
When people ask, “which condition is often a result of alcohol addiction?”, the most direct answer is nearly always liver disease. While chronic drinking wreaks havoc on the entire body, the liver is ground zero. It’s the organ responsible for processing every drop of alcohol, putting it on the front lines and making it incredibly vulnerable to lasting, often permanent, damage.
Understanding Alcohol Use Disorder (AUD)

It’s crucial to understand that alcohol use disorder (AUD) is a legitimate medical condition, not a sign of weak willpower. AUD is defined by an inability to stop or manage drinking despite negative consequences to health, work, or relationships. Diagnosis often involves a healthcare professional evaluating a patient’s drinking habits against a set of criteria, such as experiencing cravings, building a tolerance, or continuing to drink despite causing problems. It’s like a car’s brakes have failed—the desire to stop is there, but the internal mechanism to actually do it is broken.
This isn’t just a bad habit. Alcohol addiction physically rewires the brain’s chemistry, creating an intense compulsion that can easily overpower rational decision-making. Over time, tolerance builds, meaning a person has to drink more and more just to feel the same effects. This creates a dangerous, accelerating cycle of consumption that paves the way for severe physical and psychological harm. To get a deeper look at the mechanics of this disease, our guide to understanding alcohol addiction is a great resource.
The Scope of the Problem: Alcohol Addiction Statistics
The impact of alcohol addiction is a global public health crisis. According to the World Health Organization (WHO), alcohol use is directly linked to an estimated 2.6 million deaths each year. That staggering number represents 4.7% of all deaths worldwide. In the United States, the National Institute on Alcohol Abuse and Alcoholism (NIAAA) reports that nearly 30 million people aged 12 and older had AUD in 2022.
Long-term dependency dramatically raises the risk for a whole host of chronic diseases, from liver cirrhosis and cardiovascular problems to several types of cancer. The widespread damage really highlights why spotting the signs and getting help is so important. The body can only take so much before its systems start to fail, triggering a cascade of serious health emergencies.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Physical and Mental Health Consequences of Alcohol Addiction
While liver disease gets the most attention, alcohol’s destructive path is truly systemic. The table below offers a brief look at the primary physical and mental health conditions directly caused by chronic alcohol misuse, providing a clearer picture of the risks involved.
| Condition Category | Specific Examples | Primary Impact |
|---|---|---|
| Liver Disease | Fatty Liver, Alcoholic Hepatitis, Cirrhosis | Impaired toxin filtration, inflammation, and irreversible scarring. |
| Heart Problems | High Blood Pressure, Cardiomyopathy, Arrhythmias | Weakened heart muscle and strained cardiovascular system. |
| Neurological Issues | Wernicke-Korsakoff Syndrome, Dementia | Severe memory loss, confusion, and impaired coordination. |
| Mental Health | Depression, Anxiety Disorders | Worsened mood instability and dependency cycles. |
As you can see, the consequences extend far beyond a single organ, affecting everything from heart function to cognitive abilities and emotional stability. Each of these conditions carries its own serious implications for a person’s health and quality of life.
How Alcohol Overwhelms and Destroys the Liver
Think of your liver as the body’s master filtration system, working tirelessly around the clock to clear out toxins and keep you healthy. When you introduce alcohol into your system, the liver gets to work breaking it down. But when faced with chronic, heavy drinking, this vital organ simply can’t keep up. It’s like asking a small household water filter to purify a rushing, muddy river—it becomes completely overwhelmed.
This constant strain sets off a dangerous chain reaction. The process of breaking down alcohol creates highly toxic byproducts, like acetaldehyde, which is even more damaging to your cells than the alcohol itself. These chemicals trigger inflammation and start killing off healthy liver tissue, paving the way for serious, long-term disease.
The Three Stages of Liver Destruction
Alcoholic Liver Disease (ALD) doesn’t just happen overnight. It’s a progressive condition that typically unfolds in three distinct stages, with each one representing a more severe level of damage. While the earliest stage can often be reversed by stopping drinking, the later stages can lead to permanent, life-threatening failure.
This journey from a stressed liver to a failing one is a clear and direct answer to the question: which condition is often a result of alcohol addiction?
