Understanding the Scope of Veterans Addiction Treatment
Veterans addiction treatment offers specialized programs to help service members overcome substance use disorders (SUDs) by addressing challenges unique to their military experience. If you need help, here’s a quick guide:
Quick Guide to Veterans Addiction Treatment:
- VA Services: For immediate crisis support, call 988 and press 1. Visit your local VA medical center for treatment programs.
- Treatment Types: Detox, residential and outpatient rehab, medication-assisted treatment (MAT), and trauma-informed therapy.
- Common Issues: Alcohol abuse (primary issue for 65% of veterans in treatment), opioid dependence, PTSD, and chronic pain.
- Eligibility: Most veterans with an other than dishonorable discharge qualify for VA services. Other programs are available without full VA benefits.
- Cost: VA benefits cover many services. Free or low-cost options exist through state programs, Medicaid, and community resources.
Statistics show that about 11% of veterans visiting a VA facility for the first time have an SUD. For many, addiction stems from pain management or coping with invisible wounds like PTSD. However, recovery is possible through evidence-based treatments that understand the military experience.
The challenges veterans face—combat trauma, physical injuries, and readjustment difficulties—can create a perfect storm for substance misuse. While the military culture of self-reliance can make asking for help difficult, seeking treatment is a sign of strength.
At Addiction Helpline America, we connect veterans with compassionate, evidence-based care. Our experienced team helps veterans and their families steer the path to recovery and find the specialized support they’ve earned.
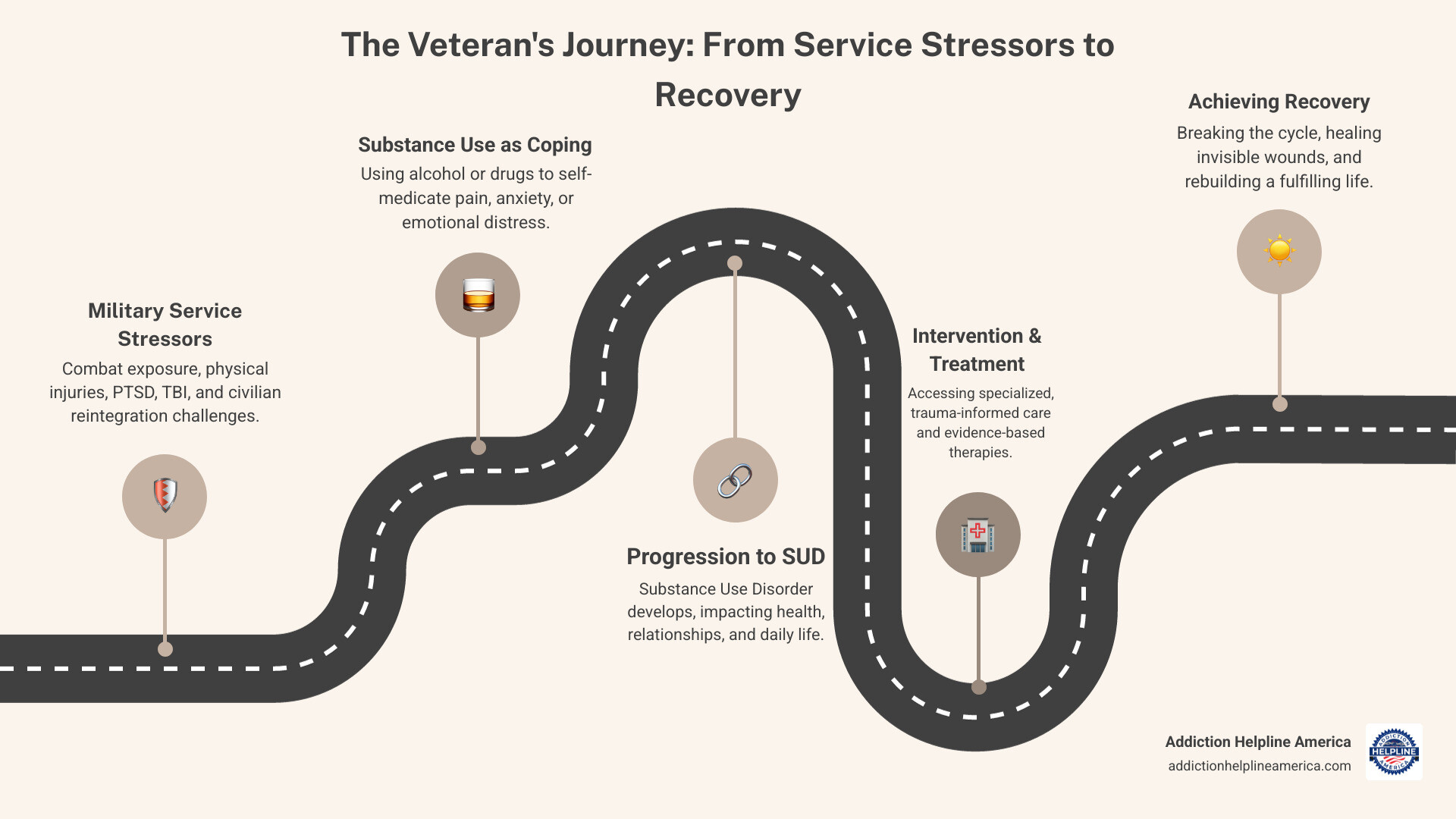
This infographic shows how military service stressors can lead to substance use disorder and highlights intervention points where veterans can access specialized treatment to break the cycle and achieve recovery.
