
Understanding Your Path to Recovery with UnitedHealthcare
UnitedHealthcare Insurance Coverage for Drug and Alcohol Rehab is available to millions of members, offering crucial support for addiction treatment. If you’re looking for help, here’s what you need to know.
Yes, UnitedHealthcare covers drug and alcohol rehabilitation. As one of the nation’s largest insurers, serving over 151 million people, UHC provides comprehensive substance use disorder treatment coverage, a requirement strengthened by the Affordable Care Act. Coverage typically includes medical detox, inpatient and outpatient programs, medication-assisted treatment (MAT), and therapy. Your out-of-pocket costs will depend on your specific plan (HMO, PPO, Medicare, etc.), its metal tier (Bronze, Silver, Gold), and whether you use in-network providers.
To get started, you can verify your benefits by calling the number on your insurance card, logging into MyUHC.com, or contacting UnitedHealthcare’s 24/7 Substance Use Helpline at 1-855-780-5955. Key factors like medical necessity, pre-authorization, deductibles, and copays will determine your final costs.
Navigating insurance can be stressful, but it shouldn’t be a barrier to recovery. At Addiction Helpline America, we specialize in breaking down complex UnitedHealthcare policies into simple, actionable steps. This guide will walk you through what’s covered, how plans differ, and how to get the help you need.
Does UnitedHealthcare Cover Drug and Alcohol Rehab?
Yes, UnitedHealthcare does cover drug and alcohol rehabilitation services. This is not an optional perk; it’s a requirement under federal law.
Two key laws ensure this coverage. The Affordable Care Act (ACA) classifies addiction treatment as an essential health benefit, while the Mental Health Parity and Addiction Equity Act (MHPAEA) requires insurers to cover substance abuse services as generously as they cover medical care. You can learn more from Healthcare.gov’s overview of this coverage.
This means UnitedHealthcare Insurance Coverage for Drug and Alcohol Rehab is a core part of your plan. Most of these benefits are managed through Optum, UHC’s behavioral health division, which provides access to a vast network of treatment providers and confidential support.
What Types of Substance Use Disorders Are Covered?
UnitedHealthcare’s coverage is based on medical necessity, not the specific substance you’re struggling with. This comprehensive approach includes treatment for:
- Alcohol Use Disorder (AUD)
- Opioid Use Disorder (OUD), including prescription painkillers and heroin
- Stimulant Addiction (cocaine, meth, etc.)
- Prescription Drug Abuse (benzodiazepines, sedatives)
- Polysubstance Abuse (addiction to multiple substances)
Crucially, coverage also extends to co-occurring disorders (or dual diagnosis), where a substance use disorder exists alongside a mental health condition like depression, anxiety, or PTSD. UnitedHealthcare supports integrated programs that treat both conditions simultaneously, which is essential for effective, long-term recovery.
A Breakdown of UnitedHealthcare Plans and Coverage Tiers
Not all UnitedHealthcare plans are the same. Your UnitedHealthcare Insurance Coverage for Drug and Alcohol Rehab and out-of-pocket costs depend on your specific plan, which can be an employer-sponsored Group benefit plan from UHC, a marketplace plan, or a government program like Medicare or Medicaid. While all plans must cover addiction treatment, the financial details vary significantly.
How Your Plan Type Affects UnitedHealthcare Insurance Coverage for Drug and Alcohol Rehab
Your plan’s structure—typically an HMO or PPO—is a major factor in your treatment options and costs.
- HMO (Health Maintenance Organization) plans have lower premiums but are more restrictive. You must use in-network providers and will likely need a referral from your primary care physician (PCP) for rehab. Going out-of-network usually means paying the full cost yourself.
- PPO (Preferred Provider Organization) plans offer more flexibility. You can see specialists without a referral and use out-of-network providers, though you’ll pay more. Staying in-network is always the most affordable option.
UnitedHealthcare also offers variations like UnitedHealthcare Choice plans (HMO-like), UnitedHealthcare Choice Plus plans (a hybrid with some out-of-network coverage), and UnitedHealthcare Options – PPO plans (traditional PPOs). Regardless of your plan, using in-network providers will save you the most money.
Understanding Metal Tiers: Bronze, Silver, Gold & Platinum
If you have a marketplace plan, it will fall into a metal tier that dictates how you and your insurer split costs. As explained by Healthcare.gov’s guide to ‘metal’ categories, these tiers are about cost-sharing, not quality of care.
- Bronze: Lowest monthly premium, but highest out-of-pocket costs (deductibles, coinsurance). You pay more when you need care.
- Silver: A balance of moderate premiums and moderate costs for care.
