
The link between bipolar disorder and addiction is something we absolutely have to talk about. These two conditions show up together so often that it creates a really tough situation known as a dual diagnosis. When they co-exist, each one makes the other worse, which can make recovery feel like an uphill battle. This isn’t just a coincidence; it’s a clinical reality that we see every day, driven by some deep, shared roots.
The Tangled Web of Bipolar Disorder and Addiction
When someone is navigating both bipolar disorder and a substance use disorder (SUD), we call it a dual diagnosis or a co-occurring disorder. Imagine trying to steer a ship through a hurricane with a compass that’s spinning wildly. The mood swings of bipolar disorder are the storm, creating incredible internal chaos. Addiction is the broken compass, adding another layer of instability that makes it almost impossible to find your way.
The two conditions create a vicious, self-sustaining cycle. During the intense, energetic highs of a manic episode, inhibitions vanish, often leading to impulsive decisions like drug or alcohol misuse. On the flip side, the crushing lows of a depressive episode can make substances feel like the only way out of the emotional pain. This is a classic case of what we call “self-medication”—a desperate attempt to manage unbearable symptoms.
To quickly grasp the core issues, this table breaks down the essentials of a dual diagnosis involving bipolar disorder and addiction.
Dual Diagnosis At A Glance
| Key Aspect | Description |
|---|---|
| The Connection | Bipolar disorder and substance use disorder (SUD) frequently occur together, creating a “dual diagnosis.” |
| The Cycle | Manic episodes can lead to impulsive substance use, while depressive episodes can drive self-medication to escape pain. |
| Prevalence | An estimated 40-60% of individuals with bipolar disorder also face addiction, a rate much higher than the general public. |
| Treatment | An integrated approach, treating both conditions simultaneously, is the most effective path to recovery. |
This snapshot really highlights why we can’t look at these conditions in isolation. The high rate of comorbidity isn’t just a number; it represents real people facing immense challenges.
The Real-World Impact
The overlap between bipolar disorder and addiction is a major public health issue, not a fringe problem. The numbers truly paint a stark picture of just how intertwined these two are.
“It’s a sobering fact: research consistently shows that somewhere between 40% and 60% of people with bipolar disorder will also struggle with a substance use disorder during their lifetime.”
This is a massive leap compared to what we see in the general population, and it has serious consequences. When both conditions are at play, individuals are more likely to be hospitalized, relapse more often, and experience poorer health outcomes overall. It makes it crystal clear that a specialized approach to treatment isn’t just a good idea—it’s essential. Simply treating the addiction while ignoring the bipolar disorder (or vice versa) is like trying to fix only one-half of a broken machine. It just doesn’t work.
Why You Can’t Treat Them Separately
Because these conditions are so deeply connected, they have to be treated together, at the same time. This is the whole idea behind integrated treatment, which is widely recognized as the gold standard for anyone with a dual diagnosis.
An integrated approach brings together a team of professionals who get the complexities of both mental health and addiction. They collaborate on a single, unified treatment plan that looks at the whole person. This typically includes:
- Medication Management: Carefully selecting mood stabilizers and other medications that support mental stability without clashing with sobriety goals.
- Targeted Therapy: Using therapies like CBT or DBT that build skills for managing both mood swings and substance cravings.
- Robust Support: Building a strong support network of family, friends, and peers who understand the unique challenges of a dual diagnosis.
Successfully managing both conditions is the only way to achieve lasting stability and wellness. For anyone looking for help, there are specialized programs built to handle this very complexity. You can find out more about what to look for by checking out our guide on dual diagnosis rehab centers. This integrated strategy gives people the best possible chance to finally break the cycle and build a solid foundation for a healthier life.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Recognizing the Warning Signs of Dual Diagnosis
Trying to spot a dual diagnosis of bipolar disorder and addiction can feel like trying to untangle two different colored threads that have been tightly woven together. The symptoms of one condition often overlap with, hide, or even mimic the symptoms of the other. It creates a genuinely confusing picture for everyone involved.