Veterans addiction treatment terms explained:
Why Veterans Face Unique Addiction Challenges
For many veterans, returning to civilian life brings invisible wounds—trauma, pain, and adjustment struggles—that can lead to substance use as a coping mechanism. These challenges are often a direct result of their service.
Combat exposure leaves lasting psychological marks. Many veterans replay traumatic events or feel constantly on edge, and some turn to alcohol or drugs to quiet the memories and find relief.
Chronic pain from service-related injuries is another major factor. Doctors often prescribe opioids for short-term relief, but prolonged use can lead to dependence. Research shows 13% of veterans who received opioids for pain developed an opioid use disorder. The VA is actively exploring alternative pain treatments to combat this issue.
Post-Traumatic Stress Disorder (PTSD) and substance use are frequently linked. Over 2 in 10 veterans with PTSD also have a substance use disorder (SUD). Substances may temporarily numb PTSD symptoms like nightmares and anxiety, but this creates a vicious cycle where the underlying trauma remains untreated.
Traumatic Brain Injury (TBI), the “signature wound” of recent conflicts, affects over 185,000 veterans using VA services. Even mild TBI can cause cognitive issues, mood changes, and poor impulse control, increasing vulnerability to substance misuse.
The transition back to civilian life can be jarring. After the structure of the military, civilian society can feel chaotic. Many veterans struggle with finding meaningful employment and a sense of purpose, leading to isolation that can drive substance use.
Finally, the military culture of self-reliance, while a source of strength, can be a barrier to seeking help. Admitting a struggle with addiction may feel like a sign of weakness. Campaigns like the Department of Defense’s “Real Warriors. Real Battles. Real Strength” are working to change this stigma.
The Critical Role of Co-Occurring Disorders
Substance use disorders in veterans rarely exist in isolation. They are often entangled with other mental health conditions like depression, anxiety, or PTSD. This is known as a dual diagnosis or co-occurring disorders.
Statistics show that in 2020, 26.2% of veterans (5.2 million people) had a mental illness, an SUD, or both. The conditions fuel each other: substances may temporarily ease mental health symptoms but ultimately worsen them, while the untreated mental illness drives continued substance use.
This is why integrated treatment is crucial for veterans addiction treatment. This approach addresses both the SUD and mental health conditions simultaneously with the same team, which research shows is more effective and responsive to patient needs. Models like “Seeking Safety” are designed specifically for treating co-occurring PTSD and SUD.
Common Substances Abused by Veterans
While veterans may abuse various substances, clear patterns emerge.
Alcohol is the most common, with over 80% of veterans with SUDs abusing it. For 65% of veterans entering treatment, alcohol is their primary substance—nearly double the rate for civilians.
Prescription opioid dependence is a major concern, linked to high rates of chronic pain. As noted, 13% of veterans prescribed opioids for pain develop an opioid use disorder.
Other substances include methamphetamine (reported by 8% of veterans seeking treatment) and nicotine (14.6% of veterans are current smokers). Marijuana, heroin, and cocaine also contribute to SUDs among veterans, but alcohol and opioids remain the most prevalent.
A Comprehensive Guide to Veterans Addiction Treatment Programs
Finding the right recovery path can be overwhelming, but Veterans addiction treatment programs are specifically designed for the experiences and struggles of military service members. At Addiction Helpline America, we connect veterans with comprehensive, evidence-based programs that understand what you’ve been through.
Recovery looks different for everyone, which is why our network offers various levels of care, from medical detox to outpatient support. The right program depends on your current situation, substance use history, and any co-occurring challenges like PTSD or chronic pain.
