Why Veterans Deserve Specialized Alcohol Treatment Support
Veterans alcohol treatment refers to specialized programs addressing the unique challenges military members face with alcohol use disorders (AUD). This includes trauma-informed care, treatment for co-occurring conditions like PTSD, and support systems that understand military culture.
Key Veterans Alcohol Treatment Options:
- VA Medical Centers: Offer detox, rehab, and medications at low or no cost.
- Community Care Network: Provides access to private treatment through VA authorization.
- Evidence-Based Therapies: Includes CBT, Motivational Interviewing, and EMDR.
- Medications for AUD: Naltrexone, acamprosate, and disulfiram help reduce cravings.
- Residential & Peer Support: Structured 24/7 care and veteran-specific support groups.
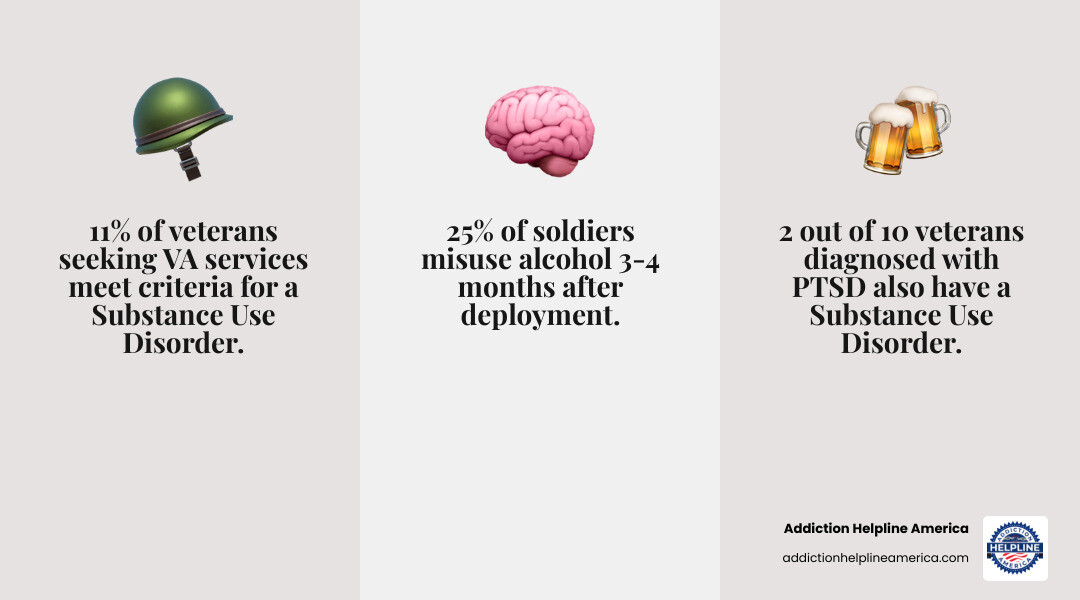
The reality is stark: 11% of veterans seeking VA services meet the criteria for a substance use disorder. Even more concerning, 2 in 10 veterans with PTSD also have a substance use disorder, and combat exposure is a major risk factor, with 25% of soldiers misusing alcohol post-deployment.
Veterans face unique barriers like combat trauma, chronic pain (affecting over 65%), and the stress of reintegration, which can create a perfect storm for alcohol misuse. Traditional treatment often fails to address these specific military-related triggers.
The good news is that veterans are more likely to seek alcohol treatment than non-veterans when the right resources are available. This guide outlines five practical pathways to finding effective veterans alcohol treatment, from professional assessments to peer support.
At Addiction Helpline America, we help veterans and their families steer the complexities of finding care. Our team is here 24/7 to connect you with resources, verify insurance, and provide compassionate guidance.
Veterans alcohol treatment helpful reading:
1. Start with a Professional Assessment Custom for Veterans
A professional assessment is like creating a map for recovery. For veterans, this map must be especially detailed, as alcohol misuse rarely occurs in isolation.
For those seeking veterans alcohol treatment, a standard assessment often misses critical issues. Two out of 10 veterans with PTSD also have a substance use disorder. Many also cope with Traumatic Brain Injury (TBI), chronic pain (affecting over 65% of veterans), or Military Sexual Trauma (MST). These challenges can fuel a cycle of self-medication that feels impossible to break.