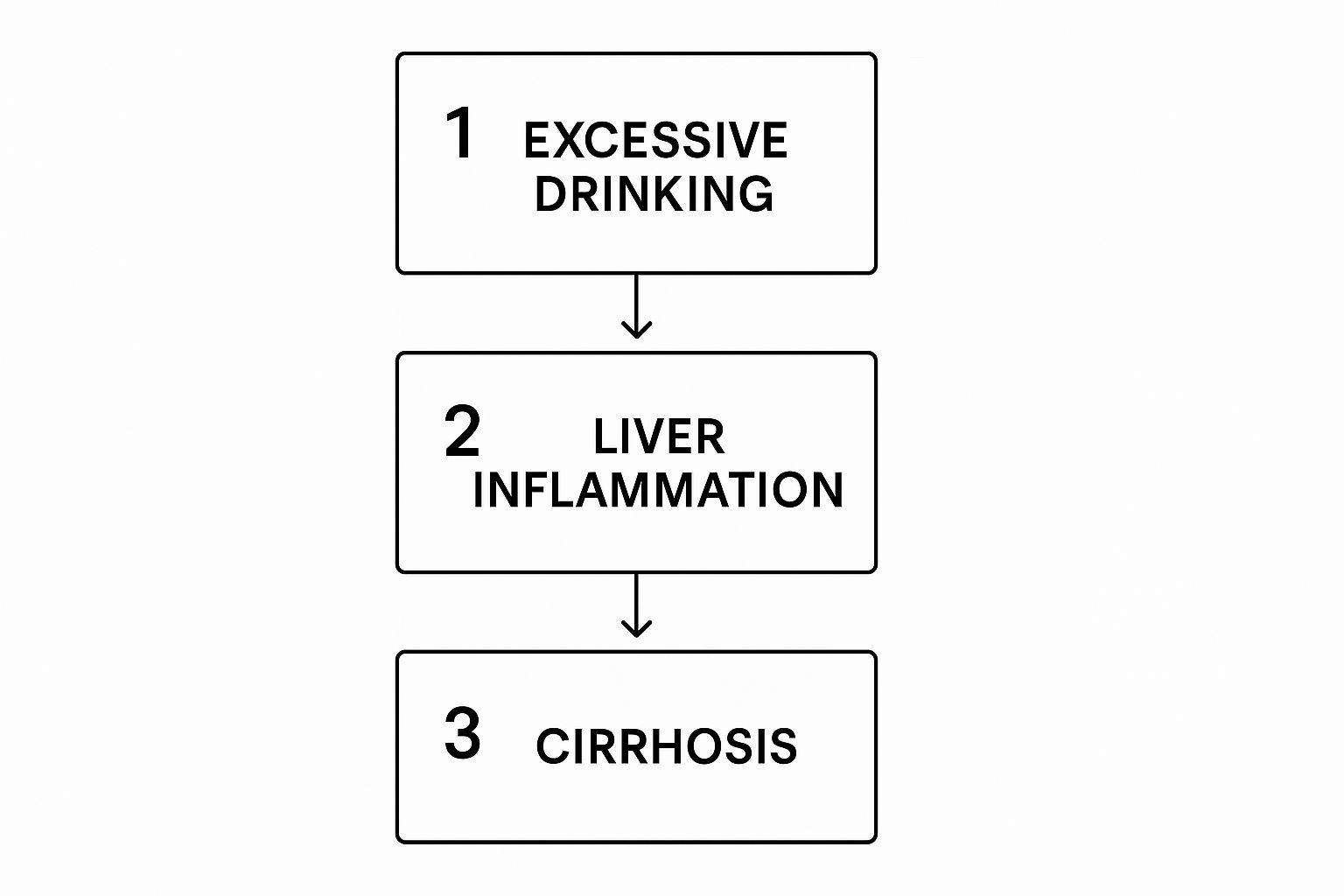
As you can see, continued alcohol use directly fuels inflammation, which eventually causes irreversible scarring known as cirrhosis.
