
Why Your Body Rebels When Alcohol Disappears
Imagine your brain as a thermostat, carefully adjusted over time to keep your internal environment comfortable. Now, picture someone suddenly yanking the settings dial to the extreme. The result? Complete chaos. That’s a pretty good analogy for what happens inside your body during alcohol withdrawal.
Regular alcohol consumption significantly changes your brain’s chemistry. It essentially rewires itself, coming to depend on the presence of alcohol to maintain balance. Think of two key neurotransmitters: GABA, which calms the nervous system, and dopamine, linked to pleasure and reward. With regular alcohol use, their production shifts, relying on alcohol to bridge the gap.
This reliance becomes deeply embedded. When alcohol is suddenly taken away, it’s like an orchestra trying to perform a symphony with half its musicians missing. The calming influence of GABA decreases, while excitatory neurotransmitters, the ones that ramp things up, take center stage.
This isn’t a failure of willpower. It’s pure biology. Your nervous system, used to the suppressing effects of alcohol, goes into overdrive. This surge of activity leads to the many unpleasant, and sometimes dangerous, symptoms that characterize alcohol withdrawal.
This neurochemical upheaval explains why withdrawal can be so intensely uncomfortable. It’s a physiological earthquake, not a personal weakness. Alcohol withdrawal syndrome is a serious public health issue, impacting those who have developed a physical dependence on alcohol over prolonged periods.
According to the National Institute on Alcohol Abuse and Alcoholism (NIAAA), alcohol is the most commonly used substance in the United States. This widespread use significantly elevates the risk of withdrawal for those who reduce or stop their consumption. You can learn more about the prevalence of alcohol dependence here.
Understanding the underlying biological mechanisms at play is critical. Recognizing withdrawal as a medical condition, and not a character flaw, is essential for successful recovery. Several factors influence the intensity of this internal “rebellion”: the amount and duration of alcohol use, individual genetic makeup, overall health, and any previous withdrawal experiences.
These variables determine how strongly your body reacts to this sudden chemical shift. They will also shape your individual experience as you navigate the alcohol withdrawal timeline.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Hours 6-24: When Reality Hits Your Nervous System
Imagine living in a soundproof room for years, then stepping out into the bustling city. The sudden onslaught of noise can be overwhelming. This is similar to what your nervous system experiences in the early stages of alcohol withdrawal. Within 6-12 hours of your last drink, your body, accustomed to the presence of alcohol, begins to react to its absence.
Your nervous system, now on high alert, starts sending out distress signals. That slight trembling in your hands? It’s not weakness, but your brain struggling to regulate motor functions without the sedative effect of alcohol. The creeping anxiety feels different from everyday stress; it’s a direct result of your brain chemistry adjusting.
The withdrawal timeline typically unfolds within 6-12 hours after the last drink, intensifying over the next few days, peaking between 24 and 72 hours. Some symptoms, like hallucinations (visual, auditory, or tactile), can emerge within the first 24 hours. Seizures, a more serious complication, are most common between 24 and 48 hours. You can find more detailed information about the alcohol withdrawal timeline here.
Let’s delve deeper into what’s happening in your brain during these crucial first hours. We’ll explore why symptoms like sweating, nausea, and restlessness appear in this timeframe.
It’s important to distinguish between common early symptoms and more serious warning signs. Recognizing these differences can help you decide when professional medical intervention is necessary.
This isn’t about toughing it out alone. Understanding these early warning signs empowers you to seek help before symptoms escalate. For example, recognizing a hand tremor as a neurological response, rather than a personal failing, can reduce feelings of shame or anxiety.
Knowing what to expect also lessens the fear that can amplify early withdrawal symptoms. This knowledge gives you a sense of control and helps prevent feeling overwhelmed. It’s about understanding the process and making informed decisions about your well-being.
