Why Veterans Face Unique Challenges with Addiction
Veteran addiction treatment provides specialized care for the unique challenges faced by those who have served. It combines treatment for combat trauma, co-occurring conditions like PTSD, and chronic pain management with evidence-based therapies, peer support, and staff trained in military culture.
Key Facts About Veteran Addiction Treatment:
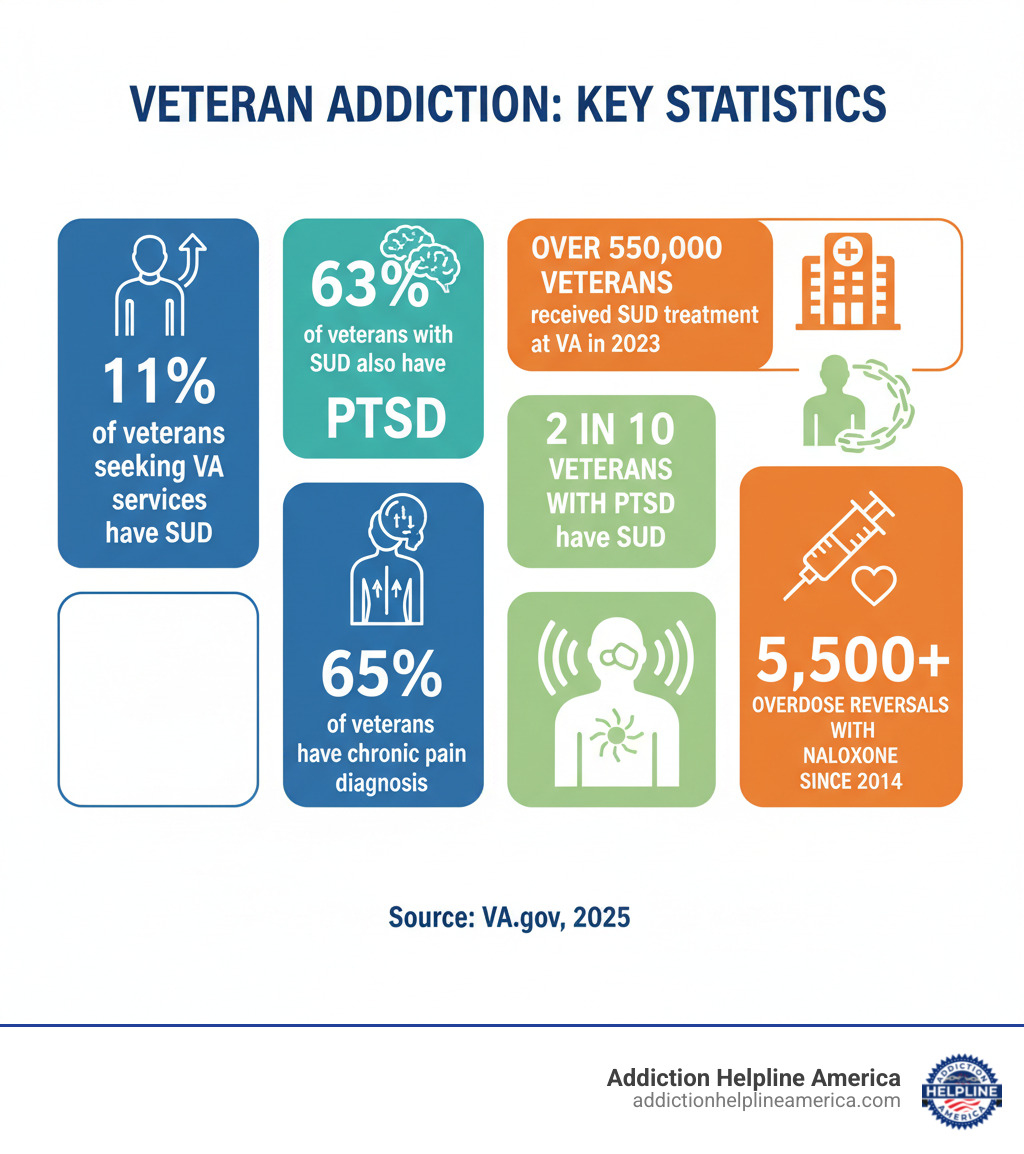
- Prevalence: 11% of veterans seeking VA services meet criteria for a substance use disorder
- Co-occurring Conditions: 63% of veterans with substance use disorders also have PTSD
- Available Programs: Detox, residential rehab, intensive outpatient, standard outpatient, and aftercare
- Treatment Access: VA healthcare, TRICARE, Community Care Program, and private facilities
- Crisis Support: Veterans Crisis Line (988, press 1) available 24/7
- Specialized Therapies: CBT, EMDR, trauma-informed care, and medication-assisted treatment
Military service takes a toll, leaving veterans vulnerable to addiction. They face combat trauma, chronic pain, and a difficult transition to civilian life. Over 65% of veterans have chronic pain, often treated with addictive opioids, and substance use is a factor in many of the 6,146 veteran suicides in 2020.
The good news is that recovery is possible. Specialized programs provide safe spaces where veterans can heal alongside peers who understand their struggles. These programs use evidence-based treatments to address addiction and underlying conditions like PTSD, TBI, and military sexual trauma (MST).
Addiction Helpline America connects veterans and their families with these specialized veteran addiction treatment resources. Our team offers 24/7 support, referrals, and guidance through VA benefits and community programs to ensure every veteran can access the care they’ve earned.
Veteran addiction treatment terms simplified:
Understanding Why Veterans Are at a Higher Risk for Addiction
The return to civilian life can bring unexpected struggles that lead to substance use. The experiences that shape a person in the military don’t disappear when the uniform comes off.
