’re presenting a truth they can’t easily argue with.”
For example, instead of a broad accusation, try something like this:
- “I was really worried last Tuesday when you didn’t get home until after midnight and weren’t answering your phone. I was scared something terrible had happened to you.”
- “When I saw that new dent on the car last week, it made me really anxious about your safety when you’re out driving.”
- “I felt so sad and a little embarrassed when you missed our niece’s birthday party. She kept asking where you were, and I didn’t know what to say.”
This approach shifts the focus from their character flaws to their concrete actions and your emotional response. It’s a game-changer. For more in-depth strategies, our complete guide on how to help someone with addiction offers more practical advice on this.
Use “I” Statements to Express Yourself
This is one of the most powerful communication tools you have, not just here, but in any difficult conversation. Using “I” statements lets you own your feelings and express your concerns without pointing a finger of blame. It centers the conversation on your experience, which is much harder for someone to dispute.
Look at the difference. It’s subtle but incredibly important.
| Blaming “You” Statement | Empathetic “I” Statement |
|---|---|
| “You lied to me again about where you were.” | “I feel hurt and find it hard to trust you when I find out you weren’t where you said you’d be.” |
| “You spent all our money on drugs.” | “I get so scared about our finances when I see our savings account is empty.” |
| “You just need to stop this now!” | “I am so worried about your health, and I really want to help you find some support.” |
“You” statements corner people and make them defensive. “I” statements, on the other hand, invite them to see things from your perspective.
Remember, this is all happening against a backdrop of intense social stigma, which makes it incredibly difficult for anyone to admit they need help. While public health campaigns are working to reduce this shame, it’s still a massive barrier. By preparing with empathy and using these communication techniques, you can help lower that barrier within your own family.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Setting Boundaries to Support Recovery, Not Addiction
There’s a fine, often blurry line between helping someone you love and enabling their addiction. It’s so easy to cross that line when you’re driven by fear and a deep desire to protect them. But enabling—unintentionally shielding them from the natural consequences of their actions—often just delays the moment they finally decide to get help.
Setting boundaries is the act of stepping back. It’s not about giving up or punishing them. It’s about protecting your own well-being while creating an environment where recovery starts to look like a better option than continuing to use. This is one of the hardest, yet most powerful, things you can do.
The Difference Between Helping and Enabling
First, you have to get honest with yourself about what your actions are really accomplishing. Are you supporting their health, or are you just making it easier for them to keep using?
It can be a tough pill to swallow, but the distinction is crucial.
- Helping is driving them to a therapy appointment or a support group meeting.
- Enabling is calling their boss with a fake excuse when they’re too hungover to go to work.
- Helping is saying, “I love you, but I can’t give you cash because I’m worried about how it will be spent.”
- Enabling is giving them money for “rent” or “groceries” when you have a gut feeling it’s really going toward drugs or alcohol.
Think of it this way: helping behaviors are focused on their long-term recovery, even if it causes a fight in the short term. Enabling behaviors are all about avoiding conflict right now, but they ultimately just prolong the addiction.
How to Define and Communicate Your Boundaries
Let’s be real: setting boundaries feels awful at first. You might feel guilty, selfish, or terrified of how they’ll react. Those feelings are completely normal. But you have to remember your goal: to stop being a safety net for the addiction.
Here are a few practical boundaries you can start with:
- Financial Limits: Get crystal clear that the bank is closed. You can say, “I love you and I’ll always support you, but I can’t give you any more cash. I’m happy to buy you groceries or pay a bill directly to the company, but I won’t be handing you money anymore.”
- No More Excuses: Stop covering for them. That means no more lying to their employer, their friends, or other family members to clean up their messes. It’s time for them to face the social and professional fallout from their choices.
- A Substance-Free Home: Your home has to be your safe space. A non-negotiable boundary is, “You are always welcome here, but you cannot be in my home if you’re under the influence. I also can’t allow any drugs or alcohol in this house, period.”
“A boundary isn’t a threat or an ultimatum. It’s a calm, clear statement of what you will and will not do. It’s about taking back control of your own actions—the only thing you truly can control in this situation.”
When you lay down these new rules, do it when things are calm, not in the middle of a crisis. Use “I” statements to explain your reasoning. For example, “I feel scared and anxious when I give you money and don’t know where it’s going. For my own peace of mind, I can’t do that anymore.”
It’s also essential to have your own support system. Connecting with others who get what you’re going through is invaluable. You can find incredible strength and guidance in local or online addiction recovery support groups that are specifically for families.
Brace yourself for pushback. They might get angry, try to guilt-trip you, or make promises you’ve heard a thousand times. Stand firm. Consistency is everything. Every time you hold your boundary, you reinforce the message that you support them, but you will no longer support their addiction.