The 48-72 Hour Crucible: When Symptoms Peak
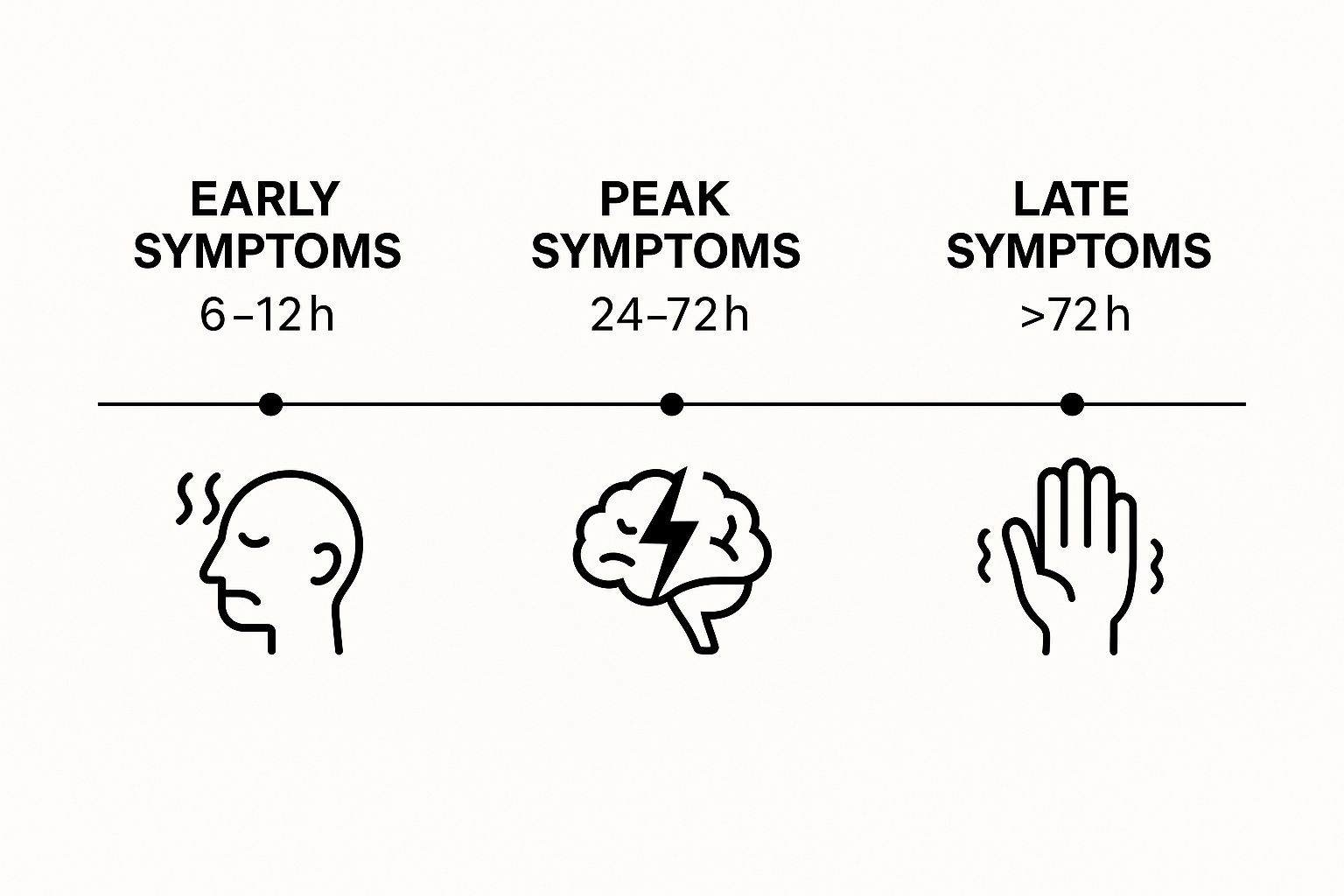
The infographic above gives us a visual roadmap of the alcohol withdrawal timeline. Notice how it highlights the early (6-12 hours), peak (24-72 hours), and late (>72 hours) stages. The 24-72 hour window is clearly marked as the most intense, showing just how critical this period can be.
If the initial withdrawal phase feels like a bumpy plane ride, the 48-72 hour mark is like flying through a hurricane. Without the right support, this is when your body’s fight to regain balance kicks into overdrive, often reaching a frightening peak. Imagine your brain going through a controlled meltdown: neurons misfiring, neurotransmitters scrambled, and your whole nervous system screaming for help.
The intense shaking, drenching sweats, and overwhelming anxiety aren’t signs of weakness. They’re actually a testament to how profoundly alcohol has rewired your brain. This crucial period is also when delirium tremens (DTs), a severe and potentially fatal form of alcohol withdrawal, can appear. Most people experience the worst of it between 24 and 72 hours after their last drink, with DTs often showing up between 48 and 72 hours. Another important statistic to keep in mind is that the most intense symptoms, like delirium tremens, often appear between 48 and 72 hours after the last drink. To understand more about the alcohol detox timeline, take a look at this resource: How Long Does Alcohol Detox Take?.