- Combat Exposure: The trauma of war can lead veterans to self-medicate with alcohol or drugs to cope with haunting memories, flashbacks, and nightmares.
- Transition to Civilian Life: Military service provides structure, camaraderie, and purpose. The loss of this identity can create a void that substances seem to fill.
- Chronic Pain Management: The physical demands of service take a lasting toll. Over 65% of veterans have a chronic pain diagnosis, and many are prescribed opioids that can lead to dependence and addiction.
- Self-Medication for Mental Health: Untreated anxiety, nightmares, and emotional numbness can lead veterans to use substances for temporary escape, which quickly spirals into dependency.
- High-Stress Environment: Military training to “push through” can make it difficult for veterans to recognize when coping strategies have become an addiction and to ask for help.
The Role of Co-Occurring Mental Health Conditions
Mental health and substance use disorders are deeply connected, with one often fueling the other. Up to 50% of Afghanistan and Iraq war veterans have a diagnosed mental health disorder, increasing their risk for substance use.
- Post-Traumatic Stress Disorder (PTSD): The symptoms of PTSD—intrusive memories, hypervigilance, and sleep problems—are exhausting. 63% of recently surveyed veterans from Afghanistan and Iraq with SUD also had PTSD. Overall, 2 in 10 veterans with PTSD also have a substance use disorder. The link between PTSD and SUD is well-documented.
- Traumatic Brain Injury (TBI): Affecting over 185,000 veterans in the VA system, even mild TBIs can cause concentration problems, mood swings, and impulsiveness that increase vulnerability to substance misuse.
- Depression and Anxiety: Widespread among veterans, these conditions can be triggered by trauma and reintegration challenges. Substances may feel like a temporary lifeline but ultimately worsen the problem.
- Military Sexual Trauma (MST): Experienced by about 1 in 5 female veterans, MST can lead to severe PTSD and depression. Survivors often turn to substances to cope with overwhelming psychological pain.
Effective veteran addiction treatment must address these interconnected issues simultaneously.
