Why Veterans Inpatient Rehab is Critical for Service Members in Crisis
Veterans inpatient rehab provides 24/7 medical care and intensive treatment for service members battling substance use disorders (SUDs) and co-occurring mental health conditions like PTSD. These programs offer a structured environment away from daily stressors, featuring specialized treatment for combat trauma, peer support from fellow Veterans, and integrated mental health care.
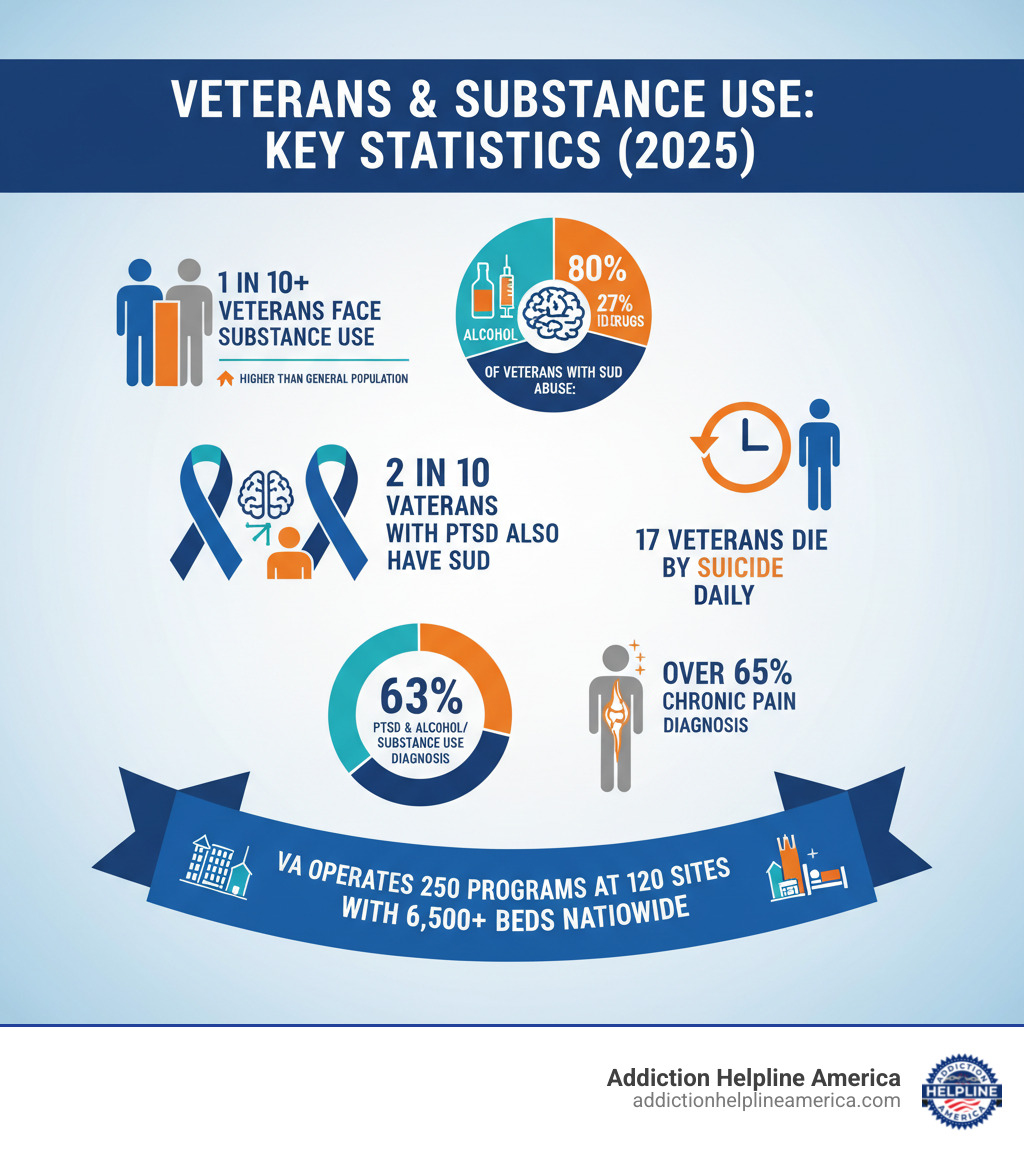
The need is significant: more than 1 in 10 Veterans face substance abuse, and 2 out of 10 Veterans with PTSD also have a SUD. The unique challenges of military service—combat exposure, physical injuries, and the difficulty of transitioning to civilian life—create a high risk for substance use. Standard rehab programs often fail to address the specific trauma and cultural factors affecting the military community, which is why veteran-specific inpatient rehab is so crucial.
