Understanding Withdrawal Symptoms: What You Need to Know
Withdrawal symptoms are the physical and psychological effects that occur when a person stops or reduces their use of a substance their body is dependent on. These symptoms can range from mild discomfort to severe, life-threatening complications.
Quick Overview of Withdrawal Symptoms:
- Physical symptoms: Nausea, sweating, tremors, muscle aches, and seizures.
- Psychological symptoms: Anxiety, depression, irritability, insomnia, and intense cravings.
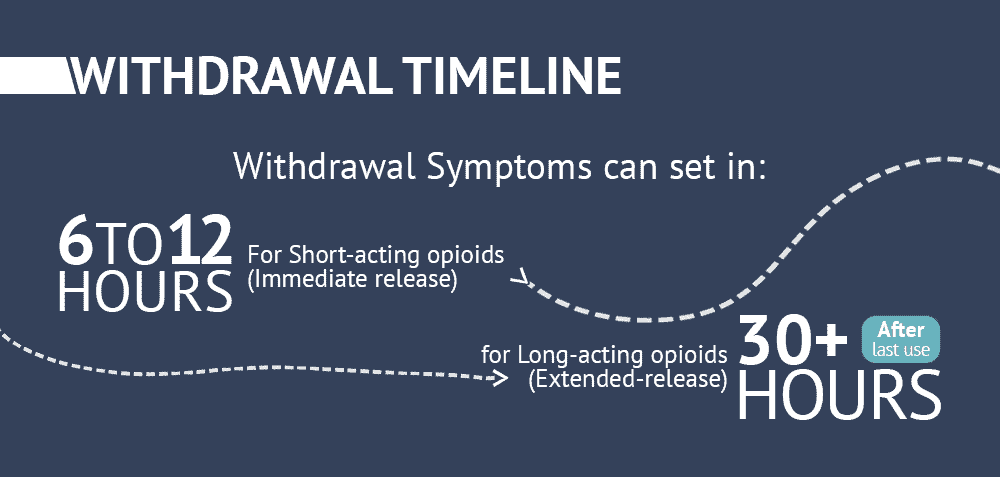
- Timeline: Symptoms typically begin 6-48 hours after the last use and can last for days or weeks.
- Severity factors: The type of substance, duration and amount of use, and overall health.
- Critical point: Withdrawal from alcohol and benzodiazepines can be life-threatening without medical supervision.
When to seek immediate help: Go to an emergency room for seizures, hallucinations, extreme confusion, chest pain, difficulty breathing, or thoughts of self-harm.
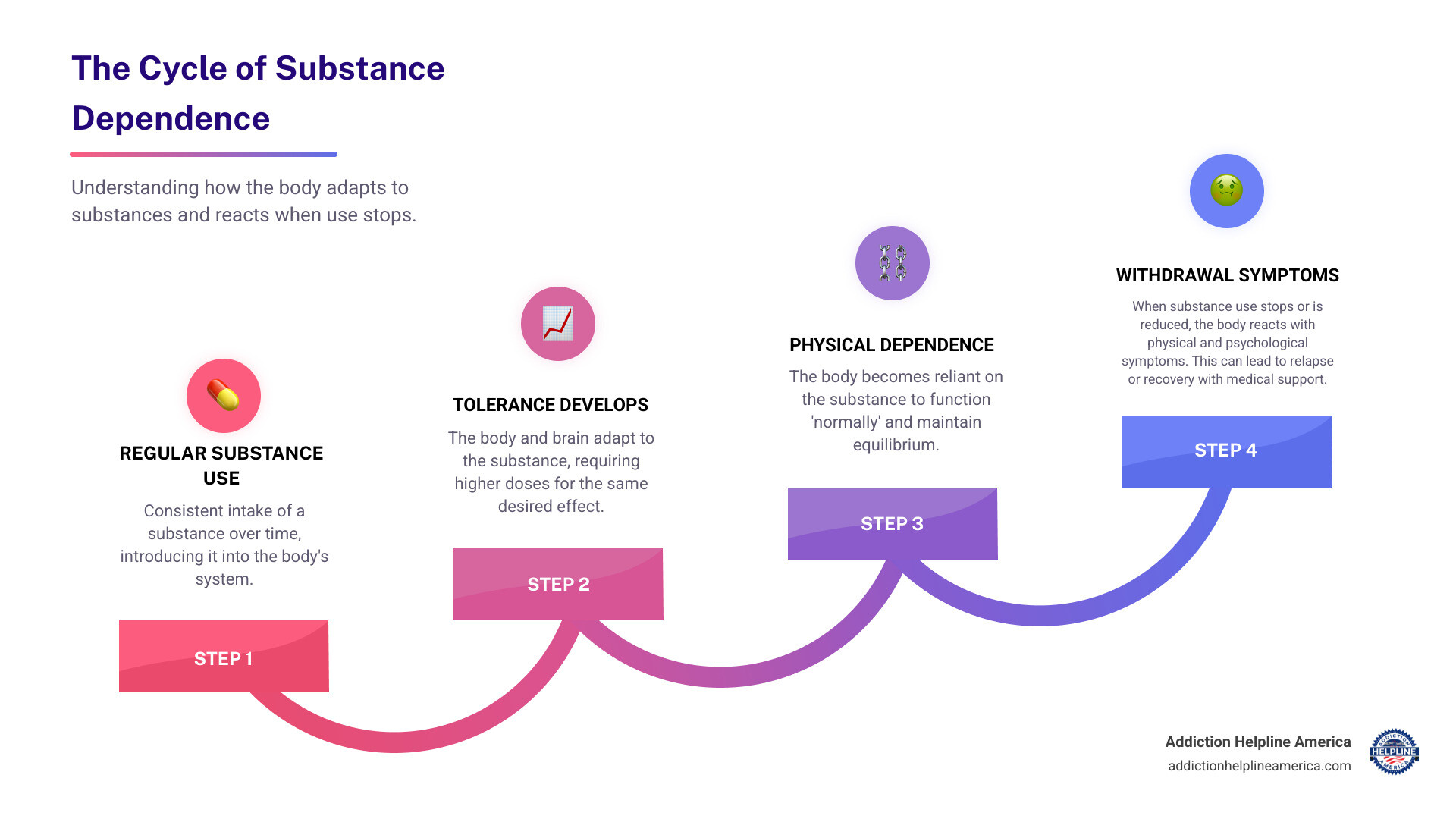
Understanding withdrawal is the first step toward recovery. The process occurs because your body adapts to the presence of a substance and needs time to readjust when it’s removed. This readjustment period causes withdrawal symptoms. The severity depends on both physical dependence (the body’s reliance) and psychological dependence (the emotional patterns tied to use).
Withdrawal can be dangerous. Alcohol and benzodiazepine withdrawal can cause deadly seizures, while opioid withdrawal dramatically increases the risk of a fatal overdose if a person relapses. At Addiction Helpline America, we’ve helped thousands safely manage withdrawal through compassionate guidance and 24/7 support. Our team is here to provide the confidential, personalized assistance you need to take that crucial first step.
Find more about withdrawal symptoms:
What Is Addiction Withdrawal?
When a person dependent on a substance stops or cuts back, their body and mind react with withdrawal symptoms. This process is also known as detoxification or “detox.”
Your body is adaptable. With regular substance use, it adjusts its internal chemistry to function with the substance present. When the substance is removed, the body is thrown off balance and must readjust, causing withdrawal symptoms.
This occurs due to physical dependence, where the body’s biology has changed to accommodate the substance, and psychological dependence, the emotional need to use the substance to cope or feel normal. For example, alcohol is a depressant that slows the brain. Over time, the brain compensates by becoming over-excited. When alcohol is removed, this over-excited state can cause anxiety, tremors, and even life-threatening seizures.
Opioids work differently, blocking pain and boosting pleasure. The brain adapts by reducing its natural production of feel-good chemicals. When opioids are stopped, the person is left with intense discomfort and powerful cravings. This adaptation also leads to tolerance, meaning more of the substance is needed to get the same effect, which makes withdrawal more challenging.
Understanding how substances rewire the brain explains why quitting alone can be difficult and dangerous. For some substances, medical supervision during withdrawal is essential for safety. To learn more about the broader picture of addiction, explore our Drug Addiction Help Guide.