A comprehensive, veteran-focused assessment digs deeper than “Do you drink too much?” It screens for mental health conditions like PTSD and depression, considers your military service history, and evaluates the unique stressors of transitioning to civilian life. Understanding that combat exposure is a major risk factor for alcohol problems changes the entire approach to treatment.
The assessment also identifies practical challenges, such as financial difficulty or low social support, so your treatment plan can address them from day one.
At Addiction Helpline America, we connect veterans to centers that conduct these in-depth evaluations, ensuring a truly personalized care plan. We’re here to help you find the right place to start.
Evidence-Based Therapies and Medications for Veterans
Once assessed, your treatment plan should include proven methods. There is solid science behind what helps veterans recover from alcohol use disorders.
- Cognitive Behavioral Therapy (CBT) helps change thought patterns that fuel drinking.
- Motivational Interviewing helps you find your own internal reasons for change.
- Eye Movement Desensitization and Reprocessing (EMDR) is transformative for processing traumatic memories that may drive alcohol use.
- Contingency Management offers tangible rewards for staying sober.
- 12-Step Facilitation connects you with peer support groups like Alcoholics Anonymous.
Medication can also be a game-changer. The VA and specialized centers offer FDA-approved medications for Alcohol Use Disorder (AUD):
- Naltrexone reduces cravings and the rewarding effects of alcohol.
- Acamprosate helps with long-term withdrawal symptoms like anxiety.
- Disulfiram creates an unpleasant physical reaction to alcohol, acting as a deterrent.
Combined with therapy, these medications significantly improve the chances of lasting recovery. The most effective veterans alcohol treatment integrates these tools into a plan customized to your specific needs. Addiction Helpline America can connect you to programs offering these evidence-based options.
2. Find Accredited Alcohol Treatment Programs with Veteran-Focused Services
After an assessment, the next step is finding a program that understands the military experience. Not all rehab facilities are equipped to provide the specialized care veterans need.
When searching for veterans alcohol treatment, look for programs with proper accreditation from organizations like The Joint Commission or CARF, and verify they are state-licensed. These credentials ensure the facility meets high standards for safety and quality.
Beyond credentials, seek programs with staff trained in military culture. Many top facilities employ veterans, creating an immediate sense of trust and shared understanding. These programs excel at treating co-occurring conditions, recognizing that 2 in 10 veterans with PTSD also struggle with substance use. They don’t treat alcohol use in isolation; they address it alongside PTSD, TBI, and chronic pain as interconnected parts of your story.
Many centers offer dedicated veteran tracks, reducing the isolation that can hinder recovery. Being surrounded by peers who understand your service creates a powerful healing environment.
Addiction Helpline America has vetted facilities nationwide that specialize in veteran care. We can connect you to a program that fits your needs and honors your service.
Understanding Levels of Care
Veterans alcohol treatment is not one-size-fits-all. It involves different levels of care for specific stages of recovery.
- Detoxification: A medically supervised process (3-7 days) to safely manage withdrawal symptoms for those with physical dependence.
- Inpatient/Residential Rehab: The most intensive level, providing 24/7 structured care and support, typically for 30-90 days. Ideal for those with severe AUD or co-occurring conditions.
- Partial Hospitalization Program (PHP): Intensive daytime treatment (5-6 hours/day) while you return home at night. It’s a step down from inpatient care.
- Intensive Outpatient Program (IOP): Offers 9-12 hours of treatment per week, allowing you to maintain work or family duties.
- Standard Outpatient Care: Consists of 1-2 therapy sessions per week, suitable for those with strong support systems or as a step-down from IOP.
- Aftercare Planning: A crucial roadmap for maintaining sobriety after formal treatment, including ongoing therapy and support groups.
Choosing the right level of care depends on your assessment. At Addiction Helpline America, we help you understand these options and connect you with the right level of support at the right time.
3. Explore Financial Assistance and Insurance Options for Veterans
One of the biggest worries about treatment is the cost. However, veterans have more options for covering veterans alcohol treatment than most people realize, and financial barriers should not prevent you from getting help.
- VA Health Care: If you’re enrolled, you can often receive substance use disorder treatment—from detox to outpatient therapy—at little to no cost.
- VA Community Care Program: The VA MISSION Act allows eligible veterans to receive care from approved private treatment centers, with the VA covering the cost. This is an option if you live far from a VA facility or face long wait times.