Common Substances of Abuse Among Veterans
While struggles vary, certain patterns of substance use are common among veterans.
- Alcohol: Misuse is widespread, with one study finding 25% of soldiers misused alcohol post-deployment. It’s a legal and accessible coping mechanism for stress and trauma. Specialized Veterans Alcohol Treatment is available.
- Prescription Opioids: Prescribed for legitimate chronic pain, these medications can quickly lead to tolerance, dependence, and addiction.
- Marijuana: Often used to manage PTSD or chronic pain, regular use can still lead to dependence and complicate mental health conditions.
- Heroin and Cocaine: For some, addiction progresses from prescription opioids to heroin. Heroin and cocaine account for over 10% and 6% of veteran treatment admissions, respectively.
The scope is significant: 11% of veterans seeking VA services for the first time met the criteria for a substance use disorder. These are people who served our country and now need specialized care.
Barriers and Challenges in Veteran Addiction Treatment
Getting help should be simple, but many veterans face barriers to veteran addiction treatment that are rooted in military culture and logistical challenges.
- Stigma in Military Culture: Service members are trained to be self-reliant and tough. Admitting the need for help can feel like a personal failure, which is why approximately 60% of veterans with mental health issues do not seek treatment.
- Concerns About Security Clearance: Some veterans fear that seeking treatment could jeopardize their security clearance and career opportunities, though policies are in place to protect them.
- Difficulty Navigating the VA System: The VA offers incredible resources, but understanding eligibility, scheduling, and navigating the bureaucracy can be overwhelming for someone already battling addiction.
- Geographic Isolation: Nearly 41% of veterans in VA programs live in rural areas, where the nearest specialized treatment center may be hours away, making consistent care difficult.
Overcoming Problems to Accessing Care
These barriers are real, but solutions are increasingly available.
- Telehealth Services: Veterans can connect with counselors and specialists from home, overcoming geographic barriers and reducing stigma.
- VA Community Care Program: This program allows eligible veterans to receive covered treatment from approved local providers if VA facilities are too far, wait times are too long, or specialized care isn’t available. Find more information on VA Community Care.
- Combining Benefits: Veterans can often use VA benefits alongside private insurance, Medicare, or Medicaid to expand their options and reduce costs.
- Housing and Employment Assistance: Since 70% of homeless veterans have a substance use disorder, programs like HUD-VASH that provide stable housing are a critical foundation for recovery. Find help for Homeless Veterans.
Unique Challenges for Women Veterans
Women veterans face additional challenges in a system historically designed for men.
- Military Sexual Trauma (MST): About 1 in 5 female veterans has been diagnosed with MST, requiring specialized, gender-sensitive care to address this complex trauma.
- Childcare Needs: As primary caregivers, many women veterans find it nearly impossible to attend treatment without access to affordable, reliable childcare.
- Need for Gender-Specific Care: Treatment settings dominated by men can be uncomfortable or re-traumatizing. Programs designed for women create a safer, more effective healing environment. The VA offers dedicated VA resources for Women Veterans.
You don’t have to figure this out alone. Solutions exist for every barrier.
Comprehensive Veteran Addiction Treatment Programs
Veteran addiction treatment is most effective when it’s built around the individual’s unique journey. A comprehensive approach involves several levels of care.
- Medical Detoxification: The first step for many is safely managing withdrawal symptoms in a supervised medical environment. This stabilizes the body for the deeper work of recovery.
- Residential Rehabilitation: For those needing intensive support, residential programs provide a structured, 24/7 environment focused on recovery. In 2023, over 23,000 veterans were served at VA residential sites.
- Intensive Outpatient Programs (IOP): IOPs offer substantial therapeutic support several times a week while allowing veterans to live at home, balancing treatment with daily life.
- Standard Outpatient Care: This involves regular therapy sessions on a less intensive schedule, ideal for those with milder issues or as a step-down from a higher level of care.