Recovery is possible with the right treatment. Inpatient rehab offers the most intensive level of care, providing medical supervision, trauma-informed therapy, and a safe space to heal. This guide will cover why service members face unique addiction challenges, what to expect from treatment, and how to access care through VA benefits.
At Addiction Helpline America, we connect Veterans and their families with specialized Veterans inpatient rehab programs. Our team provides 24/7 support and guidance through the VA system to help service members access the care they’ve earned.
Why Veterans Face Unique Addiction Challenges
Military service can expose individuals to challenges that significantly increase the risk of substance use and mental health conditions. Currently, 3.7 million Veterans live with a mental illness or substance use disorder. Understanding these unique challenges is the first step toward finding the right help, like Veterans inpatient rehab.

- Combat exposure creates psychological wounds, and research confirms a strong link between combat and an increased risk of alcohol misuse.
- Post-Traumatic Stress Disorder (PTSD) affects 11% to 30% of combat Veterans. To cope with symptoms like flashbacks and severe anxiety, 2 out of 10 Veterans with PTSD also develop a substance use disorder. Learn more from the VA’s PTSD resources.
- Traumatic Brain Injury (TBI) affects over 185,000 Veterans using VA healthcare. TBIs can cause behavioral changes and cognitive issues, and service members with TBIs also show higher rates of PTSD. The VA researches and treats Polytrauma and TBI.
- Chronic pain is a reality for over 65% of Veterans, often leading to treatment with highly addictive prescription opioids. This can inadvertently lead to an increased risk of dependence.
- Military Sexual Trauma (MST) affects about 1 in 5 female Veterans and can lead to substance misuse, depression, and isolation. The VA provides specialized support for Women Veterans.
- Re-adjusting to civilian life can be overwhelming. The loss of military structure and camaraderie, combined with invisible wounds, often leads to isolation and substance use as a coping mechanism.
The Link Between Service, Trauma, and Substance Use
For Veterans, trauma and substance use are often intertwined. Co-occurring disorders are common, with 63% of recent combat Veterans diagnosed with both PTSD and a substance use disorder. Many turn to self-medication with alcohol or drugs to numb emotional pain, which ultimately worsens both conditions. Among Veterans with a SUD, 80% abuse alcohol. The opioid prescription risk is also high, as treatment for chronic pain can lead to addiction. Tragically, these issues contribute to a high suicide risk, with about 17 Veterans a day dying by suicide in 2020. If you or a Veteran you know is in crisis, visit VeteransCrisisLine.net or call 988 (Press 1).
Recognizing the Signs That a Veteran Needs Help
Military culture can make asking for help difficult. Family and friends should watch for warning signs:
- Behavioral changes: Mood swings, irritability, or withdrawal from activities.
- Relationship issues: Frequent conflicts or isolation from loved ones.
- Neglecting responsibilities: Problems at work or home, job loss, or financial trouble.
- Increased substance use: Using more to get the same effect or experiencing withdrawal symptoms.
- Physical signs: Deterioration in hygiene or changes in sleep patterns.
- Continuing use despite harm: Persisting with substance use even when it’s causing problems.
If you see these signs, approach the Veteran with compassion. At Addiction Helpline America, we help families steer these conversations and connect Veterans with the right care. Seeking help is one of the bravest things a Veteran can do.