Therapies are chosen for their proven effectiveness with veterans, including Trauma-Informed Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), and Eye Movement Desensitization and Reprocessing (EMDR). What makes these programs truly veteran-focused is the environment of camaraderie and trust, with specialized support for co-occurring disorders, chronic pain, military sexual trauma (MST), and reintegration into civilian life.
| Feature | Addiction Helpline America’s Veteran-Focused Programs |
|---|---|
| Levels of Care | Medical Detox, Residential, Partial Hospitalization (PHP), Intensive Outpatient (IOP), Outpatient, Aftercare |
| Therapies Offered | Trauma-Informed CBT, DBT, EMDR, Motivational Interviewing, 12-Step Facilitation, Seeking Safety, Anger Management, Family Therapy |
| Specialized Focus | Co-occurring disorders (PTSD, Depression, Anxiety), Chronic Pain Management, Military Sexual Trauma (MST) support, Reintegration support |
| Environment | Patient-centered, trauma-informed, emphasizing camaraderie and trust |
| Support Systems | Veteran peer support, family programming, holistic approaches, vocational support |
| Accessibility | In-person, virtual, and hybrid options available across our network |
Addiction Helpline America’s Veteran-Focused Treatment Services
Our network programs guide you through every stage of recovery.
- Medically managed detoxification: Provides 24/7 medical supervision to ensure a safe and comfortable withdrawal process.
- Residential rehabilitation programs: Offer a structured, immersive environment away from daily triggers, where you live on-site and focus entirely on healing with comprehensive services.
- Intensive outpatient programs (IOP): Allow you to live at home while receiving substantial treatment several hours a day, multiple days a week, accommodating work or family responsibilities.
- Medication-assisted treatment (MAT): Combines FDA-approved medications (like buprenorphine or naltrexone) with counseling to reduce cravings and withdrawal symptoms, particularly for opioid and alcohol use disorders.
- Individual and group counseling: Forms the core of recovery, offering one-on-one therapy to address underlying issues and group sessions to connect with other veterans on similar journeys.
- Trauma-informed care: A fundamental approach ensuring all care is delivered in a way that creates safety and trust, acknowledging past trauma without causing re-traumatization.
- Veteran peer support: Connects you with veterans who have successfully steerd recovery. They act as guides who understand military culture and offer invaluable encouragement.
At Addiction Helpline America, we’re dedicated to matching you with the program that fits your specific situation and needs. Learn more about Addiction Helpline America’s treatment options.
Community Support and Holistic Approaches
Recovery is about building a life worth living. Community and holistic approaches are key.
- Support groups for veterans: Groups like Alcoholics Anonymous (AA), Narcotics Anonymous (NA), and SMART Recovery provide ongoing peer support. Connecting with other veterans in these settings adds a powerful layer of shared understanding.
- Holistic therapies: Many programs integrate art therapy, music therapy, yoga, and mindfulness to help manage stress and process emotions. These are powerful tools for reconnecting with yourself.
- Adventure therapy: Activities like hiking or rock climbing build confidence, trust, and coping skills in a tangible way.
- Peer support specialists: These are individuals in recovery who use their lived experience to guide and encourage you, offering a powerful message of hope.
Effective therapies for veterans include CBT, DBT, EMDR, Seeking Safety, and Anger Management Counseling, all of which address the specific challenges you face.
How to Access Immediate Crisis Support
If you or a veteran you know is in immediate danger, help is available 24/7.
The Veterans Crisis Line is staffed by qualified responders who understand military culture. You can reach them three ways:
- Dial 988 then press 1
- Text 838255
- Start a confidential chat online
This service is confidential and available to all veterans, even if not enrolled in VA benefits.
If someone is experiencing an overdose or is in immediate danger of self-harm, dial 911 or go to the nearest emergency room or VA medical center. Every minute matters. For urgent but non-life-threatening needs, contact your local VA medical center.
Navigating Access and Affordability for Treatment
One of the biggest barriers to Veterans addiction treatment is the perceived cost. However, more affordable options exist than many realize. At Addiction Helpline America, we help veterans steer the system to find care that fits their budget. Cost should not prevent you from seeking recovery.
Eligibility for Veterans Addiction Treatment Programs
Accessing VA substance use disorder programs typically starts with enrolling in VA health care. You can apply online, at a VA medical facility, or by contacting the VA enrollment office.
Your discharge status is a factor, as you generally need a discharge under other than dishonorable conditions. However, exceptions can be made, so it’s always worth inquiring.
Combat veterans receive priority care and may qualify for free counseling at one of 300 community Vet Centers, even without full VA benefits. Veterans of OEF/OIF/OND can request a specific coordinator at their local VA to help steer services.
If you’re unsure about your eligibility, our team at Addiction Helpline America can help you understand the requirements and find the right resources. Check your eligibility for treatment.
Affordable Veterans Addiction Treatment Options
Multiple pathways exist to make treatment affordable or even free.
- VA health benefits cover many SUD treatment services for eligible veterans. Costs can vary based on eligibility, income, and disability status.