Common Substances Causing Withdrawal
Many substances can cause withdrawal symptoms. The type and severity depend on the drug, duration of use, and individual health.
Alcohol: Withdrawal can be one of the most dangerous. Symptoms include high blood pressure, rapid heartbeat, tremors, hallucinations, and seizures. The most severe form, delirium tremens (DTs), can be fatal without medical treatment. Medical supervision is critical.
Opioids: This includes heroin, fentanyl, and prescription painkillers like oxycodone. Withdrawal feels like a severe flu with muscle cramps, nausea, vomiting, and intense anxiety. The primary danger is the high risk of a fatal overdose if a person relapses after their tolerance has decreased. For more on discontinuing prescription medications, see our resource on Detox From Prescription Drugs.
Benzodiazepines: Drugs like Xanax and Valium can cause dangerous withdrawal symptoms, including severe anxiety, hallucinations, and life-threatening seizures. Never stop taking these medications suddenly; a medically supervised taper is essential.
Stimulants: Cocaine, methamphetamine, and Adderall withdrawal is primarily psychological but can be severe. Symptoms include deep depression, exhaustion, paranoia, and suicidal thoughts. Learn more about Cocaine and Methamphetamine Addiction.
Nicotine: Found in tobacco and vape products, nicotine withdrawal is uncomfortable but not medically dangerous. Symptoms include irritability, trouble sleeping, anxiety, and strong cravings.
Cannabis (marijuana): Heavy, regular users can experience irritability, anxiety, sleep problems, and restlessness when they stop. Symptoms typically last one to two weeks.
Other Prescription Drugs: Some antidepressants and sleep medications can also cause withdrawal if stopped abruptly. Always consult a healthcare provider before stopping any prescribed medication.
Common Withdrawal Symptoms and Timelines
When you stop using a substance, you will likely experience a range of physical and psychological withdrawal symptoms. Understanding what to expect can reduce anxiety and prepare you for the process. The timeline and intensity vary based on the substance, duration of use, and your health. Managing intense cravings during this period is a major challenge and a key reason why medical support is vital to prevent relapse.

Physical and Psychological Withdrawal Symptoms
Physical symptoms are the body’s tangible reactions. Common symptoms include:
- Nausea, vomiting, and diarrhea
- Muscle aches and pains
- Sweating, chills, and tremors
- Headaches
- Increased heart rate and blood pressure
- Insomnia and fatigue
Psychological symptoms affect your thoughts and emotions and can often last longer than physical ones. These include:
- Intense anxiety and paranoia
- Depression, sadness, and hopelessness
- Irritability and agitation
- Difficulty concentrating or “mental fog”
- Rapid mood swings
- Intense cravings for the substance
For those dealing with stimulants, managing these psychological symptoms is especially critical. We offer support for those facing Cocaine and Methamphetamine Addiction.
Severe Symptoms Requiring Medical Attention
Some withdrawal symptoms signal a medical emergency and require immediate professional help. These can be life-threatening.
- Seizures: Can occur suddenly during alcohol and benzodiazepine withdrawal.
- Hallucinations: Seeing, hearing, or feeling things that are not there.
- Delirium Tremens (DTs): The most severe form of alcohol withdrawal, involving confusion, fever, and rapid heart rate. It can be fatal if untreated.
- Psychosis: A severe mental state involving a loss of contact with reality.
- Extreme Agitation: Uncontrollable restlessness and anxiety that can pose a danger.
- Suicidal Thoughts: The psychological pain of withdrawal can lead to thoughts of self-harm. If you are in crisis, call or text the 988 Suicide & Crisis Lifeline at 988, or call 911 immediately.
Attempting to withdraw from alcohol or benzodiazepines at home without medical supervision is extremely risky.
Withdrawal Timelines for Major Substances
The duration of withdrawal symptoms varies, but general timelines can help you prepare.
- Alcohol: Begins 6-24 hours after the last drink, peaks at 36-72 hours (highest risk for seizures/DTs), and the acute phase lasts 2-10 days.
- Short-Acting Opioids (Heroin): Starts in 8-24 hours, peaks in 1-3 days, and acute symptoms last 4-10 days.