- Gold & Platinum: Highest premiums, but lowest out-of-pocket costs. These plans are often best if you anticipate needing significant care like rehab.
Key terms to know include your deductible (what you pay before insurance pays), copayment (a flat fee for a service), coinsurance (your percentage of the cost), and out-of-pocket maximum (the most you’ll pay in a year for covered services).
Coverage for Medicare and Medicaid Recipients
UnitedHealthcare is a major provider of government-funded plans.
- Medicare: For those 65+ or with certain disabilities, Original Medicare Part A covers inpatient hospital care, while Part B covers outpatient services. Many people opt for United Healthcare Medicare plans like Medicare Advantage (Part C), which are private plans that often offer more comprehensive addiction treatment benefits.
- Medicaid: For low-income individuals, United Healthcare Medicaid plans provide robust substance abuse coverage. However, benefits are state-specific, so coverage details vary significantly by location. For more information, see our guide on What Drug Rehab Centers Accept Medicaid.
For both Medicare and Medicaid, it is essential to verify the specific benefits of your plan in your state.
What Specific Addiction Treatments Does UnitedHealthcare Cover?
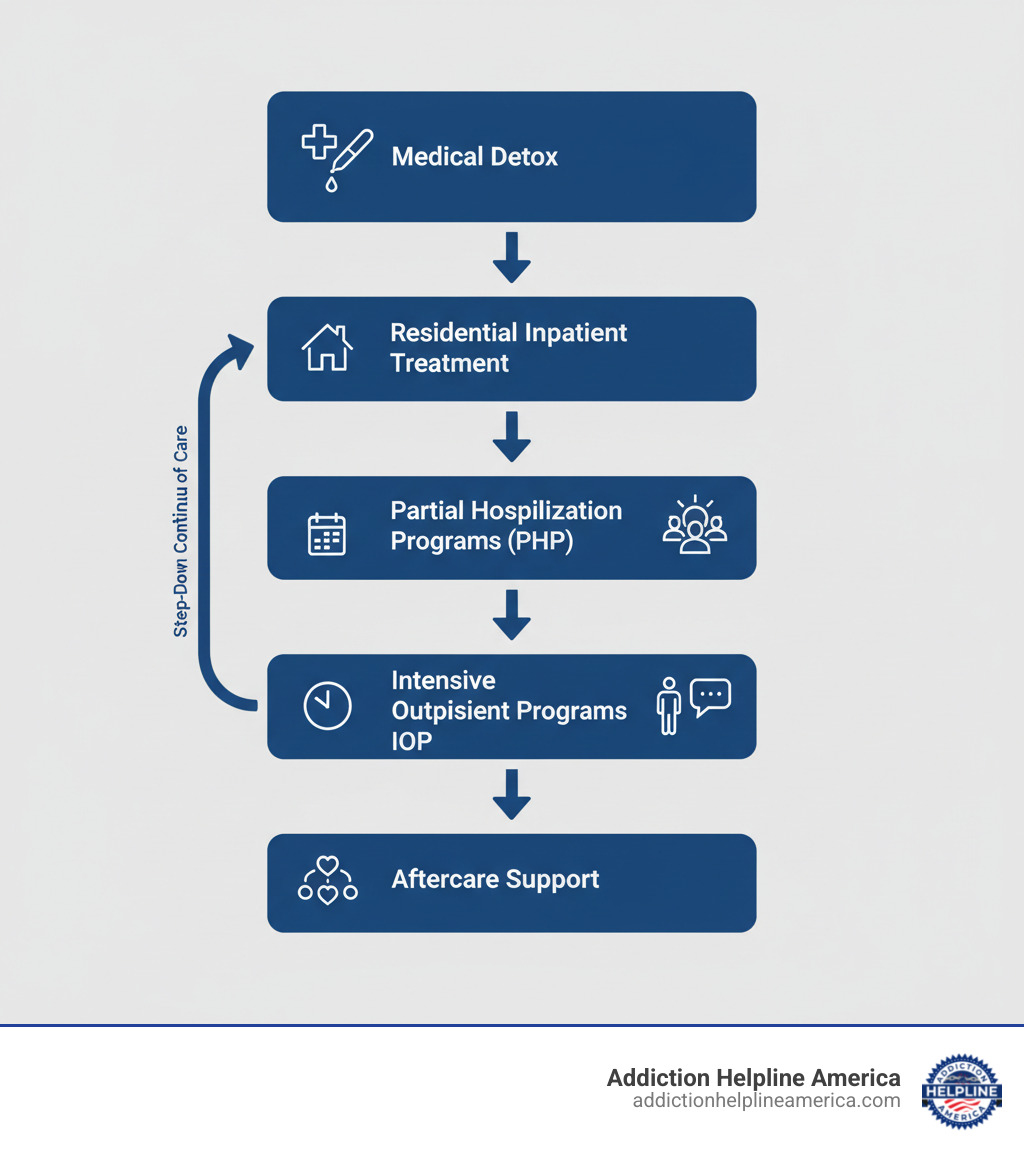
UnitedHealthcare Insurance Coverage for Drug and Alcohol Rehab includes a full continuum of care, ensuring you get the right level of treatment at the right time. Coverage is based on medical necessity, often determined by American Society of Addiction Medicine (ASAM) criteria. This step-down approach allows you to move from intensive care to more flexible programs as you progress in recovery, as outlined in NIDA’s Types of Treatment Programs.