For example, is a sudden, wild spending spree a classic sign of a manic episode? Or is it being fueled by the impulsivity that comes with a cocaine high? This is the central challenge: figuring out what’s causing what. The deep fatigue and hopelessness of a depressive episode look almost identical to the crash that follows heavy stimulant use. On the flip side, the rapid-fire speech, racing thoughts, and seemingly endless energy of mania can easily be mistaken for the effects of drugs like methamphetamine. Without seeing the full picture, you’re only getting half the story.
Behavioral Red Flags to Watch For
Often, the first clues that something is wrong show up in a person’s behavior and lifestyle. These shifts can be subtle at first, but they typically represent a major departure from who they used to be. Because both bipolar and addiction seriously mess with judgment and impulse control, these warning signs are often amplified.
Keep an eye out for behaviors like these:
- Drastic Swings in Energy and Activity: We’re not just talking about feeling a little tired or peppy. This is a dramatic swing from periods of frenzied, non-stop activity (like starting five projects at once on three hours of sleep) to phases of complete shutdown where just getting out of bed feels impossible.
- Increased Impulsivity and Risk-Taking: This can look like reckless spending, gambling sprees, hypersexuality, or dangerous driving. When you add substance use into the mix, these behaviors can escalate quickly and lead to devastating consequences.
- Pulling Away from People and Life: A person might suddenly ghost their friends, drop out of family events, and abandon hobbies they once loved. Sometimes this is a sign of depression, but it can also be a way to hide how much they’re drinking or using.
- Dropping the Ball on Responsibilities: A consistent pattern of failing to show up for work, flunking classes, or neglecting duties at home is a huge red flag. This happens when either a mood episode or substance use makes it impossible to function.
These aren’t just “bad choices.” They are symptoms of an internal storm, a destructive feedback loop where unstable moods and compulsive substance use feed each other.
Emotional and Mood-Related Indicators
Underneath all those behaviors are intense, chaotic emotional shifts. For someone struggling with a dual diagnosis, their inner world can feel like a runaway train without any brakes. The mood swings aren’t just your garden-variety “ups and downs”; they are profound, life-altering shifts.
“The hallmark of this dual diagnosis is often the sheer severity and speed of the mood cycles. While bipolar disorder causes these shifts on its own, substance use acts like gasoline on a fire, making episodes more frequent, more intense, and far less predictable.”
This emotional roller coaster is a critical piece of the puzzle. It creates an internal environment where self-medicating starts to feel like a perfectly logical, even necessary, way to cope. Someone might reach for alcohol to quiet the frantic, racing thoughts of mania, or use opioids to numb the crushing pain of depression.
Physical Signs and Symptoms
Finally, the combination of bipolar and addiction takes a heavy toll on the body. These physical signs can sometimes be the most obvious indicators that something is wrong, especially if the person is trying to hide their struggles.
Here are some common physical warning signs:
- Extreme Changes in Sleep: This can mean both insomnia (very common during mania) and hypersomnia, which is sleeping excessively (often seen in depression or during the crash from substance use).
- Significant Weight Fluctuation: Both bipolar episodes and active addiction wreak havoc on appetite, often leading to noticeable weight gain or loss in a short period.
- Signs of Drug or Alcohol Use: Sometimes the evidence is physical, like finding paraphernalia, smelling alcohol on their breath, or noticing things like persistently bloodshot eyes, dilated pupils, or track marks.
- Deterioration in Personal Hygiene: A noticeable decline in self-care and grooming is a classic sign of both severe depression and advanced addiction.
Recognizing how these signs connect is the first, most important step. It’s not about diagnosing someone yourself. It’s about seeing the pattern and understanding that these issues are deeply intertwined and require compassionate, integrated professional help to unravel.
Why These Two Conditions So Often Coexist
It’s no accident that bipolar disorder and addiction are so often found together. This powerful connection isn’t just a coincidence; it’s a complex relationship woven from biology, psychology, and personal experience. To truly help someone struggling with both, we first have to understand why they’re such common partners.
The most straightforward explanation is the self-medication hypothesis. It’s a simple concept with profound implications.