What is Veterans Inpatient Rehab and How Does it Help?
For Veterans struggling with addiction and service-related trauma, Veterans inpatient rehab offers the most intensive level of care. It provides a highly structured, supportive sanctuary where you can step away from daily triggers and focus entirely on healing. Within the VA system, this is often called residential rehabilitation, where you live at the facility and receive 24/7 support.

The VA operates about 250 programs at 120 residential rehab sites nationwide, serving over 6,500 Veterans at a time. These programs use a “whole health approach,” addressing medical needs, employment, housing, and social connections alongside addiction. Key components include:
- 24/7 medical supervision: Staff monitor vital signs and manage withdrawal symptoms, which is critical for safely detoxing from substances like alcohol or benzodiazepines.
- Structured environment: A predictable schedule of therapy, groups, and activities creates stability, which is familiar and beneficial for many Veterans.
- Safe detoxification: A controlled environment minimizes the risks and discomfort of withdrawal.
- Peer support: You are surrounded by fellow service members who understand military culture and experiences, creating powerful bonds of trust.
- Removal from triggers: A temporary sanctuary away from people, places, and situations that fuel substance use provides the space needed to heal.
- Focusing entirely on recovery: With basic needs met, you can immerse yourself in the therapeutic process.
Benefits of Veterans Inpatient Rehab
Choosing a veteran-specific inpatient program offers distinct advantages:
- Intensive therapy: Daily individual and group sessions allow you to dive deep into the roots of addiction and trauma.
- Integrated mental health care: Co-occurring disorders like PTSD, depression, and anxiety are treated simultaneously with addiction.
- Camaraderie with fellow Veterans: A shared understanding of service creates a unique and powerful support network.
- Comprehensive treatment planning: Plans are individualized and address all aspects of your well-being, from physical health to vocational goals.
- Higher success rates: The immersive, structured environment is highly effective for Veterans with severe SUDs or a history of relapse.
Inpatient vs. Residential vs. Outpatient: Choosing the Right Level of Care
Understanding the differences between care levels helps you make the best choice. “Inpatient” and “residential” are often used interchangeably, but there are some distinctions.
- Inpatient Rehab: The highest intensity, hospital-based care for short-term medical detox and stabilization.
- Residential Rehab: Long-term care (weeks to months) in a non-hospital setting, focusing on therapy and skill-building.
- Outpatient Rehab: Allows you to live at home while attending scheduled therapy sessions, ideal for less severe SUDs or as a step-down from a higher level of care.
| Feature | Inpatient Rehab | Residential Rehab | Outpatient Rehab |
|---|---|---|---|
| Intensity | Highest: 24/7 medical and clinical care | High: 24/7 structured living with clinical care | Low to Moderate: Scheduled therapy sessions |
| Living Situation | Hospital or clinical setting, 24/7 supervision | Non-hospital setting, 24/7 sober living environment | Lives at home, commutes for treatment |
| Duration | Short-term: Days to a little over a week | Medium to long-term: Several weeks to many months | Flexible: Weekly sessions for months or years |
| Ideal Candidate | Severe SUD, medical detox needed, acute mental health crisis, high relapse risk | Chronic SUD, co-occurring disorders, need for structured environment, transition from inpatient | Mild to moderate SUD, strong support system, able to manage daily life, step-down from higher levels of care |
Choosing the right level depends on your individual needs. What matters is finding the support that gives you the best chance at lasting recovery.
Core Therapies and Treatments in Veteran-Specific Programs
Effective Veterans inpatient rehab programs go beyond just stopping substance use; they heal the underlying wounds. For Veterans, this means addressing trauma, PTSD, and chronic pain through a combination of proven medical and therapeutic treatments.
Dual-diagnosis treatment is central to quality care, as addiction and mental health conditions like PTSD are often intertwined. The best programs treat both simultaneously. Treatment is built on a foundation of evidence-based therapies:
- Cognitive Behavioral Therapy (CBT): Helps change negative thought patterns that lead to substance use.