- TRICARE: Active-duty members, retirees, and their families have comprehensive coverage for all levels of substance abuse treatment.
- Medicare & Medicaid: Many veterans qualify for these programs, which can provide substantial coverage for treatment, especially outside the VA system. Nearly 10% of veterans are covered by Medicaid.
- Private Health Insurance: Employer-provided or marketplace plans can be used at non-VA facilities and can work alongside your VA benefits.
Navigating these options can be confusing. At Addiction Helpline America, our admissions navigators offer free, confidential insurance verification. We can help you understand your benefits, maximize them, and find a program that fits your financial situation.
Navigating Coverage for Veterans Alcohol Treatment
Most insurance plans, including VA benefits, TRICARE, and private policies, cover the full spectrum of care, from medical detox to outpatient services. The duration and intensity of covered treatment are based on medical necessity as determined by your assessment.
If you have both VA benefits and other insurance, you can use them strategically. VA benefits cover care at VA facilities, while other insurance can be used for treatment outside the VA network. This can help reduce or eliminate out-of-pocket costs.
To use the VA Community Care Network, you must get VA authorization before seeking treatment at a non-VA facility. Your VA care team can help, or we can assist in navigating this process. Be aware of potential copayments or deductibles with any plan.
If you are uninsured, your first step should be to check your eligibility for VA health care. You can also explore Medicaid in your state or seek out non-profits and state-funded programs that offer free or low-cost treatment. Many private centers also offer sliding scale fees. Our team can help you explore all these options.
4. Seek Programs Addressing Co-Occurring Disorders and Trauma
For many veterans, alcohol use is deeply intertwined with the invisible wounds of service—PTSD, chronic pain, and trauma. This is why effective veterans alcohol treatment must address the whole person, not just the addiction.
The statistics are clear: two in ten veterans with PTSD also have a substance use disorder. Among recent veterans, up to half experience both a mental health and substance use disorder simultaneously. With over 65% of veterans living with chronic pain and many impacted by Military Sexual Trauma (MST), treating alcohol use in isolation is ineffective.
Veterans often use alcohol to self-medicate these conditions—to numb pain, quiet nightmares, or escape memories. This creates a trap where drinking offers temporary relief but ultimately worsens the underlying issues.
Integrated care is the solution. In an effective program, mental health therapists, addiction counselors, and medical staff collaborate on your treatment. PTSD isn’t something to be handled “later”; it’s addressed simultaneously with the alcohol use because they are fundamentally connected.
These programs are built on a foundation of trauma-informed care, creating a safe environment that recognizes the impact of military service. Dual diagnosis programs integrate therapies for both addiction and mental health into one cohesive plan, helping veterans process trauma and develop healthy coping skills.
At Addiction Helpline America, we prioritize connecting veterans to facilities that specialize in dual diagnosis and trauma-informed care, because treating the whole person is the standard for lasting recovery.
Therapies for Trauma and Recovery
When trauma is unaddressed, it fuels addiction. Trauma-focused therapies are essential in veterans alcohol treatment to break the self-medication cycle.
- Eye Movement Desensitization and Reprocessing (EMDR) helps process traumatic memories, reducing their emotional charge so they are no longer overwhelming.
- Cognitive Processing Therapy (CPT) helps veterans challenge and change unhelpful beliefs about trauma, the world, and themselves.
- Dialectical Behavior Therapy (DBT) provides powerful skills for managing the intense emotions that trauma can trigger, offering alternatives to drinking.
- Group Therapy with other veterans is especially powerful, creating a sense of belonging and mutual understanding that reduces isolation and fosters hope.
These therapies provide healthy ways to cope with difficult emotions and memories. Effective programs also address physical health, social connection, and life purpose, building a strong foundation for a life worth living. We can connect you with programs offering these advanced, trauma-informed therapies.
5. Connect with Peer, Family, and Community Support Resources
Recovery doesn’t happen in a vacuum. It thrives in connection with others who understand your journey. Research shows that strong social support is a key factor in successful recovery for veterans.
Peer support groups offer a unique space where you don’t have to explain the challenges of military service and reintegration. Other veterans just get it.
- Alcoholics Anonymous (AA) and Narcotics Anonymous (NA) provide a 12-step framework in nearly every community. Many areas have meetings exclusively for veterans.
- SMART Recovery offers an alternative, science-based approach focused on self-empowerment.