Think of living with bipolar disorder as being on a ship in the middle of a volatile ocean. During a manic episode, you’re caught in a violent storm, tossed about by towering waves of frantic energy, racing thoughts, and overwhelming impulses. To stop the ship from capsizing, you might desperately reach for anything that brings a sense of calm, like alcohol or sedatives.
Then, the storm passes, and you’re plunged into a depressive episode. Now, the ship is adrift in a dead calm, surrounded by a thick, suffocating fog of hopelessness. To feel anything—to try and catch a gust of wind to move forward—you might turn to stimulants. This is self-medication in action. It’s not about getting high for fun; it’s about using substances as a desperate tool to survive the unbearable extremes of the illness.
This visual helps illustrate the core relationship between bipolar disorder, substance use, and their shared risk factors.
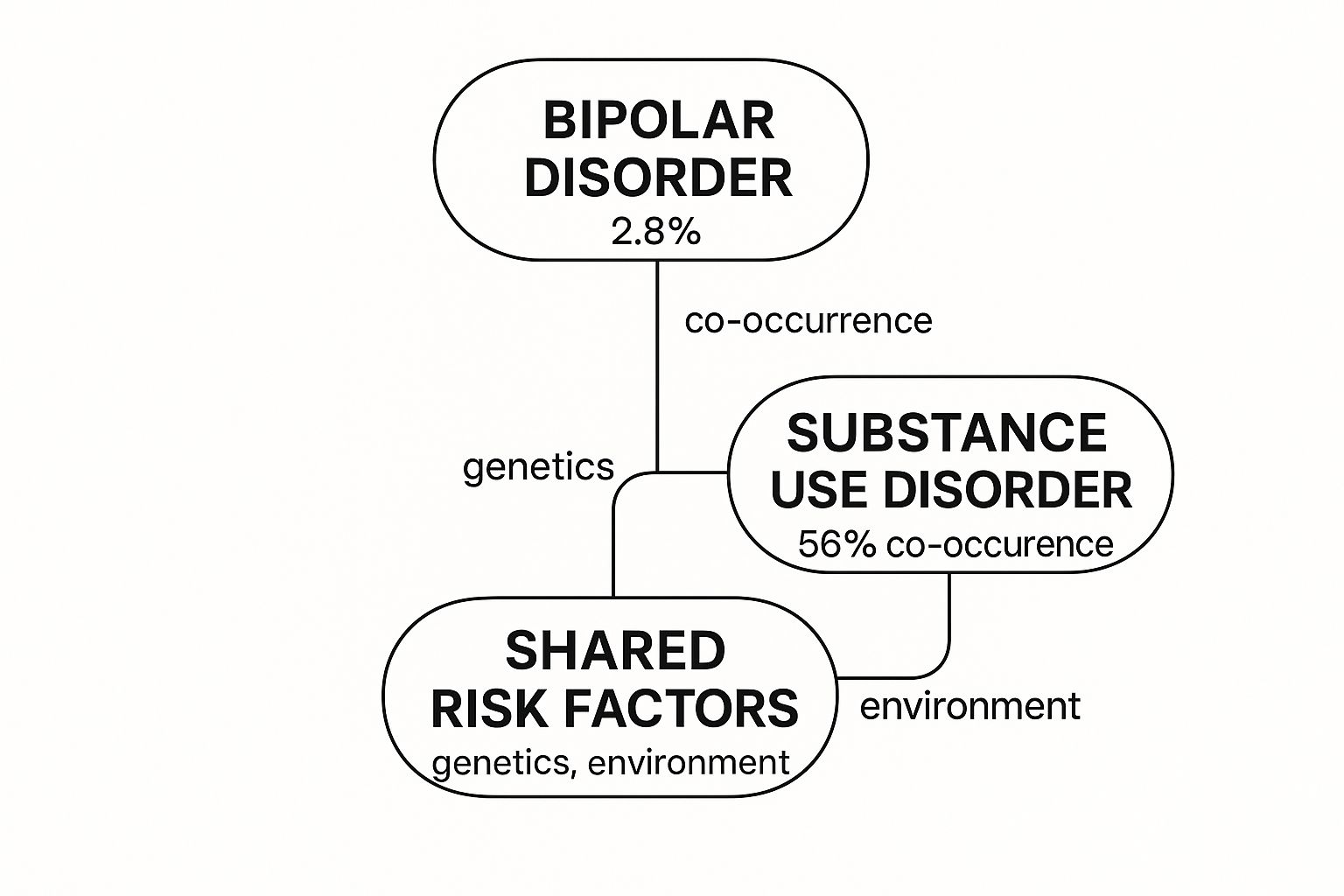
As you can see, the overlap is staggering. With over half of all people with bipolar disorder also facing a substance use disorder, it’s clear these conditions are deeply intertwined.