- Aftercare and Relapse Prevention: Recovery is a long-term process. Aftercare provides ongoing support to help veterans steer life after treatment and prevent relapse.
Benefits of Specialized Veteran Addiction Treatment
Programs designed specifically for veterans offer unique advantages that general treatment may lack.
- Peer Support: Healing alongside fellow veterans creates a powerful bond of trust and understanding. There’s no need to explain military culture—they just “get it.”
- Staff with Military Cultural Competency: Therapists who understand military terminology and values can provide more effective and respectful care.
- Integrated Treatment for Co-Occurring Disorders: These programs treat substance use and underlying conditions like PTSD, TBI, or depression simultaneously, which is critical for success.
- Trauma-Informed Care: Every aspect of treatment is designed to create a safe environment and avoid re-traumatization, recognizing the high prevalence of trauma among veterans.
Addiction Helpline America can help you find a VA-affiliated clinic near you that offers these specialized benefits.
Evidence-Based Therapies for Lasting Recovery
Effective programs use therapies with proven track records for helping veterans.
- Cognitive Behavioral Therapy (CBT): Helps veterans identify and change negative thought patterns and behaviors related to substance use.
- Motivational Interviewing (MI): A collaborative style that helps individuals find their own internal motivation to change.
- Eye Movement Desensitization and Reprocessing (EMDR): A specialized therapy that helps process traumatic memories, reducing their emotional power and the need to self-medicate.
- Family Therapy: Involves loved ones in the healing process to repair relationships, improve communication, and build a strong support system.
- Group Counseling: Provides a structured therapeutic setting to learn new skills and gain perspective from other veterans.
Other effective approaches include Motivational Improvement Therapy (MET), Contingency Management (CM), and 12-Step facilitation. SAMHSA offers a comprehensive guide to evidence-based practices.
Finding Support: VA Programs and Community Resources
A comprehensive network of VA programs and community resources exists to support veterans through recovery. The challenge is often knowing where to find and access this help.
The starting point for many is VA healthcare enrollment. If enrolled, ask your primary care provider for a mental health referral to access veteran addiction treatment. If not, you can apply online or at your nearest VA medical center. Key resources include:
- VA Substance Use Disorder (SUD) Program Locator: This online tool helps you find local VA treatment programs for all types of substance use challenges.
- Vet Centers: These community-based centers offer no-cost, confidential counseling for addiction, PTSD, and readjustment challenges in a welcoming, non-clinical setting.
- Medication-Assisted Treatment (MAT): The VA offers MAT, which combines FDA-approved medications (like buprenorphine for opioid use or naltrexone for alcohol use) with counseling to treat the physical and psychological aspects of addiction.
- Harm Reduction: The VA supports strategies to save lives, such as providing naloxone to reverse opioid overdoses. Since 2014, the VA has reported more than 5,500 overdose reversals with naloxone, giving thousands a second chance at recovery.
How Family and Friends Can Help
Family and friends play a powerful role in a veteran’s recovery, but they need support too.
- Communicate Openly: Express your concerns with care and honesty, focusing on your love for them, not judgment. Let them know you’re ready to help find treatment.
- Encourage Treatment Without Judgment: Addiction is a medical condition, not a moral failing. Offer practical help, like researching options or arranging transportation.
- Set Healthy Boundaries: Supporting someone doesn’t mean enabling their addiction. It’s okay to set limits, such as not providing money for substances, to protect yourself and create space for recovery.
- Find Support for Yourself: You are not alone. Groups like Al-Anon for families of alcoholics and the VA Caregiver Support Program offer resources and community for those supporting a veteran.
Addiction Helpline America can help you steer these resources. We provide free, confidential guidance 24/7 to connect you with the right programs.
Frequently Asked Questions about Veteran Addiction Treatment
When a veteran is struggling, families and friends have urgent questions. Here are answers to some of the most common ones.
How do I know if a veteran I love has a substance use problem?