The three main stages are:
- Fatty Liver (Steatosis): This is the first and most common sign of trouble. Fat begins to build up inside liver cells, causing the organ to swell. Most people don’t experience any symptoms at this point, but it’s a critical warning that the liver is under serious duress.
- Alcoholic Hepatitis: If heavy drinking continues, the persistent inflammation can escalate into alcoholic hepatitis. This is when symptoms usually start to appear, including fever, abdominal pain, and jaundice (a yellowing of the skin and eyes). This is a serious condition that can be fatal.
- Cirrhosis: This is the final, irreversible stage. After years of inflammation, healthy liver tissue is replaced by hard, non-functional scar tissue. The liver shrinks, hardens, and loses its ability to perform its essential functions, leading to severe complications like internal bleeding, fluid buildup, and ultimately, liver failure.
“Globally, alcohol is a leading cause of liver-related illness and death. Data shows alcohol use is causally linked to over 200 health conditions, with liver diseases being among the most prominent.”
From Silent Damage to Critical Failure
One of the scariest things about alcoholic liver disease is how quietly it can develop. A person can live with a fatty liver for years without any outward signs, allowing the damage to progress silently. By the time symptoms finally show up, the disease may have already reached an advanced stage.
As cirrhosis worsens, the failing liver can no longer filter toxins from the blood. These toxins can travel to the brain, causing confusion, personality changes, and even a coma. It’s crucial to understand these severe health risks, including acute emergencies. Our guide on the signs of alcohol poisoning offers vital information for these situations. The slow, tragic decline of the liver is one of the most direct and devastating consequences of untreated alcohol addiction.
Damage Beyond the Liver: The Toll on Your Heart and Brain

When we talk about alcohol’s physical toll, the liver often gets all the attention. But the damage doesn’t stop there. Alcohol is a systemic toxin, meaning it travels through the bloodstream and impacts every single organ, including the two most critical ones: your heart and brain.
When people ask which condition is often a result of alcohol addiction, it’s crucial to look past the liver. The heart, for instance, is a powerful muscle that simply can’t withstand the constant strain of heavy drinking. This can lead to a serious condition called alcoholic cardiomyopathy.
Essentially, the heart muscle gets stretched out, thin, and weak, losing its ability to pump blood effectively. Think of an overused rubber band that has lost its snap. This weakened heart then struggles to get oxygen-rich blood to the rest of your body, which can cause fatigue, shortness of breath, and eventually, life-threatening heart failure.
Alcohol’s Assault on the Cardiovascular System
Beyond just weakening the heart muscle, chronic drinking is a major cause of high blood pressure, or hypertension. Even a single night of binge drinking can send your blood pressure soaring temporarily.
Over years, this sustained high pressure puts a tremendous burden on your entire circulatory system. Your heart is forced to work overtime, and the constant stress can damage the walls of your arteries, making them prone to blockages. This dramatically increases your risk for several serious events:
- Arrhythmias: These are irregular heartbeats that might feel like a flutter or a racing pulse.
- Stroke: High blood pressure is a leading cause of strokes, which happen when blood flow to the brain is cut off.
- Heart Attack: This occurs when a blockage prevents blood from reaching the heart muscle itself.
The Brain’s Silent Suffering
The cognitive effects of alcohol go far beyond the temporary brain fog or memory gaps after a night out. Long-term, heavy alcohol use literally shrinks brain tissue and disrupts the delicate communication lines between brain cells.
One of the most tragic neurological outcomes is Wernicke-Korsakoff syndrome (WKS), sometimes grimly called “wet brain.” It’s actually two separate but related conditions rolled into one, caused by a severe deficiency of thiamine (vitamin B1), which alcohol abuse notoriously drains from the body.
“Wernicke-Korsakoff syndrome can inflict profound and often permanent damage. Sufferers experience severe memory loss, deep confusion, and a loss of muscle coordination. They may become unable to form new memories or recall significant parts of their past, which can completely alter their personality and rob them of their independence.”
WKS is a stark reminder of how addiction starves the brain of vital nutrients, leading to catastrophic and often irreversible consequences. This is why getting to the psychological root of the addiction is so important. Understanding the role of therapy in addiction recovery is a critical step, as it provides the support needed to heal both the mind and the body.