The Brain’s Hijacked Reward System
Beyond the attempt to self-medicate, what’s happening inside the brain is a major part of the story. Your brain has an internal motivation engine known as the reward system, which runs on a chemical called dopamine. This system is what makes you feel pleasure and encourages you to repeat behaviors essential for survival, like eating a good meal or connecting with loved ones.
Unfortunately, both bipolar disorder and addiction can hijack this delicate system.
- During Mania: A manic episode naturally floods the brain with dopamine. This creates an intense, euphoric high, driving a person to seek even more stimulating experiences—including drugs or alcohol, which push that dopamine surge even further.
- During Addiction: Substances work by artificially overwhelming the reward system with dopamine. This creates a powerful, addictive rush that the brain is hardwired to chase again and again.
This feedback loop is incredibly dangerous. The brain starts to confuse the artificial highs from substances with the natural-feeling highs of mania, blurring the lines between them. The reward pathways become unbalanced, making it hard to find pleasure in everyday life and intensifying the cravings for the extreme rush that only the combination of bipolar and addiction seems to provide.
“The consequences of this destructive interplay are severe. The combination of bipolar disorder and a co-occurring addiction creates a much riskier clinical picture, significantly increasing the likelihood of negative outcomes.”
This is precisely why treating one condition while ignoring the other is so often ineffective. It leaves the brain’s reward system unbalanced and wide open for relapse.
Shared Biological Blueprints
The link goes even deeper, right down to our genes. Research increasingly suggests that some people have shared genetic pathways that make them more vulnerable to both bipolar disorder and substance use disorders. It’s like having two different architectural blueprints for a building. If both plans have the same flaw in the foundation’s design, the final structure is at risk of collapsing from two different directions.
In the same way, certain genetic markers can affect brain regions responsible for:
- Impulse Control: A shared vulnerability can make it harder to resist both the impulsive behaviors of mania and the compulsion to use substances.
- Emotional Regulation: Difficulty managing intense emotions is a hallmark of bipolar disorder and a primary driver for turning to substances to cope.
- Stress Response: A heightened sensitivity to stress can act as a trigger for both mood episodes and substance cravings.
This genetic overlap doesn’t guarantee a dual diagnosis. It just means some people start with a higher level of vulnerability. When that biological predisposition runs into environmental triggers—like trauma, chronic stress, or early exposure to drugs and alcohol—the risk of both conditions developing together skyrockets.
This perfect storm, where bipolar and addiction take hold together, creates a serious health crisis. People facing this dual diagnosis are twice as likely to attempt suicide and often require more frequent hospitalizations. You can learn more by looking at these bipolar disorder and addiction statistics on therapyroute.com. When the stakes are this high, understanding the full scope of the problem is the first, most critical step toward finding a real, lasting solution.
Finding Your Way: Effective Treatment for Bipolar Disorder and Addiction

When you’re dealing with both bipolar disorder and addiction, you need a roadmap that treats both conditions as one. It’s a common mistake to tackle them separately, but that rarely works. Trying to fix one while ignoring the other is like bailing water out of a boat with two holes, but only plugging one—you’re still going to sink. The most effective approach, hands down, is what we call integrated treatment. This means your mental health and addiction specialists aren’t in separate corners; they’re working together as a single, coordinated team.
This unified strategy is crucial because these two conditions are so deeply tangled. The mood episodes from bipolar disorder can easily trigger substance use, and in turn, that substance use can make the mood swings far worse. The only way to truly break free from this vicious cycle is with a plan that understands and addresses this connection, creating a solid foundation for real, lasting recovery.
