Understanding What Barbiturates Are and Why They Matter
What are barbiturates? They are a class of powerful sedative-hypnotic drugs that depress the central nervous system (CNS). Here’s what you need to know:
Quick Answer: What Are Barbiturates?
- Drug Class: Central nervous system (CNS) depressants derived from barbituric acid
- Primary Effect: Slow down brain activity by enhancing GABA, causing sedation to coma
- Medical Uses: Historically for anxiety and insomnia; now mainly for seizures, anesthesia, and severe brain injury
- Legal Status: Controlled substances (Schedule II, III, or IV) due to high abuse potential
- Common Names: Phenobarbital, Seconal, Nembutal; street names include “barbs,” “downers,” “yellow jackets”
- Major Risks: Extremely addictive, narrow safety margin, high overdose risk, no antidote available
- Current Use: Largely replaced by safer drugs like benzodiazepines in the 1970s
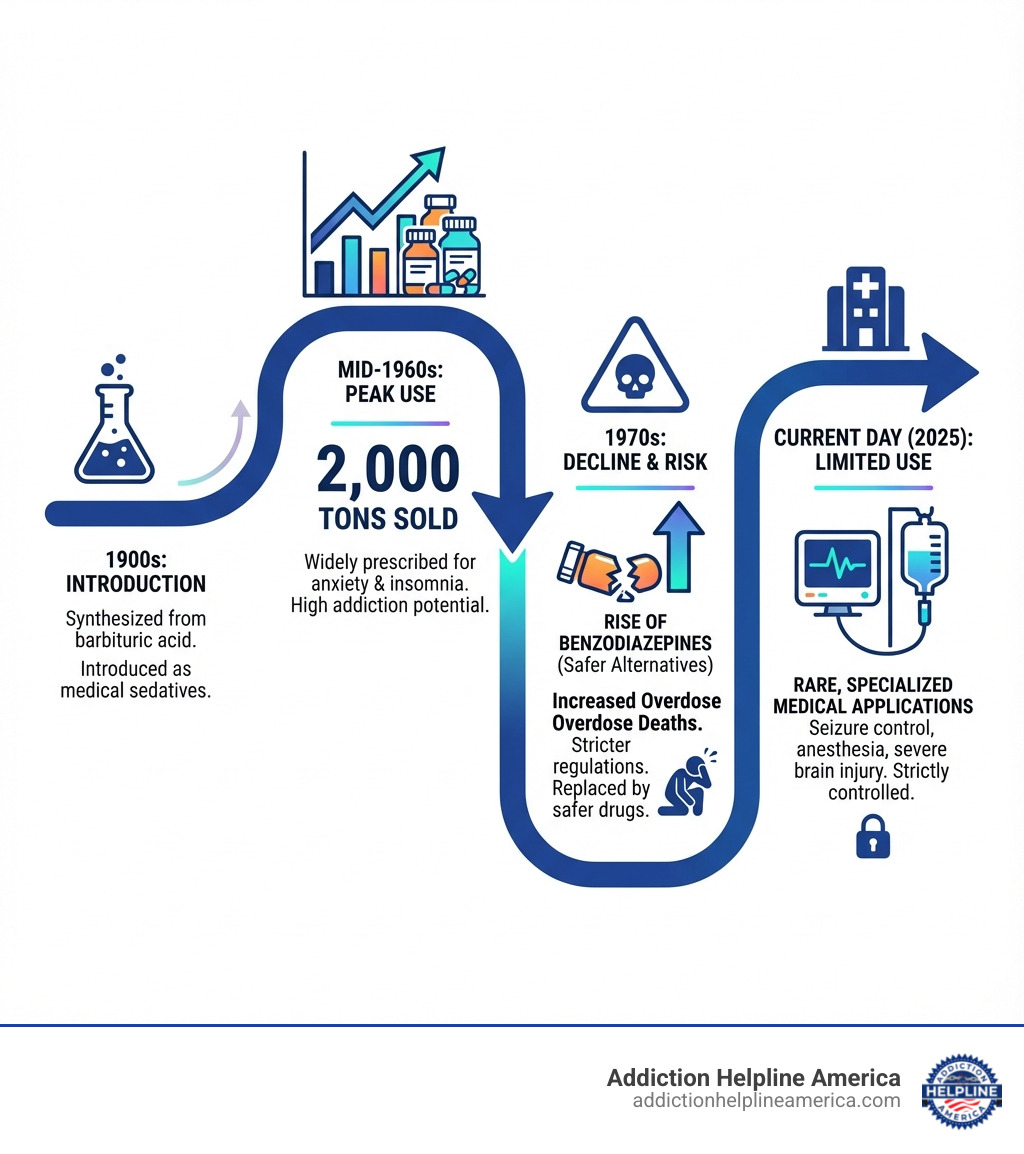
Once widely prescribed, barbiturate use peaked in the mid-1960s but plummeted in the 1970s due to their extreme addictiveness and a high number of overdose deaths. Their danger lies in a narrow therapeutic index: the difference between a therapeutic dose and a fatal one is frighteningly small. Combining them with alcohol or opioids dramatically increases overdose risk, and withdrawal can be life-threatening.