A Personal Story: John’s Wake-Up Call
John, a successful marketing executive, never thought he had a problem. A few whiskeys after work helped him unwind from the high-stress days. But over five years, “a few” turned into a bottle a night. He started forgetting meetings and snapping at his family. The wake-up call came not from a DUI, but from his doctor. Routine bloodwork showed elevated liver enzymes—the first sign of fatty liver disease. “My doctor told me that my ‘unwinding’ habit was actively poisoning me,” John recalls. “Seeing the tangible proof of the damage I was doing was terrifying. It was the push I needed to finally seek help.” John’s story shows how silently the physical toll can mount, even when someone appears to be functioning on the surface.
Recognizing the Signs of Alcohol Addiction

It’s a question many people silently ask themselves: when does social drinking tip over into something more dangerous? Figuring out if someone has an alcohol use disorder (AUD) isn’t about passing judgment. It’s about spotting patterns that show a clear loss of control. These signs often don’t appear overnight, building slowly until alcohol takes center stage.
Behavioral and Psychological Signs
Often, the most noticeable changes are in someone’s behavior and priorities. Common red flags include:
- Loss of Control: Drinking more or for longer than intended.
- Neglecting Responsibilities: Letting duties at work, school, or home slide due to drinking.
- Relationship Problems: Continuing to drink despite it causing issues with family or friends.
- Loss of Interest: Giving up on hobbies and activities that were once important.
- Cravings: Experiencing a strong, persistent urge to drink.
- Secrecy: Hiding the extent of one’s drinking or being defensive when it’s mentioned.
These changes are a clear signal that alcohol is no longer just a part of their life—it has become the main event. If you see these signs in someone and want to help, this guide on how to provide recovery support offers some really practical advice.
Physical Signs and Symptoms
The body has its own way of sending distress signals. A classic sign is tolerance, which means someone needs to drink more and more to get the same effect. Another major indicator is withdrawal. When they try to stop or reduce their drinking, their body protests with symptoms like tremors, sweating, nausea, anxiety, or insomnia. In severe cases, withdrawal can be life-threatening. Experiencing withdrawal is a powerful sign that the body is now physically dependent on alcohol.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Finding Your Path to Recovery and Hope
Taking that first, monumental step of admitting that alcohol has become a problem is incredibly brave. The next move—finding a path to recovery—is where the journey begins. Recovery isn’t one-size-fits-all; it involves finding a support system that addresses both the physical and mental health issues caused by alcohol.
Treatment Options for Alcohol Addiction
Modern treatment provides a toolbox of methods designed to fit individual needs. The goal is to build a solid foundation for lasting sobriety.
- Inpatient Rehab: This involves living at a treatment facility for 30-90 days, providing a structured, trigger-free environment. It’s best for severe addiction or co-occurring health issues.
- Outpatient Rehab: This allows individuals to live at home while attending regular therapy sessions, offering flexibility for those with strong support systems.
- Therapy: One-on-one counseling, particularly Cognitive Behavioral Therapy (CBT), helps identify triggers and build healthier coping strategies.
- Support Groups: Peer groups like Alcoholics Anonymous (AA) offer a powerful community of shared experience and mutual support.
- Medication: Certain FDA-approved medications can help reduce cravings and manage withdrawal symptoms, making it easier to focus on recovery.
Prevention Strategies
Preventing alcohol addiction often starts with education and awareness. Understanding the risks, promoting healthy coping mechanisms for stress, and fostering strong community and family support can reduce the likelihood of substance misuse. Encouraging open conversations about mental health and the dangers of self-medication is also a key preventative measure.
Resources for Help
If you or someone you know is struggling, you are not alone and effective help is available. For confidential support and to explore treatment options, you can visit https://addictionhelplineamerica.com/ or call Addiction Helpline America at 844-561-0606. Compassionate professionals are available 24/7 to guide you toward the right path for your situation.
Whether you need professional advice on supporting a loved one or want to explore treatment options for yourself, help is available. Contact Addiction Helpline America by calling our 24/7 confidential helpline at 844-561-0606 or find a wealth of resources at Addiction Helpline America’s website.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.