Here are the specific treatments generally covered by UnitedHealthcare plans.
Medical Detox
Detox is the first step for many, providing safe, medically supervised withdrawal management. This is critical for substances like alcohol, benzodiazepines, and opioids, where withdrawal can be dangerous. UHC plans typically cover both inpatient detox (24/7 medical care) and outpatient detox for less severe cases.
Inpatient and Residential Rehab
These programs offer a structured, 24/7 therapeutic environment away from daily triggers. Treatment includes individual and group therapy, life skills training, and holistic activities. UnitedHealthcare covers both short-term rehab (15-90 days) and long-term residential treatment when medically necessary.
Outpatient Programs (PHP & IOP)
Outpatient care allows you to receive intensive treatment while living at home.
- Partial Hospitalization Programs (PHP) are the most intensive, often running 5 days a week for several hours.
- Intensive Outpatient Programs (IOP) are more flexible, typically involving a few sessions per week, allowing you to work or attend school.
- Standard outpatient care involves weekly or bi-weekly therapy sessions for ongoing support.
Medication-Assisted Treatment (MAT)
MAT combines FDA-approved medications with counseling to treat opioid and alcohol use disorders. It is an evidence-based approach that helps reduce cravings and normalize brain chemistry. Covered medications often include:
- For opioid use: Buprenorphine (Suboxone), Methadone, and Naltrexone (Vivitrol).
- For alcohol use: Naltrexone, Acamprosate, and Disulfiram (Antabuse).
These prescriptions are typically covered when filled at an in-network pharmacy.
Therapy and Counseling
Therapy is the foundation of recovery. UnitedHealthcare covers various evidence-based approaches that are integrated into all levels of care:
- Individual, group, and family therapy to address root causes, build support, and heal relationships.
- Cognitive Behavioral Therapy (CBT) to change negative thought patterns.
- Dialectical Behavior Therapy (DBT) to build coping and emotional regulation skills.
- Motivational Interviewing to help you find your own motivation for change.
How to Verify Your UnitedHealthcare Insurance Coverage for Drug and Alcohol Rehab
Before starting treatment, you must verify what your insurance will cover to avoid unexpected costs. This process confirms your benefits, prior authorization requirements, and which facilities are in-network. While it may seem daunting, it’s a crucial step. If you need help, our team at Addiction Helpline America offers a free service to Verify Insurance with a treatment specialist.

While UHC may not require formal prior authorization for all services, pre-notification is often necessary, especially for medical detox and inpatient stays, to establish medical necessity.
Step-by-Step Guide to Checking Your Benefits
Here are the most effective ways to get the answers you need:
- Call the number on your insurance card. This is the most direct way to speak with a representative who can explain your deductible, copays, coinsurance, and in-network providers.
- Log into your MyUHC member portal. The MyUHC.com website gives you 24/7 access to your plan documents, benefit details, and a provider search tool.
- Review your plan documents. Your Summary of Benefits and Coverage (SBC) provides a plain-language breakdown of what your plan covers.
- Contact a treatment provider for help. Most reputable rehab centers, including our partners, offer complimentary insurance verification. We can call UHC on your behalf and explain your benefits clearly.
Understanding In-Network vs. Out-of-Network Costs
This is one of the biggest factors affecting your final bill.
- In-network providers have a contract with UnitedHealthcare to offer services at a pre-negotiated, lower rate. Your costs will be significantly lower.
- Out-of-network providers do not have a contract, so they can charge higher rates. PPO plans may offer some coverage, but you’ll pay much more. HMO plans typically offer no coverage for out-of-network care.
To maximize your benefits, always choose an in-network provider.
Using the UnitedHealthcare Substance Use Helpline
UnitedHealthcare offers a dedicated, free, and confidential resource for members. The Substance Use Helpline details from UHC explain that this service is available 24/7/365.