- Dialectical Behavior Therapy (DBT): Teaches skills to manage intense emotions and improve relationships.
- Eye Movement Desensitization and Reprocessing (EMDR): A highly effective therapy that helps the brain process traumatic memories, reducing their emotional impact. Learn more about PTSD treatment at the VA’s PTSD page.
- Prolonged Exposure (PE): Gradually helps you confront traumatic memories and situations until they lose their power.
- Motivational Interviewing (MI): A collaborative approach that helps you find your own motivation to change.
- Medication-Assisted Treatment (MAT): Combines FDA-approved medications (like buprenorphine or naltrexone) with counseling to reduce cravings and support recovery from opioid or alcohol addiction.
- Holistic and Life Skills Approaches: Therapies like mindfulness, yoga, art therapy, and vocational training address the whole person—mind, body, and spirit—and prepare you for life after rehab.
Treating Co-Occurring Disorders: The Key to Lasting Sobriety
For Veterans, addiction is rarely just about the substance. Treating co-occurring mental health disorders is essential for lasting recovery. An integrated approach is needed to address the complex links between PTSD and SUD, provide specialized TBI support for cognitive challenges, and offer depression and anxiety treatment to stabilize mood without self-medication. The VA provides comprehensive information on its mental health conditions resources, and Veterans can log into My Health to access screenings and support.
Finding a Specialized Veterans Inpatient Rehab Program
Not all rehabs are equipped to serve Veterans. Look for programs with:
- Veteran-specific tracks: Grouping Veterans together creates powerful camaraderie and a judgment-free zone.
- Staff trained in military culture: Therapists who understand the military mindset can connect on a deeper level.
- Trauma-informed care: The entire environment is designed to feel safe and avoid re-traumatization.
- Gender-specific programs: These can provide a safer space for Veterans, especially those who have experienced Military Sexual Trauma.
Many VA residential programs and qualified community providers offer these specialized services. Your care team can help you determine whether a VA facility or an authorized community option is the best fit based on your needs and eligibility.
At Addiction Helpline America, we help you find a *Veterans inpatient rehab program that truly understands your experience. Our team is available 24/7 to guide you toward the specialized care you’ve earned.*
Navigating Benefits and Finding the Right Center
Once you’ve decided to seek help, the next step is figuring out how to pay for Veterans inpatient rehab. As a Veteran, you have earned comprehensive healthcare benefits, and multiple pathways exist to access the treatment you need.

Your primary resource is the Department of Veterans Affairs (VA) healthcare system, which offers a full range of substance abuse treatment services. You can explore your Health Benefits at VA.gov. If a VA facility isn’t available or close by, the VA Community Care Network (CCN) allows you to receive authorized care at an approved non-VA facility in your community. Many Veterans also have private health insurance or TRICARE, which can cover treatment at non-VA facilities.
Regarding cost and copays, VA healthcare is often low-cost or free, depending on your service history, income, and other factors. The VA uses a Means Test to determine if you will have any Copays.
How Can Benefits Cover Inpatient Rehab?
Accessing your benefits for inpatient rehab involves a few key steps:
- Enroll in VA Health Care: If you haven’t already, you must apply for VA health care benefits. Most Veterans who served in active service and were discharged under conditions other than dishonorable are eligible. Check your Veteran Eligibility to be sure.
- Get a Referral: Schedule an appointment with a VA primary care provider or contact a mental health provider at your local VA medical center. Be honest about your concerns—they can assess your needs and refer you to the appropriate level of care. Some residential programs also accept direct applications.
- Coordinate Community Care: If you plan to use a non-VA facility through the CCN, a referral from the VA is essential to ensure coverage. Our team at Addiction Helpline America can help you steer this authorization process.
How to Find Approved or Specialized Rehab Centers
Finding the right program is a critical decision. The VA’s website is an excellent starting point.
- Use the Hospitals & Clinics locator to find your nearest VA facility.
- Search the dedicated Substance Use Disorder (SUD) Program – Locations directory for specialized programs in your state.