Today, safer medications like benzodiazepines have largely replaced them, but misuse still occurs with severe consequences. At Addiction Helpline America, we have extensive experience helping individuals and families steer the complexities of barbiturate addiction. Understanding what are barbiturates and their risks is the first step toward recovery. If you or someone you love is struggling, call us at 844-561-0606 for confidential support and guidance—we’re available 24/7 to help you find the right treatment path.
Must-know what are barbiturates terms:
What Are Barbiturates and How Do They Affect the Brain?
To understand what are barbiturates, we must look at how they affect the brain. These drugs are potent central nervous system (CNS) depressants derived from barbituric acid.
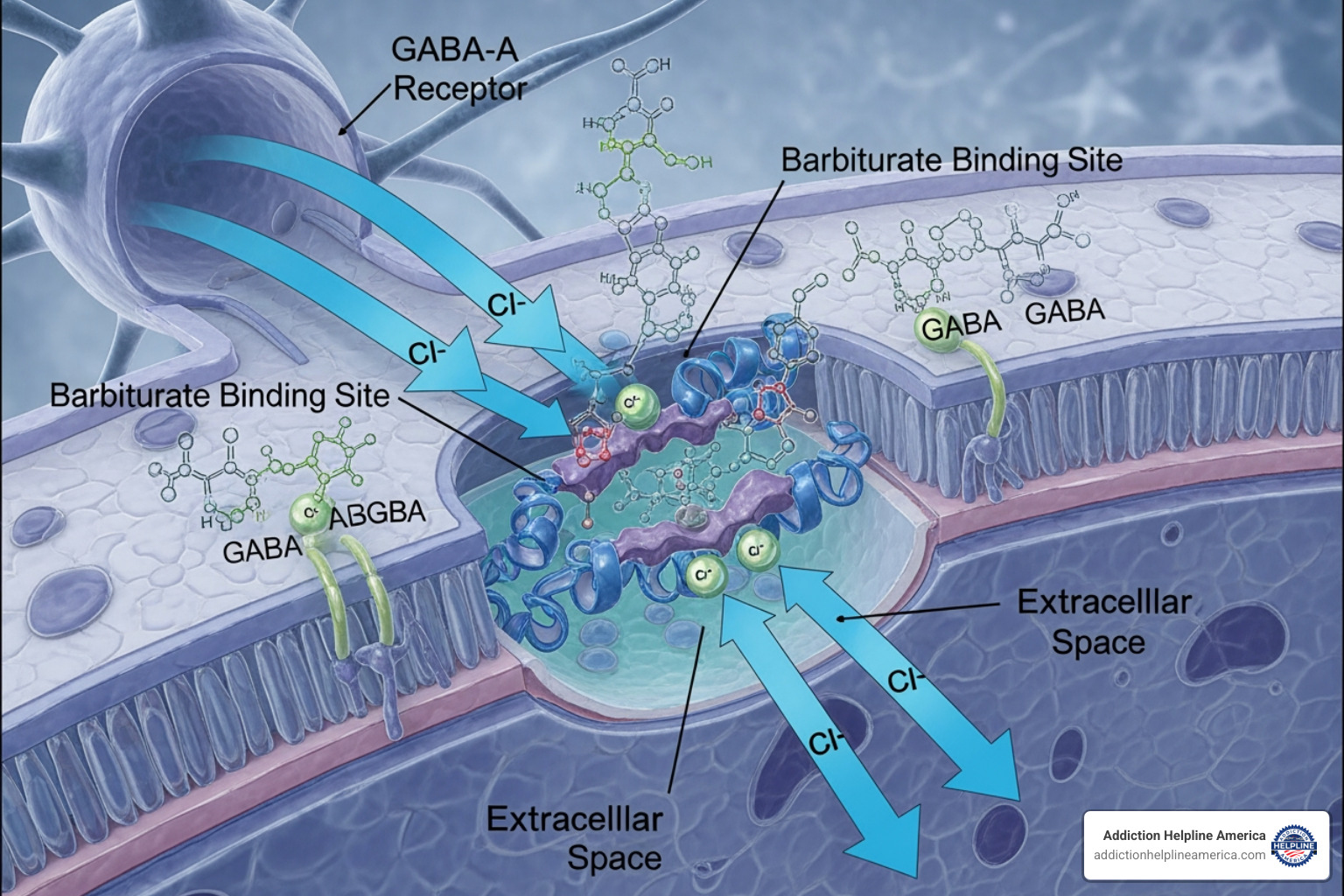
Their primary action is to improve the effects of gamma-aminobutyric acid (GABA), the brain’s main inhibitory neurotransmitter. GABA acts as the brain’s “brake pedal,” slowing nerve cell activity to produce calmness. Barbiturates amplify this effect by binding to GABA-A receptors and holding chloride ion channels open longer. This makes brain cells less likely to fire, effectively slowing down all brain activity. This powerful mechanism is what makes them both medically useful and incredibly dangerous. If you are concerned about how these drugs affect you or a loved one, call Addiction Helpline America at 844-561-0606 for immediate, confidential advice.