The Central Role of Integrated Therapy
Therapy is the bedrock of any successful dual diagnosis program. But it has to be the right kind of therapy. We need approaches specifically built to handle the powerful emotions and destructive thought patterns that fuel both bipolar disorder and addiction.
Two of the heavy hitters in this arena are Dialectical Behavior Therapy (DBT) and Cognitive Behavioral Therapy (CBT).
- Dialectical Behavior Therapy (DBT): Though first created for borderline personality disorder, DBT has turned out to be a game-changer for people with a dual diagnosis. It’s intensely practical, focusing on teaching four core skills: mindfulness, distress tolerance, emotional regulation, and interpersonal effectiveness. For someone whose overwhelming feelings often spark cravings, these skills aren’t just helpful; they’re life-saving.
- Cognitive Behavioral Therapy (CBT): This approach helps you learn how to spot, question, and ultimately change the negative thinking that drives unhealthy actions. For instance, you might learn to catch the automatic thought, “I can’t cope with this feeling unless I have a drink,” and actively replace it with a more empowering belief and a solid plan for what to do instead.
These therapies go beyond just talking. They’re about building a real-world toolkit of skills you can pull out and use anytime to manage your moods and protect your sobriety.
Medication Management: A Delicate Balance
While medication is vital for managing bipolar disorder, using it in the context of a dual diagnosis is a delicate balancing act. The goal is always to stabilize mood swings without using medications that carry a risk of abuse or could interfere with addiction recovery. This requires a psychiatrist who has deep experience treating co-occurring disorders.
Mood stabilizers are typically the first line of defense. Medications like lithium or certain anticonvulsants work to level out the dizzying highs of mania and the crushing lows of depression. When those extremes are less severe, the urge to self-medicate often diminishes right along with them.
“A core principle of integrated care is that stabilizing the mood disorder first makes addressing the addiction significantly more manageable. Once someone isn’t constantly battling their own brain, they finally have the mental and emotional energy to fully commit to their recovery work.”
Antidepressants can also be part of the plan, but they’re used with great care. Without a mood stabilizer, they can sometimes trigger a manic episode in someone with bipolar disorder. Every decision about medication is highly personalized, carefully considering a person’s unique symptoms, their history with substance use, and their overall health.
Comparing Treatment Approaches For Dual Diagnosis
To truly grasp how these different components work together, it helps to see them side-by-side. Think of it as a toolbox—each therapeutic method provides a unique and essential tool for someone navigating the complexities of bipolar and addiction.
| Treatment Approach | Primary Focus | Key Benefit for Dual Diagnosis |
|---|---|---|
| Integrated Treatment | Addressing both bipolar disorder and addiction simultaneously with a single, unified team. | Prevents conflicting treatments and addresses the root causes of the self-reinforcing cycle. |
| Cognitive Behavioral Therapy (CBT) | Identifying and changing negative thought patterns and their resulting behaviors. | Helps break the link between depressive thoughts and self-medication or manic impulses and substance use. |
| Dialectical Behavior Therapy (DBT) | Building skills for managing intense emotions, tolerating distress, and improving relationships. | Provides practical tools to handle emotional crises without turning to substances. |
| Medication Management | Using non-addictive medications to stabilize mood and reduce bipolar symptoms. | Reduces the underlying mood instability that often drives the compulsion to use drugs or alcohol. |
This multi-pronged strategy ensures that no part of the dual diagnosis is overlooked. It’s a comprehensive plan built not just to halt destructive behaviors, but to create a life where those behaviors are no longer necessary. By weaving together targeted therapies and precise medication management, individuals get a clear, achievable path toward taking back control and finding genuine, lasting wellness.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Building a Toolkit for Long-Term Recovery
Think of clinical treatment as laying the foundation for a new life. It’s essential, but the real construction happens one day at a time, long after you leave a treatment setting. The work truly begins as you re-enter the flow of daily life, and success hinges on building a personal “recovery toolkit”—a set of practical, go-to strategies for managing both bipolar and addiction.