- Find community-based counseling and support at Vet Centers.
Your VA provider is your best advocate and can recommend appropriate VA or community care programs. The VA operates facilities nationwide, and you can find a program in your state. Examples include:
- Arizona:Northern Arizona VA Health Care System
- California:VA Central California Health Care System
- Florida:VA Lecanto Clinic
- Georgia:Atlanta VA Health Care System
- Kentucky:Lexington VA Medical Center
- Maryland:VA Maryland Health Care System
- New Jersey:VA New Jersey Health Care System
- Ohio:VA Central Ohio Healthcare System
Navigating this system can be complicated. At Addiction Helpline America, we use our expertise to help you find a program that fits your needs, whether it’s a VA facility or a specialized community provider. Our services are free and confidential.
Life After Rehab: Support for Lasting Recovery
Completing Veterans inpatient rehab is a major accomplishment, but it’s the beginning of a lifelong recovery journey. The transition back to civilian life can be challenging, which is why a strong aftercare plan is essential. Before you leave treatment, your team will work with you to create a personalized roadmap for sustained recovery.
This plan may include stepping down to an intensive outpatient program (IOP), continuing with individual and group therapy, and participating in mutual-help groups like Alcoholics Anonymous (AA) or SMART Recovery. Your VA case manager will help ensure you have a safe discharge plan and access to these services.
Relapse prevention strategies are a core part of aftercare. You will continue to practice identifying your triggers and using the healthy coping mechanisms you learned in rehab. If a relapse occurs, it’s not a failure but a sign to reach out for help and get back on track quickly.
Building a sober network is crucial. Staying connected to the Veteran community you built in rehab through alumni groups or peer support provides ongoing accountability. Many Veterans also find purpose and stability through vocational and housing support. The VA’s Compensated Work Therapy-Transitional Residence (CWT-TR) program helps Veterans overcome employment barriers, while resources for Homeless Veterans can provide housing stability.
How Can Family Members Support a Veteran in Recovery?
Family support is a powerful factor in a Veteran’s recovery. Here’s how you can help:
- Participate in Family Therapy: Addiction affects the entire family. Therapy provides a safe space to heal, improve communication, and rebuild trust.
- Educate Yourself: Learning about addiction as a medical condition helps you respond with compassion instead of frustration. Understanding the unique challenges Veterans face is key.
- Create a Supportive Home Environment: Make your home a safe space for recovery by removing alcohol or other triggering substances. Work to create a peaceful atmosphere that minimizes stress.
- Set Healthy Boundaries: There is a fine line between supporting and enabling. Healthy boundaries mean loving the person while holding them accountable. For example, refuse to provide money for substances but offer to drive them to a support meeting. This protects their recovery and your own well-being.
Taking care of yourself is also vital. The VA’s Caregiver Support program offers assistance, education, and resources for those caring for Veterans. You can call the Caregiver Support Line at 855-260-3274 or explore resources for Families of Veterans. Support groups like Al-Anon or Nar-Anon can also provide community and understanding.
At Addiction Helpline America, we support the entire family. We can help you understand what to expect and find resources for your loved one and for yourself.
Conclusion: Take the First Step Towards a Healthier Future
The path to recovery is a brave one, and no Veteran should have to walk it alone. Veterans inpatient rehab offers the specialized, intensive care needed to address the unique challenges of military service, from combat trauma and PTSD to chronic pain.
We’ve seen how these programs provide a medically supervised, peer-supported environment where deep healing can happen. With integrated treatment for co-occurring disorders and therapies designed for military culture, recovery is not just possible—it’s a reality for countless Veterans.
At Addiction Helpline America, we are honored to serve those who have served us. Our mission is to provide free, confidential guidance to connect Veterans with the best treatment programs available. We understand the VA system and can help you find a program that meets your unique needs.
Your path to a healthier future starts with a single step. Reach out today.
Explore different types of treatment programs
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
24/7 Free & Confidential Helpline for Veterans Inpatient Rehab
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.