Why This Peak Is So Dangerous
The intensification of symptoms during this time isn’t random. The sudden absence of alcohol throws your brain’s delicate neurochemical balance completely out of whack. It’s like suddenly pulling a critical support beam out from under a bridge – the whole structure starts to wobble.
This instability shows up as the severe physical and psychological symptoms we associate with peak withdrawal. The risk of seizures, hallucinations, and DTs goes up dramatically during this 48-72 hour window, making medical supervision absolutely essential.
The Importance of Medical Support
Professional medical help during peak withdrawal can truly be a lifesaver. Medical professionals offer critical support in several ways. They can manage severe symptoms with the right medications, closely monitor your vital signs to prevent serious complications, and provide a safe, supportive environment to help you get through this tough time.
With proper monitoring and intervention, what could be a dangerous, even fatal, ordeal becomes a manageable medical process. Professional care turns a potentially life-threatening crisis into a medically supervised journey toward recovery, offering you the stability you need to weather the storm and emerge on a path to lasting sobriety.
To understand more clearly what’s happening during this crucial period, let’s take a look at a breakdown of the typical symptoms:
Peak Withdrawal Symptoms Timeline (48-72 Hours)
A detailed breakdown of the most common symptoms experienced during the peak withdrawal period and their typical onset times
| Symptom Type | Onset Time | Severity Level | Duration |
|---|---|---|---|
| Seizures | 12-48 hours | Moderate to Severe | Minutes |
| Hallucinations | 12-48 hours | Moderate to Severe | Variable, can last hours or days |
| Delirium Tremens (DTs) | 48-72 hours | Severe | Days |
| Confusion and Disorientation | 24-72 hours | Moderate to Severe | Variable |
| Agitation and Restlessness | 24-72 hours | Moderate to Severe | Persistent |
| Increased Heart Rate and Blood Pressure | 24-72 hours | Moderate to Severe | Persistent until medically managed |
| Fever and Sweating | 24-72 hours | Moderate to Severe | Intermittent |
| Tremors | 6-12 hours (increasing severity) | Moderate to Severe | Persistent until medically managed |
| Insomnia | 24-72 hours | Moderate to Severe | Persistent |
This table helps visualize the progression and intensity of withdrawal symptoms during this critical timeframe. As you can see, the 48-72 hour period is marked by the potential onset of the most severe complications, reinforcing the need for professional medical care. Remember, seeking help during this time is not a sign of weakness, but a proactive step towards a safer and more successful recovery.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Days 4-7: Finding Your Sea Legs Again
Imagine a ship navigating calmer waters after weathering a fierce storm. The most intense part of the journey is over, yet the vessel still sways with the residual swell. This is much like the experience of days 4-7 of alcohol withdrawal. The worst of the acute symptoms has likely passed, but the body and mind are still adjusting and healing.
While many individuals experience noticeable improvements during this time, it’s essential to remember that recovery isn’t always a linear progression.
Your brain, now free from the constant influx of alcohol, begins the crucial task of rebuilding neural pathways. These pathways, essential for healthy brain function, may have been dormant or altered for an extended period. It’s like retraining muscles after a long period of inactivity – it takes time and consistent effort. Furthermore, sleep is often still disrupted. This is because alcohol throws off the body’s natural production of melatonin, the hormone that regulates sleep, and it takes time to re-establish a healthy rhythm.
You might experience fluctuating energy levels, feeling exhausted one moment and then inexplicably wired the next. These shifts occur as your metabolism readjusts to functioning without the presence of alcohol. This phase, while generally less intense than the initial days of withdrawal, can be surprisingly challenging due to these lingering effects. It’s common to feel frustrated by the nonlinear nature of healing or to become concerned by unexpected symptom flare-ups. Recovery is rarely a steady upward climb; it’s more like navigating a winding road with occasional bumps along the way.
This stage of alcohol withdrawal also presents unique emotional challenges. Lingering anxiety, persistent sleep disturbances, and waves of emotional volatility are not uncommon. Moreover, it’s during this time that a critical misconception often arises: feeling better doesn’t mean the recovery process is complete. Your brain needs weeks, and sometimes even months, to fully restore its chemical balance after prolonged alcohol use.
This is why continued support and realistic expectations are so vital. Think of recovery like tending a garden. Even after the initial planting, the garden requires consistent care and attention to thrive. Similarly, your recovery journey needs ongoing nurturing and support to solidify the foundation for your long-term well-being. Resources like Addiction Helpline America offer valuable guidance and support during this critical phase and beyond.