At lower doses, this leads to mild sedation. As the dose increases, the effects progress to sleep induction (hypnosis), anesthesia, and coma. They don’t just calm specific areas; they depress brain function broadly, affecting memory, judgment, coordination, and breathing.
What are the medical and historical uses of barbiturates?
For decades, barbiturates were hailed as miracle drugs for insomnia and anxiety. Historically, they were prescribed as:
- Sedatives: To calm anxiety.
- Hypnotics: To induce sleep.
- Anticonvulsants: To control seizures (phenobarbital was a staple).
- Anesthetics: For surgical procedures.
- “Truth Serums”: Sodium amytal was used in interrogations to lower inhibitions, though it often led to false memories and is no longer admissible.
The widespread use of barbiturates declined dramatically in the 1970s due to their high addiction potential, severe withdrawal, and narrow therapeutic index, which led to numerous overdose deaths. Safer alternatives like benzodiazepines emerged.
Today, their medical use is limited and specialized:
- Seizure Control: Phenobarbital is still used for refractory epilepsy and status epilepticus.
- Anesthesia: Ultra-short-acting barbiturates like methohexital are used for anesthesia induction.
- Severe Traumatic Brain Injury (TBI): Used to induce a coma to reduce intracranial pressure in critical care.
- Headache Disorders: Butalbital is a component in some migraine medications.
- Neonatal Withdrawal: Used to manage withdrawal symptoms in newborns.
For a deeper dive into their history, you can explore More on the history of barbiturates.
Types of Barbiturates and Their Classifications
Barbiturates are categorized by how long their effects last:
- Ultra-short-acting: Act almost instantly, lasting about 15 minutes. Used for anesthesia induction (e.g., Methohexital, Thiopental).
- Short-acting: Effects last three to four hours. Historically used for insomnia (e.g., Pentobarbital, Secobarbital).
- Intermediate-acting: Effects last four to six hours. Used for headaches or neurological tests (e.g., Amobarbital, Butalbital).
- Long-acting: Slowest onset, with effects lasting up to 12 hours. Used as anticonvulsants (e.g., Phenobarbital, Primidone).
Common brand names include Fiorinal®, Seconal®, and Nembutal®. Street names often reflect their effects or appearance: Barbs, Downers, Goof Balls, Red Devils, and Yellow Jackets.
Due to their high potential for abuse, barbiturates are strictly regulated under the Controlled Substances Act:
- Schedule II: High abuse potential, severe dependence risk (e.g., amobarbital, pentobarbital, secobarbital).
- Schedule III: Moderate to low dependence potential (most other barbiturates).
- Schedule IV: Low abuse potential and dependence risk (e.g., phenobarbital).
The Dangers and Side Effects of Barbiturate Use
The main reason barbiturates are rarely prescribed is their inherent danger. They have a narrow therapeutic index, meaning the line between a helpful dose and a fatal one is very thin. With no specific antidote for overdose, timely medical intervention is critical.
Even at prescribed levels, common side effects of what are barbiturates include:
- Drowsiness and sedation
- Dizziness and impaired coordination
- Slurred speech
- Confusion (especially in older adults)
- Headache and vertigo
- Nausea and vomiting
- Irritability and paranoia
- Low blood pressure
Barbiturates are also dangerous during pregnancy, as they can cross the placental barrier and cause withdrawal symptoms in newborns. If you are experiencing concerning side effects, please prioritize your safety. Call Addiction Helpline America at 844-561-0606 for guidance. Our team can connect you with medical resources in your area, from Florida to Texas.