Navigating the Path to Professional Treatment
After having that tough conversation, the next question is almost always, “So, what now?” The road ahead usually leads toward professional help, and honestly, stepping into the world of addiction treatment can feel like trying to read a map in a foreign language. But understanding the different routes to recovery is the most powerful tool you have when helping a loved one.
There’s no one-size-fits-all solution here. Every person’s journey is unique. The real key is matching the level of care to their specific needs, which can range from intensive medical supervision to more flexible community support.
Understanding the Levels of Care
The first step is often detoxification, or detox. This is a medically supervised process built to safely manage the physical symptoms of withdrawal. For substances like alcohol or benzodiazepines, trying to detox without medical help can be incredibly dangerous, sometimes even life-threatening. Detox stabilizes the body, but it’s crucial to remember it’s not a complete treatment—it’s the essential first step before the real therapeutic work can begin.
Once detox is complete, many people transition into a more structured program.
- Inpatient or Residential Rehab: This means living at a treatment facility for a set period, usually from 30 to 90 days. It provides an immersive, structured environment away from the triggers and distractions of daily life. This is often the best choice for someone with a severe addiction, co-occurring mental health disorders, or an unstable home environment.
- Outpatient Programs: These offer a lot more flexibility. Participants live at home and go to therapy sessions and group meetings at a treatment center several times a week. It’s a solid option for people who have a strong support system at home and a less severe addiction, allowing them to keep up with work or school.
But the journey doesn’t just stop after a 30- or 90-day program. Real, long-term recovery is built on a foundation of ongoing support.
“Recovery is a marathon, not a sprint. The goal of initial treatment is to build a foundation of skills and stability. Lasting change requires a long-term commitment to aftercare and community connection.”
Finding Reputable Programs and Support
Let’s be clear: not all treatment centers are created equal. It’s so important to vet facilities carefully. You want to look for state-licensed and accredited programs that use evidence-based therapies like Cognitive Behavioral Therapy (CBT). Be very wary of any center that promises a “cure” or uses high-pressure sales tactics.
Peer support groups are another vital piece of the recovery puzzle. They offer a sense of community and shared understanding that can be incredibly powerful.
- 12-Step Programs: Groups like Narcotics Anonymous (NA) and Alcoholics Anonymous (AA) are available almost everywhere and follow a spiritual model of recovery.
- Secular Alternatives: Groups like SMART Recovery use a science-based approach, focusing on self-empowerment and cognitive skills to manage cravings and behaviors.
This infographic gives a good overview of how to start assessing what kind of help is needed.
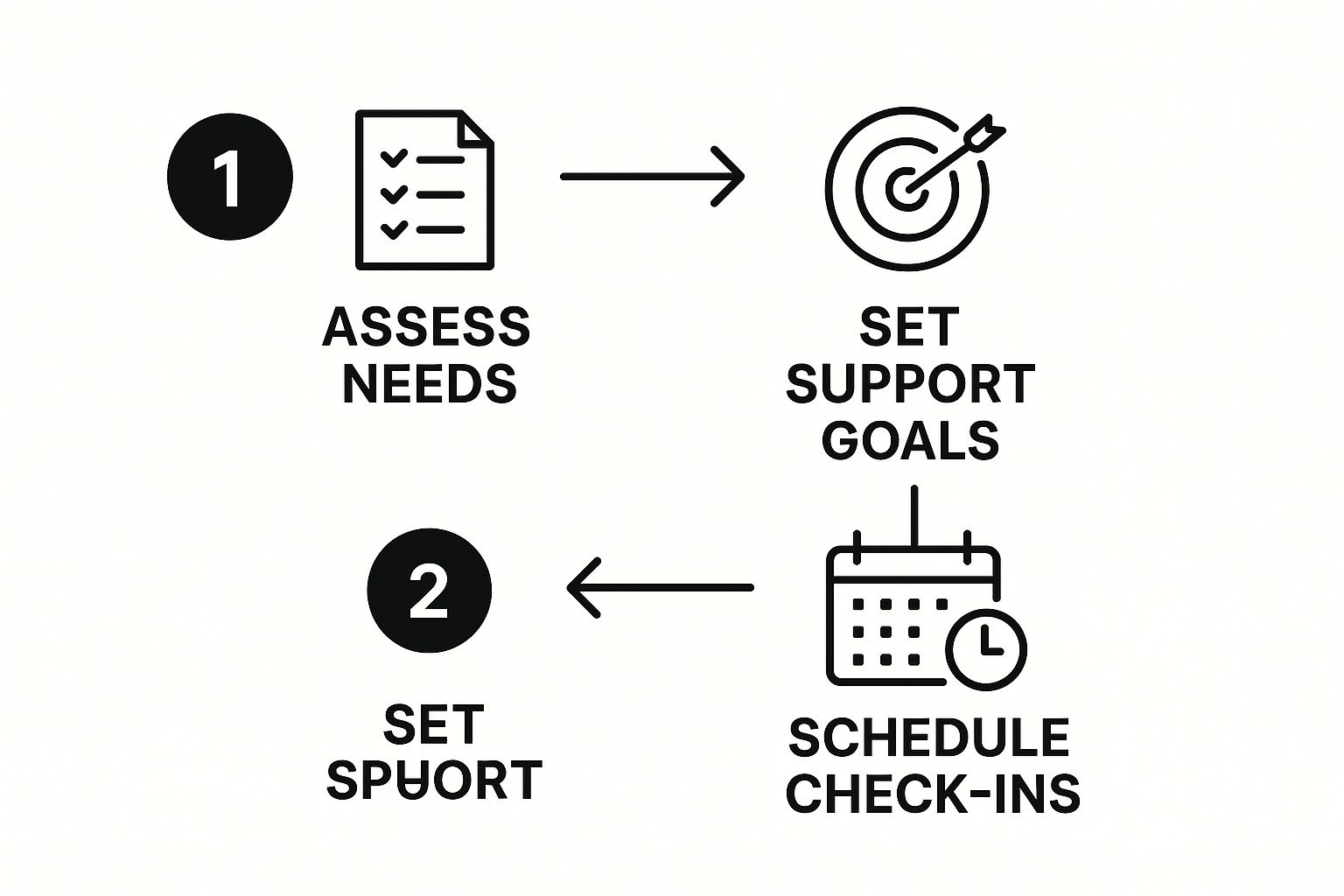
The process really comes down to this: effective support starts with a clear-eyed assessment of what’s needed, followed by setting specific goals and keeping the lines of communication open.
Addressing the Practical Hurdles