Veterans are often skilled at masking their struggles, but there are common signs to watch for:
- Behavioral Changes: Increased irritability, withdrawal, secrecy, or loss of interest in hobbies.
- Neglected Responsibilities: Trouble keeping a job, missing family events, or a decline in personal hygiene.
- Financial or Legal Trouble: Unexplained requests for money, mounting bills, or arrests related to substance use.
- Hiding Substance Use: Becoming defensive or evasive when asked about their activities or time spent alone.
- Withdrawal Symptoms: Becoming shaky, sweaty, or anxious when they can’t use their substance of choice.
- Inability to Quit: Making promises to stop but being unable to follow through, which is a key sign of addiction, not a lack of willpower.
If these signs are familiar, trust your instincts. Reaching out for professional guidance is a loving and necessary step toward getting them help with veteran addiction treatment.
Is veteran addiction treatment covered by insurance?
Yes, veterans have several options for covering the cost of treatment.
- VA Health Benefits: For enrolled veterans, SUD treatment is typically covered with minimal to no out-of-pocket costs. Over 550,000 veterans received SUD treatment at the VA in FY 2023.
- TRICARE: This covers service members, retirees, and their families for detox, residential, and outpatient care.
- Medicare and Medicaid: These programs can work alongside VA benefits or cover treatment outside the VA system.
- Private Insurance: Coverage through an employer or private plan often includes addiction treatment and can be combined with VA benefits.
- Community Care Network: If the VA can’t provide timely or local care, this program authorizes and covers treatment with approved community providers.
Navigating insurance is complex, but we can help. Addiction Helpline America can verify your benefits and find an affordable path to treatment.
What is the first step to getting help for a veteran in crisis?
If a veteran is in immediate danger of harming themselves or others, act now.
- Call the Veterans Crisis Line: Dial 988 and press 1. This 24/7 confidential line connects you with trained mental health professionals who understand military culture.
- Chat or Text: For those who prefer not to call, you can chat online with the Veterans Crisis Line or text 838255 to connect with a counselor.
- Go to the Nearest Emergency Room: For any medical emergency, including overdose or severe withdrawal, an ER can provide immediate stabilization.
- Call 911: For any life-threatening emergency, do not hesitate to call 911.
Reaching out for help is a sign of strength. After the immediate crisis is managed, Addiction Helpline America can help find a long-term veteran addiction treatment program.
Your Path to Recovery Starts Today
If you’ve read this far, you’ve taken a courageous step. The journey from military service to civilian life can include unexpected struggles with addiction and mental health, stemming from combat trauma, chronic pain, and the challenges of reintegration.
But here’s what we want you to remember most: recovery is possible. Over 550,000 veterans received treatment for substance use disorders at VA in 2023. Each of those numbers represents a person who decided that their story didn’t end with addiction.
Specialized care makes all the difference. Veteran addiction treatment programs understand military culture. They offer peer support from people who truly “get it,” staff trained in trauma-informed care, and integrated treatment for the co-occurring conditions that so often accompany substance use disorders.
We know that taking the first step can feel overwhelming. You might be worried about stigma, unsure how to pay for treatment, or simply exhausted from carrying this burden alone. That’s exactly why Addiction Helpline America exists. We provide free, confidential guidance to help you find the right veteran addiction treatment program for your specific situation. Our team understands VA benefits, TRICARE, private insurance, and the Community Care Program. We can connect you with specialized treatment centers across all fifty states—from Alabama to California, Florida to Texas, and everywhere in between.
Your service to this country was extraordinary. You answered the call when your nation needed you. Now it’s time to let others answer your call. Whether you need help for yourself or you’re supporting a veteran you love, we’re here 24/7 to guide you toward healing.
Your path to recovery starts with a single conversation. Find a personalized drug and substance abuse treatment program today. You’ve already shown tremendous courage by reading this far. Take the next step—you’ve earned it.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.