When to Call for Backup: Recognizing Medical Emergencies
Knowing when alcohol withdrawal symptoms shift from uncomfortable to truly dangerous is critical. This isn’t about overreacting; it’s about understanding that alcohol withdrawal can, in some cases, be fatal. Certain symptoms demand immediate professional help– think seizures, severe confusion, high fever, and hallucinations. These are not things you should try to manage on your own.
Recognizing the Danger Signs
Imagine your nervous system as the electrical grid powering your body. During alcohol withdrawal, this grid can get overloaded, leading to potentially dangerous power surges. Here are some warning signs that your system is in crisis:
- Seizures: These are a major red flag and require immediate medical attention.
- Hallucinations: Seeing, hearing, or feeling things that aren’t real indicates a serious disruption in normal brain function.
- Severe Confusion or Disorientation: If you or someone you’re caring for becomes increasingly confused, disoriented, or unable to recognize familiar people or places, this signals a dangerous neurological shift.
- Rapid Heart Rate and High Blood Pressure: These can put a significant strain on your heart and other organs, like a motor running at dangerously high speeds.
- High Fever: A fever above 101°F (38.3°C), especially with other withdrawal symptoms, needs urgent medical evaluation.
Delirium Tremens: A Life-Threatening Complication
One of the most serious complications of alcohol withdrawal is delirium tremens (DTs). Think of it as the most severe form of alcohol withdrawal, affecting roughly 3-5% of people withdrawing from alcohol. This condition brings on hallucinations, delusions, confusion, agitation, and potentially fatal issues with the heart and blood vessels. Tragically, if not properly managed, DTs has a fatality rate between 5% and 15%. This underscores the critical importance of prompt medical help for severe alcohol withdrawal. For a more in-depth look at the dangers of DTs and the importance of medical detox, check out this resource: Learn more about alcohol withdrawal and detox.
Levels of Care: Finding the Right Support
Depending on the intensity of your symptoms and your individual risk factors, different levels of care are available, much like choosing the right tool for a specific job. These include:
- Outpatient Monitoring: This option involves regular check-ups with a healthcare provider and is suitable for milder forms of withdrawal.
- Inpatient Detox: This provides 24/7 medical supervision in a hospital or specialized detox facility. It’s essential for those at higher risk of severe withdrawal or complications like DTs.
- Residential Treatment: Following detox, residential programs offer continued support and therapy in a structured, supportive environment. It’s like having a guide and a safe haven as you navigate the early stages of recovery.
Overcoming Barriers to Seeking Help
It’s understandable to encounter obstacles when considering professional help. Common concerns include:
- Cost Concerns: Many insurance plans cover detox and treatment, so it’s worth checking your coverage. Other options include payment plans or sliding-scale fees.
- Stigma: It’s important to remember that addiction is a medical condition, not a personal failing. Seeking help demonstrates strength, not weakness.
- Fear of Judgment: Healthcare professionals are trained to provide compassionate, non-judgmental care. Their goal is to help, not to judge.
Understanding the alcohol withdrawal timeline and recognizing the signs of medical emergencies empowers you to make informed decisions about your health and safety. Don’t hesitate to seek help – it could be life-saving.
What Makes Your Withdrawal Timeline Unique
Just like fingerprints, everyone’s experience with alcohol withdrawal is different. Your personal journey isn’t set in stone; it’s molded by a unique combination of factors. Imagine two individuals: one who has been drinking heavily daily for years, and another whose heavy drinking has been more recent and less frequent. Their withdrawal experiences will be vastly different.
Your age, overall health, and even past attempts at quitting (successful or not) all contribute to your unique withdrawal timeline. Genetics also play a surprising role, influencing how your body reacts to the absence of alcohol. Let’s explore how these individual variables create your personal withdrawal experience, and why your journey may differ drastically from others’ stories.
Factors That Personalize Your Withdrawal
Many factors contribute to the specifics of your withdrawal timeline. Pre-existing mental health conditions, like anxiety or depression, can intensify withdrawal symptoms. Certain medications can also complicate the process. Interestingly, previous withdrawal experiences can actually “prime” your brain to expect more severe symptoms in the future.
This phenomenon, known as kindling, can make each subsequent attempt at quitting more challenging and potentially more dangerous. The length and intensity of alcohol use also plays a significant role. Furthermore, factors like age, past instances of Delirium Tremens (DTs), and liver health can influence the likelihood and severity of withdrawal symptoms. Learn more about these individual factors at The Recovery Village.