By calling 1-855-780-5955 (TTY 711), you can speak with a trained recovery advocate who can help you understand your benefits, find in-network providers, and get a cost estimate for treatment. This is an invaluable resource included with your plan.
Managing Rehab Costs and Financial Options
Even with good UnitedHealthcare Insurance Coverage for Drug and Alcohol Rehab, you will likely have some out-of-pocket costs like deductibles and copayments. However, the financial burden of treatment should never prevent you from getting help. Our Paying for Addiction Treatment guide offers a detailed breakdown of your options.
Understanding Costs with UnitedHealthcare Insurance Coverage for Drug and Alcohol Rehab
Your costs depend on your plan’s metal tier, deductible, and whether you’ve met it. Higher-premium plans (Gold) lead to lower out-of-pocket costs for treatment, while lower-premium plans (Bronze) mean you pay more when you need care. Every plan has an out-of-pocket maximum, which is the most you’ll pay for covered services in a year.
| Plan Tier | Deductible (Example) | Coinsurance for SUD Treatment (Example) | Copay for Office Visits (Example) |
|---|---|---|---|
| Bronze | $8,300 | 50% | $100+ |
| Silver | $3,600 | 40% | $100 |
| Gold | $2,000 | 20% | $50 |
Note: These are illustrative examples. Your actual costs will vary based on your specific plan details.
What to Do if Your Plan Doesn’t Cover the Full Cost
If you’re facing a balance after insurance, you have several options. Many treatment centers and organizations have created pathways to make care more accessible.
- Payment plans: Most facilities will work with you to set up manageable monthly payments.
- Sliding-scale fees: Some centers adjust costs based on your income.
- Rehab scholarships and grants: Organizations like SAMHSA and non-profits offer financial aid that you don’t have to repay.
- Personal loans or crowdfunding: These are other options to cover remaining costs.
- State-funded programs: Your state may offer low-cost or free treatment programs for eligible residents.
Our team at Addiction Helpline America can help you explore all these financial avenues. We work with centers that offer flexible payment solutions and can connect you with a facility that fits your clinical needs and your budget.
Frequently Asked Questions about UHC Rehab Coverage
Here are concise answers to the most common questions about UnitedHealthcare Insurance Coverage for Drug and Alcohol Rehab.
How long will UnitedHealthcare cover addiction treatment?
The length of coverage depends on medical necessity, not a fixed number of days. Clinicians use criteria from the American Society of Addiction Medicine (ASAM) to determine the appropriate level and duration of care. While many 30, 60, or 90-day programs are covered, your treatment team can request extensions if longer care is clinically justified. UnitedHealthcare supports a continuum of care, meaning coverage can adapt as you transition from inpatient to outpatient settings.
Do I need a referral or pre-authorization for rehab with UnitedHealthcare?
It depends on your plan.
- HMO plans almost always require a referral from your primary care physician (PCP).
- PPO plans typically do not require referrals, giving you more freedom to choose.
Regarding pre-authorization (or pre-certification), UnitedHealthcare often requires it for services like medical detox and inpatient stays to confirm medical necessity. While not always mandatory for all services, it’s a critical step to prevent coverage denials. In an emergency, you can get care first and notify UHC as soon as possible. Always check your specific plan’s requirements before starting treatment.
Does UnitedHealthcare cover treatment for co-occurring disorders?
Yes, absolutely. UnitedHealthcare provides coverage for co-occurring disorders (also called dual diagnosis), where a person has both a substance use disorder and a mental health condition like depression or anxiety. Federal parity laws (MHPAEA) require that mental and behavioral health services be covered to the same extent as medical services. UHC supports integrated treatment programs that address both conditions simultaneously, which is the most effective approach for lasting recovery.
Take the First Step Towards Recovery Today
Seeking answers is a courageous first step. While navigating insurance can feel complex, understanding your UnitedHealthcare Insurance Coverage for Drug and Alcohol Rehab is the key to open uping life-changing treatment.
Recovery is possible. UnitedHealthcare provides robust coverage for the full continuum of care, from detox to long-term therapy. You have access to a vast network of providers and a dedicated, 24/7 Substance Use Helpline at 1-855-780-5955 for confidential support.
But you don’t have to figure this out alone. At Addiction Helpline America, our recovery advocates specialize in working with UnitedHealthcare plans. We provide free, confidential guidance to help you:
- Verify your specific benefits.
- Understand your out-of-pocket costs.
- Find a quality, in-network treatment center that fits your needs.
We take the burden of insurance navigation off your shoulders so you can focus on getting well. The path to a healthier life starts with asking for help. Verify your UnitedHealthcare rehab insurance coverage with our complete guide or call our team today. We’re ready to help you begin your journey.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.