- Long-Acting Opioids (Methadone): Starts in 12-48 hours, peaks in 2-4 days, and the acute phase can last 10-20 days.
- Benzodiazepines: Onset is 1-2 days for short-acting types and several days for long-acting ones. Withdrawal is prolonged, with acute symptoms lasting 2-8 weeks or more.
- Stimulants (Cocaine): Begins within 24 hours, peaks around days 3-5, with psychological symptoms like depression and cravings lasting for weeks or months.
Many people also experience Post-Acute Withdrawal Syndrome (PAWS), where psychological symptoms like mood swings, anxiety, and low energy persist in waves for months after acute withdrawal. This is why ongoing therapy and support are crucial for long-term recovery.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Factors Influencing Withdrawal and When to Get Help
No two people experience withdrawal identically. The severity is shaped by a combination of biology, history, and circumstance. Understanding these factors helps you know when professional support is essential.

What Affects the Severity of Withdrawal Symptoms?
The intensity of your withdrawal symptoms depends on several key factors:
- Type of substance: Alcohol and benzodiazepine withdrawal carry risks of fatal complications, while opioid withdrawal is uncomfortable, and stimulant withdrawal is psychologically severe.
- Duration and amount of use: Longer periods of use and higher doses create deeper physical dependence, leading to more intense withdrawal.
- Method of use: Injecting or smoking delivers substances to the brain faster, often resulting in more severe withdrawal.
- Co-occurring mental health conditions: Existing anxiety or depression can be dramatically amplified during withdrawal. Our Inpatient Behavioral Health Complete Guide explores integrated treatment for these cases.
- Age and physical health: A person’s overall health affects their ability to tolerate the stress of withdrawal. Chronic conditions add layers of risk.
- Previous withdrawal attempts: Each withdrawal episode can be more severe than the last, a phenomenon known as “kindling.”
- Polysubstance use: Using multiple substances creates a complex and unpredictable withdrawal profile.
Dangers of Unmanaged Withdrawal
Attempting to detox alone can be deadly. The body’s reaction can quickly spiral into a medical emergency.
- Dehydration and Malnutrition: Severe vomiting and diarrhea can lead to dangerous electrolyte imbalances, risking heart and organ failure.
- Aspiration Pneumonia: If a person vomits while unconscious or during a seizure, stomach contents can enter the lungs, causing serious infection or choking.
- Overdose Risk After Detox: This is a major danger for opioid users. After a period of abstinence, tolerance plummets. If a person relapses and uses their previous dose, it can be fatal. Most opioid overdose deaths occur in people who have recently detoxed.
- Mental Health Deterioration: The psychological distress of withdrawal can lead to severe depression, anxiety, and suicidal thoughts.
- Delirium Tremens (DTs): This severe form of alcohol withdrawal causes confusion, hallucinations, and seizures. Without intensive medical care, it can lead to heart failure and death. Research confirms these alcohol withdrawal complications and the need for medical supervision.
These dangers are manageable with proper medical care. Addiction Helpline America can connect you with professionals who make withdrawal safer and more comfortable. Recovery starts with a safe detox.
Navigating Treatment for Withdrawal Symptoms
Successfully managing withdrawal symptoms through medical detox is the critical first step toward recovery. Detox focuses on safely stabilizing your body, alleviating discomfort, and preventing dangerous complications. It is not a cure for addiction but the necessary foundation for further treatment.
Medical detox often combines Medication-Assisted Treatment (MAT), supportive care, and professional monitoring. The goal is to clear the fog of withdrawal so you can begin long-term recovery planning. Our Addiction Treatment Programs Complete Guide details the continuum of care available after detox.
Where to Receive Withdrawal Treatment
Choosing the right setting for managing withdrawal symptoms depends on the substance, severity of dependence, and your overall health. This decision should always be made with a healthcare professional.
- Outpatient Detox Programs: For those with moderate symptoms and a stable home environment, these programs allow you to live at home while attending scheduled appointments for medical monitoring and medication.
- Inpatient or Residential Detox Centers: This setting provides 24/7 medical supervision and is ideal for those with moderate to severe symptoms, a history of complicated withdrawal, or co-occurring health conditions.