Signs and Dangers of an Overdose
A barbiturate overdose is a life-threatening emergency. The drug’s profound CNS depression can shut down vital bodily functions. Initial signs of intoxication include slurred speech, an unsteady gait, poor judgment, and irritability.
An overdose is characterized by:
- Extreme drowsiness, unresponsiveness, or coma
- Shallow, slowed, or stopped breathing (the most common cause of death)
- Weak and rapid pulse, followed by low blood pressure and shock
- Decreased body temperature (hypothermia)
- Clammy skin
What to do in an overdose:
- Call 911 immediately. Provide all known information about the drug taken.
- Stay with the person. Try to keep them awake and position them on their side to prevent choking.
- Do not induce vomiting.
- Inform responders if other substances like opioids were taken.
Overdose management involves aggressive supportive care, primarily focused on supporting breathing with mechanical ventilation. For more on clinical management, see this Information on barbiturate toxicity.
The Risks of Mixing Barbiturates with Other Substances
Polydrug use, or mixing barbiturates with other substances, dramatically amplifies the risks and is a leading cause of death.
- Mixing with Alcohol: Both are CNS depressants. Together, their effects are synergistic, creating a much greater risk of severe respiratory depression, unconsciousness, and fatal overdose. We strongly advise against consuming any alcohol while taking barbiturates.
- Mixing with Opioids: This combination is extremely dangerous, as both substances are powerful respiratory depressants. The risk of breathing stopping completely and causing a fatal overdose is incredibly high.
- Mixing with Benzodiazepines: Combining these CNS depressants can lead to unpredictable and dangerously improved sedation, increasing overdose risk.
Mixing substances is a clear sign that professional help is needed. Our team at Addiction Helpline America is here to provide confidential support across states like Pennsylvania, Ohio, and Michigan. Call us at 844-561-0606 without delay.
Barbiturate Abuse, Dependence, and Long-Term Consequences
Understanding what are barbiturates requires acknowledging their high potential for abuse and the lasting damage they can cause. Abuse often starts with non-medical use to achieve euphoria or to counteract other drugs. In 2018, over 400,000 Americans reported using barbiturates, with tens of thousands misusing them, leading to significant health problems nationwide.
Understanding Tolerance and Dependence
The cycle of abuse is fueled by rapid tolerance and dependence.
- Tolerance: The body adapts quickly, sometimes within two weeks, requiring higher doses to get the same effect. This pushes users closer to a toxic dose.
- Dependence: With prolonged use, the body requires the drug to function normally. Intense psychological cravings also develop.
Barbiturate withdrawal is one of the most dangerous known. Abruptly stopping after regular use can trigger life-threatening symptoms, often within 8 to 15 hours:
- Restlessness, agitation, and severe anxiety
- Insomnia
- Tremors and sweating
- Hallucinations and delirium
- Severe, life-threatening seizures
Due to these risks, medical supervision is essential for barbiturate detoxification. Quitting “cold turkey” can be fatal. If you’re considering stopping, please seek professional help first. Call Addiction Helpline America at 844-561-0606 for safe detox options.
What are the long-term health effects of barbiturates?
Chronic barbiturate misuse exacts a heavy toll on physical and mental health:
- Cognitive Impairment: Persistent problems with memory, concentration, and judgment.
- Liver Damage: The liver is strained from metabolizing high doses of the drug.
- Muscle Weakness and Bone Pain: Chronic use can impact mobility and quality of life.
- Depression and Psychological Distress: Long-term use can worsen mood disorders, leading to chronic depression and paranoia.
- Increased Suicide Risk: The psychological toll significantly increases the risk of suicide. A sobering statistic reveals that 11% of males and 23% of females with sedative-hypnotic misuse die by suicide.
The damaging effects of long-term use underscore the need for early intervention. Addiction Helpline America is here to help at 844-561-0606.
Barbiturates vs. Benzodiazepines: A Comparison
To fully grasp what are barbiturates and why their use declined, it’s helpful to compare them to benzodiazepines, the drugs that largely replaced them. Both are CNS depressants that improve GABA, but they do so in different ways, leading to major differences in safety.
| Feature | Barbiturates | Benzodiazepines |
|---|---|---|
| Mechanism of Action | Increase the duration of chloride ion channel opening at GABA-A receptors. | Increase the frequency of chloride ion channel opening at GABA-A receptors. |
| Safety Margin | Narrow – Small difference between effective and toxic dose. | Wide – Much larger difference between effective and toxic dose. |
| Overdose Risk | High – Often fatal respiratory depression. | Lower – Rarely fatal when taken alone. |
| Antidote Availability | None – Management is purely supportive. | Available – Flumazenil can reverse overdose effects. |
| Addiction Potential | High – Rapid tolerance and life-threatening withdrawal. | Moderate to High – Withdrawal can be severe but is less life-threatening. |
| Current Medical Use | Limited to severe seizures, anesthesia, and critical care. | Widely used for anxiety, insomnia, seizures, and muscle spasms. |
Key Differences in Mechanism:
The critical difference is how they affect the brain’s GABA receptors. Barbiturates hold the brain’s chloride channels open longer, causing profound CNS depression that can easily become fatal. Benzodiazepines only increase the frequency of channel opening, a more subtle effect that makes them generally safer.