- Private insurance, including TRICARE for active duty, retired military, and families, and CHAMPVA for eligible spouses and children, typically covers addiction treatment. Our network facilities work with most major providers.
- Medicaid can cover most or all treatment costs for those who qualify based on income. Many programs in our network accept Medicaid.
- State-funded programs offer free or low-cost treatment based on income and residency, supported by federal grants.
- Community resources like non-profit organizations and health clinics often provide free or low-cost services. The SAMHSA treatment locator can help you find them.
- Sliding scale fees are offered by some private centers, adjusting the cost based on your income.
Don’t let financial concerns stop you. Our team provides free guidance on finding affordable care that meets your needs.
Support for Families and Loved Ones
Addiction impacts the entire family. Supporting loved ones is a crucial part of Veterans addiction treatment, as family healing strengthens the foundation for recovery.
Family members may have their own benefits through TRICARE or CHAMPVA. The VA also provides resources for family caregivers. You can find more information at Healthcare for spouses, dependents, and family caregivers.
Many treatment centers offer family programming, including educational sessions and counseling to improve communication and heal relationships. Mutual support groups like Al-Anon, Nar-Anon, and Alateen provide free, confidential support for families affected by a loved one’s substance use. These resources recognize that family members need their own support to steer the recovery journey.
Frequently Asked Questions about Veterans Addiction Treatment
Can a veteran get disability benefits for a substance use disorder?
The VA generally does not rate a substance use disorder (SUD) as a primary service-connected disability. However, an SUD may be considered a secondary condition if you can prove it was caused or worsened by a service-connected condition like PTSD, depression, or anxiety.
For example, if a veteran with service-connected PTSD develops an alcohol use disorder as a way to cope with symptoms, the SUD could be linked as secondary to the PTSD. This requires a thorough evaluation by VA medical professionals to establish a clear causal link. If service-connection is granted, you may be eligible for disability compensation and expanded coverage for Veterans addiction treatment.
What help is available for veterans who do not have insurance?
Even without insurance, multiple pathways to care exist.
- Vet Centers: Offer free, confidential counseling for combat veterans at 300 community-based locations.
- Community health clinics: Often provide addiction treatment on a sliding scale based on income.
- Non-profit organizations: Groups like the Salvation Army and other veteran-specific charities may offer free or low-cost treatment.
- State and local government programs: Fund addiction treatment for residents regardless of insurance status. Contact your state health department or SAMHSA’s National Helpline (1-800-662-4357).
- Emergency care: In an overdose or severe withdrawal, emergency rooms must provide stabilizing care regardless of ability to pay.
At Addiction Helpline America, we specialize in helping uninsured veterans explore every option to find affordable care.
What is the difference between a treatment center and a support center?
Understanding the distinction helps you choose the right resource for your needs.
Treatment centers, like VA Medical Centers and facilities in our network, are clinical healthcare settings. They are staffed by medical professionals (doctors, therapists) who diagnose and treat addiction. Services include medical detox, residential care, medication-assisted treatment, and evidence-based therapies. They provide structured programs and are bound by HIPAA privacy laws.
Support centers, like Vet Centers and peer support groups (AA, NA), offer non-medical counseling, peer encouragement, and resources for readjustment. They provide a community setting for sharing experiences and mutual support. While they are vital for long-term recovery, they do not provide clinical interventions or prescribe medication. Confidentiality is based on group norms.
Both are valuable and often work best together. Many veterans begin with clinical care at a treatment center and continue their recovery with ongoing community support.
Conclusion: Your Path to Recovery Starts Today
If you are a veteran struggling with addiction, know this: recovery is possible. The challenges of military service—combat exposure, chronic pain, PTSD, and the difficult return to civilian life—are real, but they do not have to define your future.
Asking for help is not a weakness; it is a sign of strength. Reaching out for Veterans addiction treatment is taking decisive action, a skill you have already mastered.
Effective pathways to healing are available now. From medical detox and residential treatment to trauma-informed therapies and peer support, there is a program that can help you rebuild your life. Options exist regardless of your financial situation, whether through VA benefits, private insurance, or community resources.
At Addiction Helpline America, we specialize in connecting veterans with treatment programs that understand your unique experiences. Our guidance is free, confidential, and personalized to match you with the right level of care.
Your service to this country was extraordinary. Now, it’s time to serve yourself with the same courage. Recovery is not about erasing the past, but learning to build a hopeful future with better tools and stronger support.
Today can be the day everything changes. We’re here to help, 24/7. No judgment, just real people ready to connect you with the specialized care you’ve earned.
Find a rehab center that understands veterans’ needs.
Your path to recovery starts today. Let’s take that first step together.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.