- Hospital Settings: Essential for the most severe cases with a high risk of seizures, DTs, or other acute medical complications, ensuring immediate access to emergency care.
Even if you plan on Virtual Rehab for ongoing care, the initial detox phase often requires in-person medical supervision.
Common Medications and Therapies
Medications are vital for making withdrawal safer and more tolerable. The specific drugs used depend on the substance and your symptoms.
- For Alcohol Withdrawal: Benzodiazepines like diazepam (Valium) are used to calm the nervous system and prevent seizures and DTs.
- For Opioid Withdrawal: Buprenorphine and methadone are key components of MAT. They reduce withdrawal symptoms and cravings without producing a high. Clonidine can also help manage physical symptoms.
- Symptomatic Medications: Other drugs can be used to treat specific symptoms like nausea (anti-emetics), muscle aches (pain relievers), and insomnia (sleep aids).
Cognitive Behavioral Therapy (CBT) is invaluable for addressing the psychological side of addiction. It helps you identify triggers and develop healthy coping skills. Many centers also offer holistic therapies like yoga and meditation to reduce stress and promote well-being. For more, explore our guide on Holistic Drug Addiction Treatment.
Proper nutrition and hydration are also fundamental to supporting your body as it heals. This comprehensive approach paves the way for sustained recovery.
Frequently Asked Questions about Withdrawal
When facing withdrawal symptoms, it’s natural to have questions. Here are answers to some of the most common concerns we hear.
Can withdrawal be fatal?
Yes, withdrawal from certain substances can be life-threatening. This is why professional medical care is essential. Withdrawal from alcohol and benzodiazepines is the most dangerous, as it can lead to seizures or delirium tremens (DTs), a condition with a high mortality rate if untreated. While opioid withdrawal is rarely fatal on its own, the severe drop in tolerance during detox creates a high risk of a fatal overdose if a person relapses.
How long do cravings last after the initial withdrawal period?
While acute physical symptoms usually subside within days or weeks, psychological cravings can persist for months or even years. This is often part of Post-Acute Withdrawal Syndrome (PAWS), where the brain is still healing. Cravings are often triggered by stress, people, or places associated with past use. Ongoing therapy and support groups are crucial for learning to manage these triggers and prevent relapse, forming the foundation for lasting recovery.
Is it safe to detox at home without medical help?
For substances like alcohol, opioids, and benzodiazepines, detoxing at home without medical supervision is extremely dangerous. The withdrawal symptoms can escalate unpredictably into life-threatening medical emergencies like seizures. The intense discomfort also increases the likelihood of relapse. For opioid users, relapsing after a home detox attempt is particularly deadly due to decreased tolerance. Medical detox programs exist to manage these dangers safely with medication, monitoring, and a supportive environment.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
How to Support a Loved One and Find Help
Watching someone you care about struggle with withdrawal symptoms is overwhelming. Your support is crucial, but it must be paired with professional help. Addiction is a disease, and withdrawal is a medical process that requires compassion and patience.
Start by educating yourself and offering non-judgmental support. Listen with empathy and validate their struggle. Avoid lectures or ultimatums, which can push them away. One of the most important things you can do is encourage them to seek professional help for medical detox and ongoing treatment. Offer practical assistance, like helping them research options or make phone calls.
It’s also vital to distinguish between supporting and enabling. Enabling behaviors, like giving money for substances or making excuses, can prolong the addiction. Learn more in our guide on how to support people with drug and alcohol problems.
Supporting someone in recovery is exhausting. Caregiver burnout is real, so you must prioritize your own well-being. Set healthy boundaries to protect your mental health. Their recovery is their responsibility; you can support them, but you cannot do the work for them.
Recovery is possible. At Addiction Helpline America, we’ve seen it happen time and again. We connect individuals and families to a network of treatment centers across all 50 states and the District of Columbia. Whether your loved one needs medical detox, residential treatment, or outpatient support, we can help you find the right program.
Our services are free, confidential, and available 24/7. We provide personalized guidance based on your specific situation. If you or someone you love is struggling, please reach out. The call that feels hardest to make might be the one that changes everything. Find help through addiction and rehab hotlines and take the first step toward recovery today.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.