This isn’t about some unrealistic quest for perfection. It’s about creating a sense of structure and learning healthier ways to respond when life inevitably throws you a curveball. Learning to stay sober while managing a mental health condition is like mastering any new skill: it takes practice, a healthy dose of patience, and the right tools for the job.
Creating a Routine as Your Anchor
When you’re navigating a dual diagnosis, predictability is your superpower. The chaotic highs and lows of bipolar disorder feed on instability, which is often the very environment addiction creates. A consistent daily routine becomes a powerful anchor, keeping you grounded when your internal world feels like a storm.
This routine doesn’t need to be some complex, military-style schedule. It just needs to be reliable.
- Consistent Sleep: Try to go to bed and wake up around the same time every single day, even on weekends. Stable sleep is one of the most powerful non-medical tools for keeping your mood on an even keel.
- Regular Meals: Eating balanced meals at roughly the same times helps stabilize your blood sugar and energy. This has a direct and surprisingly strong impact on both mood and cravings.
- Scheduled Activity: Weaving some movement into your day—a simple morning walk, a trip to the gym, or some evening stretching—is a proven way to boost your mental health.
This simple structure cuts down on decision-making stress and fosters a sense of safety and control, which is incredibly valuable when managing the unpredictability of both conditions.
Identifying Triggers and Planning Ahead
A vital part of your toolkit is a solid relapse prevention plan, and any good plan starts with self-awareness. You have to learn to recognize your own unique triggers—the specific people, places, emotions, or situations that tend to spark a mood episode or an urge to use.
“A trigger is anything that can set off the chain reaction that leads to a relapse. For someone with bipolar disorder and addiction, this could be something internal, like a wave of intense sadness, or external, like running into an old friend you used to drink with.”
Once you know what your triggers are, you can start building a plan to handle them proactively. This might mean setting firm boundaries with certain people or making a conscious choice to avoid specific places. If you’re trying to figure out how to best support a loved one through this, understanding these dynamics is key. Our guide on how to help someone with addiction can offer more insight into creating a supportive home front.
This forward-thinking approach puts you back in the driver’s seat. Instead of just reacting to crises as they happen, you’re actively steering your recovery away from known hazards.
Active Coping Strategies for Daily Resilience
Beyond routine and planning, your toolkit needs active coping strategies for those tough moments. These are the tools you pull out when you feel stressed, overwhelmed, or emotionally raw.
Consider making these powerful techniques part of your daily life:
- Mindfulness and Meditation: These practices aren’t about emptying your mind; they’re about learning to observe your thoughts and feelings without judgment. This creates a critical pause between a trigger and your reaction, giving you the space you need to choose a healthier response.
- Journaling: There’s real power in getting your thoughts out of your head and onto paper. Writing can help you spot patterns in your moods, recognize the early warning signs of an episode, and simply release pent-up feelings in a safe, private way.
- Physical Exercise: The link between moving your body and feeling better mentally is undeniable. Exercise releases endorphins, burns off stress hormones, and improves sleep—making it an essential tool for managing both bipolar symptoms and substance cravings.
Building this toolkit is an ongoing journey of self-discovery. Each new strategy you learn and practice makes you more resilient, more capable, and more confident in your ability to build a life of lasting wellness.
Finding Your Support System for the Journey Ahead

Navigating a dual diagnosis is not something anyone should do alone. Trying to manage both bipolar and addiction on your own is like trying to climb a mountain without a rope or a guide—it’s not just difficult, it’s incredibly dangerous. A strong support system is the gear that keeps you safe and helps you move forward.
This network isn’t something that just magically appears; you have to build it, piece by piece. The foundation is your professional team. This includes therapists, psychiatrists, and case managers who really get co-occurring disorders. They provide the clinical framework for your recovery, offering expert guidance, medication management, and proven therapeutic strategies.
Connecting with Peers Who Understand
Beyond professional help, the value of peer support is immense. There’s a unique sense of validation and belonging that comes from connecting with others who have truly walked in your shoes. It’s a feeling that’s hard to find anywhere else.