Figuring out the money and logistics can feel like a huge challenge. The global drug addiction treatment market is projected to climb from $18.91 billion in 2025 to over $31.20 billion by 2032. That’s a massive number, and it shows just how much recovery depends on organized, and often costly, healthcare systems.
Start by checking your loved one’s insurance policy. Most plans today cover substance abuse treatment, but the details of that coverage can vary wildly. Call the insurance provider directly to get clear answers on deductibles, co-pays, and which facilities are in-network. If there’s no insurance, state and local health departments often fund public treatment programs.
This stage can feel overwhelming, but breaking it down into smaller, manageable steps makes it doable. For a deeper look into this process, check out our guide on how to get addiction help, which has even more resources and guidance. Your role is to help research and present the options, empowering your loved one to take the lead in their own recovery journey.
Why Caring for Yourself Is Essential

Supporting someone battling addiction is a marathon, not a sprint. It’s an exhausting, all-consuming journey that takes an immense emotional, mental, and even physical toll. In the chaos of trying to save someone you love, it’s frighteningly easy to lose yourself. All your energy gets poured into their crisis, and before you know it, your own well-being has completely eroded.
This isn’t just about feeling a little tired. We’re talking about a deep-seated burnout that can leave you anxious, resentful, and utterly depleted. The constant cycle of worry, broken promises, and emotional whiplash can lead to what’s known as compassion fatigue. It’s a very real state of secondary trauma, and it happens to people just like you who are caring for someone in crisis.
If you don’t make a conscious, active choice to care for yourself, you simply won’t have the strength to provide the sustained support your loved one needs. It can feel selfish in the moment, but it’s a strategic necessity.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Moving Beyond Bubble Baths to Real Self-Care
When people hear “self-care,” their minds often jump to bubble baths and face masks. And while those things can be nice, that’s not what we’re talking about here. True self-care in this context runs much deeper. It’s about actively protecting your mental health, reinforcing your own support systems, and finding ways to recharge your own battery so you don’t burn out.
Think of it like the oxygen mask on an airplane. You have to put yours on first before you can effectively help anyone else. This isn’t a luxury; it’s your lifeline.
Here are some practical self-care strategies that actually make a difference:
- Find Your Own Therapist: You are going through a traumatic experience, period. Having a professional, neutral third party to help you process your own feelings of anger, grief, and guilt is invaluable. A therapist can equip you with coping mechanisms and help you reinforce your boundaries without judgment.
- Protect Your Hobbies and Friendships: Addiction has a nasty habit of isolating everyone it touches. Don’t let it cut you off from the people and activities that bring you joy. Keep that coffee date. Go to your yoga class. Read that book. These small acts of normalcy are crucial for reminding you that you have a life and identity outside of this crisis.