- Vet Centers are community-based counseling centers, often staffed by veterans, that offer free and confidential readjustment counseling.
The VA’s “Make the Connection” program also provides tools and stories from peers with similar experiences. At Addiction Helpline America, we help you find these ongoing support networks that are crucial for turning initial recovery into lasting sobriety.
Resources for Spouses, Family, and Friends
Addiction impacts the entire family. If you’re a friend or family member of a veteran who is struggling, there is support for you, too. Your role in their recovery can be incredibly powerful.
You can’t force recovery, but you can create an environment that encourages it. The VA suggests discussing your concerns privately and calmly, focusing on specific behaviors. Offering to help research treatment can make a significant difference.
It’s also vital to get support for yourself. Key resources include:
- Al-Anon and Alateen for families affected by someone’s drinking.
- Community Reinforcement and Family Training (CRAFT), a VA-endorsed online course that teaches strategies to encourage treatment while supporting your own well-being.
- The VA’s Caregiver Support Line at 855-260-3274.
- Military OneSource for 24/7 confidential help at 1-800-342-9647.
- The National Resource Directory (NRD) connects veterans and families with a wide range of support programs.
Addiction Helpline America recognizes that family support is vital. We can connect your entire family with the resources needed for a shared path toward healing.
Frequently Asked Questions about Veterans Alcohol Treatment
Considering veterans alcohol treatment brings up valid questions. Here are clear, honest answers to some common concerns.
Is substance abuse considered a disability for veterans?
Substance abuse by itself is not considered a VA disability. However, if your alcohol use disorder developed as a result of a service-connected condition like PTSD, depression, or anxiety, it may be considered a secondary condition. In this case, you may be eligible for VA disability benefits.
To establish this, you need a documented medical nexus linking your service-connected condition to your alcohol use. Seeking treatment for both conditions is the best way to create the necessary medical documentation. Don’t let concerns about disability claims prevent you from getting help—proper treatment can actually strengthen your case.
Can seeking alcohol treatment affect my veterans benefits?
No. Let us be clear: seeking help for an alcohol use disorder will not negatively affect your veterans benefits. The VA views substance use disorder as a treatable medical condition, not a character flaw, and actively encourages veterans to seek care.
Your benefits are secure. The only situations that might affect benefits, such as a dishonorable discharge or felony convictions, are entirely separate from seeking treatment for your health. Reaching out for help is a protected and encouraged act. Our team at Addiction Helpline America can provide confidential reassurance based on facts, not fears.
How is stigma addressed in veterans alcohol treatment?
Stigma is a major barrier, as military culture often emphasizes self-reliance. The best veterans alcohol treatment programs tackle stigma directly.
- Changing the Narrative: Campaigns like the DoD’s “Real Warriors” frame seeking help as a sign of strength.
- Confidentiality: Your treatment is protected by federal law, allowing you to speak openly and honestly without fear of repercussions.
- Peer Support: In groups with other veterans, stigma dissolves. The shared understanding and camaraderie foster a powerful sense of community and prove you are not alone.
- Integrated Care: Treating alcohol use alongside mental health conditions like PTSD reinforces that these are legitimate medical issues requiring comprehensive care.
We connect you to programs that create these stigma-free environments, allowing you to focus on healing. Your service took courage—so does recovery.
Conclusion: Your Path to Recovery Starts Today
Simply by reading this, you’ve taken a courageous first step toward change. We’ve outlined five practical pathways to veterans alcohol treatment: starting with a veteran-specific assessment, finding accredited programs, exploring financial options, seeking integrated care for trauma, and connecting with support networks. These are real, accessible routes to recovery.
The VA wants every veteran to know: “Recovery is possible for everyone… VA offers evidence-based treatments… that are proven to be effective.” This is a fact backed by the experiences of countless service members who have reclaimed their lives.
The hardest part is often reaching out. Military culture can make asking for help feel like a weakness, but the opposite is true. Taking action to get support requires the same strength you’ve shown throughout your service.
On the other side of treatment, veterans find improved physical health, better sleep, and healed relationships. You don’t have to figure this out alone. At Addiction Helpline America, we understand the unique challenges you face. We offer free, confidential, 24/7 support to help you verify insurance, understand your options, and connect with specialized treatment centers that honor your military service.
Your service proved your resilience. Now is the time to direct that same determination toward your own healing.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.