This distinction explains why benzodiazepines (“benzos”) and nonbenzodiazepines (“Z-drugs”) are now preferred for treating anxiety and insomnia. While they still carry risks, they do not have the same high lethality as barbiturates. If you have questions about these medications, call Addiction Helpline America at 844-561-0606.
Finding Help for Barbiturate Addiction
Recognizing the need for help with barbiturate addiction is a courageous first step. Signs of addiction may include:
- Inability to stop or control use
- Neglecting work, school, or family responsibilities
- Intense cravings for the drug
- Continuing use despite negative consequences
- Developing tolerance and experiencing withdrawal
If these signs are familiar, please know that confidential support is available. Addiction to barbiturates is a serious medical condition requiring professional intervention. Our team at Addiction Helpline America provides free, personalized guidance to help you find the right program from our network of treatment centers across the U.S., including in Arizona, Colorado, and Washington.
Effective treatment for barbiturate addiction involves several key stages:
- Medically Supervised Detoxification: This must occur in a specialized facility with 24-hour medical monitoring to safely manage the life-threatening withdrawal symptoms.
- Inpatient vs. Outpatient Rehab:
- Inpatient Treatment: Provides 24/7 care in a structured, immersive environment, which is often crucial for severe addictions.
- Outpatient Treatment: Allows individuals to live at home while attending regular therapy, suitable for those with strong support systems.
- Behavioral Therapies: Evidence-based therapies like Cognitive Behavioral Therapy (CBT) help address the root causes of addiction and build coping skills.
- Support Groups: Peer-led groups like Narcotics Anonymous offer a community of shared experience and ongoing encouragement for long-term sobriety.
Don’t wait to seek treatment. The sooner you reach out, the sooner you can begin your journey to recovery. Call Addiction Helpline America at 844-561-0606 to discuss your options today. Our compassionate team is ready to help you find a path to a healthier, substance-free life.
Frequently Asked Questions about What Are Barbiturates
Here, we address some of the most common concerns about what are barbiturates.
Why are barbiturates so dangerous?
Barbiturates are dangerous for several key reasons:
- Narrow Therapeutic Window: The effective dose is dangerously close to a toxic one.
- High Overdose Risk: A small extra amount can cause fatal respiratory depression, especially when mixed with alcohol or opioids.
- Severe Withdrawal: Abruptly stopping can cause life-threatening seizures.
- Lack of Antidote: There is no medication to reverse a barbiturate overdose.
Are barbiturates still prescribed today?
Yes, but their use is highly restricted. They are rarely prescribed for anxiety or insomnia. They are still used in controlled hospital settings for anesthesia, severe epilepsy, and managing traumatic brain injuries.
What are the withdrawal symptoms of barbiturates?
Barbiturate withdrawal is severe and requires medical supervision. Symptoms include:
- Tremors and muscle twitching
- Severe anxiety and agitation
- Insomnia
- Nausea and vomiting
- Hallucinations and delirium
- Potentially fatal seizures
Due to these risks, detox must be medically managed. Our team at Addiction Helpline America can help you find a facility that offers safe detox in states like New Jersey, Illinois, or Tennessee. Call us at 844-561-0606 for help.
Conclusion
This guide has detailed what are barbiturates: powerful CNS depressants with a dangerous history. Their narrow therapeutic index, high addiction potential, and severe withdrawal risks make them particularly hazardous. While largely replaced by safer drugs like benzodiazepines, barbiturates are still misused, leading to long-term cognitive damage, depression, and even suicide.
Understanding these risks is the first step toward safety. If you or someone you care about is struggling with barbiturate use, help is not just available—it’s essential. Addiction Helpline America is dedicated to connecting individuals nationwide with the specialized treatment they need. Our free, confidential guidance can help you steer the complexities of addiction and find the right recovery program.
Contact Addiction Helpline America today for free, confidential guidance to find the right treatment program. We are here to support you on your journey to lasting recovery.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.