- Prioritize Your Physical Health: Stress wreaks havoc on the body. Make a conscious effort to eat nourishing meals, get some form of movement each day, and protect your sleep. These fundamentals are always the first to go when you’re in crisis mode, but they are the very foundation of your resilience.
The Power of Shared Experience
You might feel like you’re the only person in the world going through this. I promise you, you are not alone. One of the most powerful forms of self-care is connecting with others who truly get it. It validates your feelings and gives you a playbook from people who have already walked this difficult path.
“You cannot control their addiction, but you can control how you respond to it. Seeking support for yourself is the first step in shifting from a reactive, chaotic state to one of grounded strength.”
Support groups like Al-Anon and Nar-Anon are designed specifically for the friends and family members of those struggling with addiction. They provide a safe, confidential space to share your story, learn from others, and realize that your feelings are both normal and justified. Finding the right support system for helping family with addiction can be a major turning point for your own well-being.
You Deserve Support Too
Remember, their addiction is not your fault. You didn’t cause it, you can’t control it, and you can’t cure it. Releasing yourself from that impossible burden is an ongoing process, but it is absolutely essential for your survival.
Taking care of yourself isn’t giving up on your loved one. On the contrary, it’s the very thing that will give you the stamina to be there for the long haul, offering the kind of steady, healthy support that actually helps recovery. It is the most loving thing you can do for both of you.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Common Questions About Supporting a Loved One
When you’re in the thick of it, trying to help someone you love, your mind can feel like a constant storm of questions and what-ifs. The path forward is almost never a straight line, and it’s so easy to get lost in the gray areas. I want to walk through some of the most pressing and painful questions families I’ve worked with have faced, offering some direct, experience-based answers to guide you through these incredibly tough moments.
What if My Loved One Refuses to Admit They Have a Problem?
This is, without a doubt, the most common and soul-crushing hurdle you’ll face. Denial is an incredibly powerful defense mechanism, and honestly, it’s a core symptom of addiction itself. When you try to bring it up, your loved one might get angry, defensive, or even try to twist things around to blame you.
The most important thing you can do here is refuse to get into an argument. You simply cannot win a debate against the disease of addiction. Instead, do your best to stay calm and just repeat your concern. Stick with “I” statements like, “I am worried about you,” and hold firm to the boundaries you’ve already set. The goal isn’t to force a tearful confession, but to keep the door open for when they’re finally ready to talk. Focus on the only thing you truly have power over: your own actions and well-being.
“A person’s readiness to accept help can’t be forced. Your role is to be a consistent, loving presence that represents a path to recovery—not a source of conflict. When that small window of opportunity opens, and it often does, you want to be the person they feel safe turning to.”
Is a Professional Intervention a Good Idea?
Interventions can be a powerful catalyst for change, but let’s be clear: they are high-stakes events that can go sideways very quickly if they aren’t handled with expertise. A poorly planned intervention can feel like an ambush, shattering trust and pushing your loved one even deeper into isolation.
A professionally guided intervention isn’t a confrontation. It’s a highly structured and loving conversation. A trained professional leads family and friends as they express their concerns and present a clear, pre-arranged path to treatment. An interventionist is crucial for helping you prepare, script what you need to say, and manage the intense emotions that will absolutely come up.
Consider an intervention if:
- Your loved one is in immediate physical danger.
- All your other attempts to talk have been met with a brick wall.
- You have a clear, pre-arranged treatment plan ready to go the moment they say “yes.”
Before making this decision, it’s smart to look into all the resources for families of addicts. This will help you fully grasp the commitment and intense preparation required.
How Do I Cope if My Loved One Relapses?
Relapse is just gut-wrenching for everyone. It can feel like a complete and total failure, as if every bit of progress has been erased in an instant. It is absolutely crucial to understand that relapse can be a part of the recovery process for many; it is not a sign of moral failure or proof that treatment was a waste of time.
How you respond in this moment is critical. The key is to separate the person you love from their behavior. Reassure them of your unwavering love and support for their recovery while absolutely refusing to enable the substance use. This means holding those boundaries you set—no money, no making excuses for them.
Encourage them to immediately get back in touch with their support system—their sponsor, their therapist, or their treatment provider. This is also the time for you to lean hard on your own support network, whether that’s a therapist, Al-Anon, or friends you can trust. You cannot carry this weight by yourself. Recovery is a long-term journey with brutal ups and downs, and this is just one part of that incredibly difficult road.
When you’re helping a loved one with addiction, it’s easy to feel lost and alone. But you don’t have to navigate this path by yourself. At Addiction Helpline America, we connect you with compassionate professionals who can provide the support and guidance your family needs. If you’re ready to find a path forward, visit us at https://addictionhelplineamerica.com to take the first step.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.