Groups like Dual Recovery Anonymous (DRA) are tailor-made for people managing both a mental health condition and substance use. In these meetings, shared experiences build powerful bonds and chip away at the profound isolation that so often accompanies a dual diagnosis. Hearing someone else put your exact struggles into words can feel like a lifeline.
“Connection is a powerful antidote to the shame and secrecy that often accompany bipolar disorder and addiction. When you realize you aren’t alone, the journey immediately feels less daunting and more hopeful.”
Empowering Your Personal Circle
Finally, your own circle of family and friends can be a huge source of strength, but they’ll likely need some guidance. It’s up to you to learn how to communicate your needs clearly and effectively. This means setting healthy boundaries and explaining exactly how they can best support you—which might be very different from what they assume. For a closer look at this dynamic, you can learn more about the importance of support systems in recovery and how to build a healthy network.
When you weave together professional, peer, and personal support, you create a resilient safety net. It ensures that on the tough days, you have multiple places to turn for help, turning your recovery from a lonely battle into a shared journey supported by a community.
Frequently Asked Questions About Bipolar and Addiction
When you’re trying to understand the link between bipolar disorder and addiction, it’s only natural to have a lot of questions. It’s a complex topic, and getting clear answers is the first step toward finding a path forward. Here are some of the most common things people ask, broken down into simple, straightforward explanations.
Can Someone Really Recover From Both at the Same Time?
Yes, absolutely. In fact, tackling both at once isn’t just possible—it’s considered the most effective way to build a strong, lasting recovery.
This approach is called integrated treatment, and it views the two conditions as intertwined, not separate problems. Trying to treat addiction while leaving bipolar symptoms unmanaged (or vice versa) often creates a revolving door. One condition will almost always trigger the other, leading straight back to relapse. A unified plan that combines therapy, support, and the right medication gives you the best shot at a stable, healthy future.
Which Condition Should Be Treated First?
This is one of the most frequent questions we hear, and it comes from a completely understandable place. However, the best practice today isn’t to treat them one after the other. It’s to address them together, right from the start.
“That said, an immediate priority in early recovery is often getting the mood disorder under control. Once bipolar symptoms are stabilized with medication and therapy, those powerful internal triggers—the deep depression or the frantic energy of mania that drive self-medication—start to fade.”
This creates the solid foundation of mental and emotional clarity you need to really dig in and do the hard work of addiction recovery.
Are Certain Substances More Common with Bipolar Disorder?
While a person can become addicted to any substance, some are more common because of how they temporarily seem to “fix” bipolar symptoms.
- Alcohol: This is by far the most common. People often use it to try and quiet the racing thoughts of mania or to numb the crushing weight of a depressive episode.
- Marijuana: Many use it to self-soothe, but it’s a double-edged sword. For some, it can actually make paranoia, anxiety, or even psychosis much worse.
- Cocaine and other stimulants: During a depressive phase, someone might use stimulants to get a boost of energy or a lift in mood. The major risk here is that these drugs can easily kick off a full-blown manic episode.
- Opioids: The intense emotional pain of bipolar depression can lead people to use opioids to simply escape and feel nothing for a while.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
How Can Family and Friends Offer Support?
Supporting a loved one with a dual diagnosis is a marathon, not a sprint. It takes a huge amount of patience, compassion, and—crucially—healthy boundaries.
Your role isn’t to be their therapist, but you can be their biggest ally. Start by educating yourself about both conditions to understand what they’re truly up against. Encourage them to stick with professional treatment and be there to listen without judgment. It’s also vital that you protect your own mental health and get support for yourself through groups like Al-Anon or therapy.
For a wider look at common questions, you can also read through our general addiction FAQs for more helpful insights.
If you or someone you care about is caught in the cycle of bipolar and addiction, please know you aren’t alone and help is available. Addiction Helpline America is here to connect you with compassionate, experienced professionals who understand dual diagnosis. We can guide you to the right treatment and support. Let us help you take that first, brave step toward a healthier life. Find out more at https://addictionhelplineamerica.com.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.