To help illustrate how these factors interact, let’s take a look at the following table:
Factors Influencing Withdrawal Severity
Comparison of individual factors and their impact on withdrawal timeline and symptom intensity
| Risk Factor | Low Risk | Moderate Risk | High Risk |
|---|---|---|---|
| Duration of Heavy Drinking | Less than 5 years | 5-10 years | Over 10 years |
| Quantity of Alcohol Consumed Daily | 1-3 standard drinks | 4-7 standard drinks | 8+ standard drinks |
| Previous Withdrawal Attempts | None or one mild episode | Two or more mild episodes, or one moderate episode | Multiple moderate to severe episodes, or history of DTs |
| Age | Under 30 | 30-50 | Over 50 |
| Co-occurring Mental Health Conditions | None | Mild anxiety or depression | Severe anxiety, depression, or other mental health diagnoses |
As you can see, the interplay of these factors paints a clearer picture of individual risk. Someone with a longer history of heavy drinking, coupled with pre-existing anxiety, will likely experience a more intense and prolonged withdrawal than someone with a shorter history and no underlying mental health conditions.
Understanding Your Individual Needs
By understanding these risk factors, you can develop a realistic picture of what your own recovery might look like. This knowledge empowers you to advocate for the level of care you need. It helps you recognize when your situation requires specialized medical intervention, perhaps through a treatment plan specifically designed for your individual risk profile. For instance, someone with a history of seizures during withdrawal will need a different level of care and medical supervision than someone without that history.
This personalized approach is vital for navigating the challenges of withdrawal and sets the stage for long-term success. Knowing what to expect allows you to seek appropriate support at the right time. This turns a potentially overwhelming experience into a manageable one, guiding you toward a healthier, alcohol-free future.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Building Your Recovery Foundation Beyond Detox
Successfully navigating the initial stages of alcohol withdrawal is a major step. It’s like crossing a turbulent river – you’ve reached the other side, but the journey isn’t over. The real work begins with rebuilding on more solid ground. The end of acute withdrawal isn’t the finish line; it’s the starting block of your true recovery.
The Long Game of Recovery
Your brain, after prolonged exposure to alcohol, needs time to recalibrate, sometimes months, even after the initial withdrawal symptoms fade. Think of it like a garden that needs tending after a harsh winter. Post-acute withdrawal symptoms (PAWS) can appear weeks or even months later, bringing unexpected bouts of anxiety, disturbed sleep, and shifting moods. These are like the occasional weeds that pop up – less pervasive, but still disruptive. These lingering symptoms can be tough, so having a strong support system is essential.
Building a Support Network
Recovery is a marathon, not a sprint. Your support network needs to understand that it’s about building a long-term framework for well-being, not just getting through the initial detox. This can involve several elements:
- Finding Healthcare Providers: Look for doctors specializing in addiction medicine. They can offer continued medical care, track your recovery, and adjust any necessary medications.
- Connecting with Peer Support Groups: Groups like Alcoholics Anonymous (AA) or SMART Recovery provide invaluable peer support and shared understanding. Connecting with others facing similar challenges can offer both encouragement and practical tips. Finding the right group for you depends on your individual personality and preferences.
- Involving Family Members: Family can be a tremendous source of support, but they might need guidance on how to best help. Open communication and educating them about the recovery process can turn them into powerful allies.
Identifying Triggers and Developing Coping Strategies
Rebuilding your foundation involves understanding what situations, feelings, or environments trigger your urge to drink. Imagine these triggers as potholes in the road to recovery. Once you identify them, you can develop healthier ways to navigate around them. This could involve mindfulness techniques, exercise, or pursuing hobbies you enjoy.
Rebuilding Confidence and Addressing Psychological Needs
Beyond the physical aspects, there’s the psychological work of rebuilding self-assurance – trusting yourself to handle life’s pressures without alcohol. This often involves professional help to address underlying issues that may have contributed to alcohol dependence. It’s like strengthening the roots of a tree to help it withstand future storms.
Recovery is not simply about enduring withdrawal; it’s about building a life that nurtures your continued health and growth. It’s about designing a fulfilling, sustainable future where alcohol no longer dictates your choices and well-being. It’s about rebuilding, not just surviving.
Are you or a loved one struggling with alcohol addiction and ready to begin the journey to recovery? Addiction Helpline America provides confidential support and resources to help you take the first step. Reach out today at https://addictionhelplineamerica.com and start building your foundation for a healthier tomorrow.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
24/7 Free & Confidential Alcohol Withdrawal Support
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.















