What You Need to Know About Opiate Detox Programs
Opiate detox programs are medically supervised treatment services designed to help individuals safely stop using opioids while managing withdrawal symptoms. These programs provide medications, monitoring, and support during the critical first days of recovery.
Quick Overview of Opiate Detox Programs:
- What they are: Medically supervised withdrawal from opioids with symptom management
- Where they happen: Inpatient facilities (24-hour care) or outpatient settings (office visits)
- How long: 5-7 days for short-acting opioids, 14+ days for long-acting opioids
- What they provide: Medications (buprenorphine, methadone, clonidine), medical monitoring, counseling
- Cost: Many programs accept insurance, Medicare/Medicaid, or offer sliding scale fees
- What comes next: Transition to long-term treatment (medication-assisted treatment, therapy, support groups)
The opioid crisis in America continues to worsen. In the year leading up to December 2020, more than 92,000 people died from overdose – a nearly 30% increase from the previous year. Behind these numbers are individuals and families searching for a way out of opioid dependence. In 2010 alone, an estimated 12 million people abused prescription pain relievers, and over 600,000 abused heroin, highlighting the pervasive nature of this challenge.
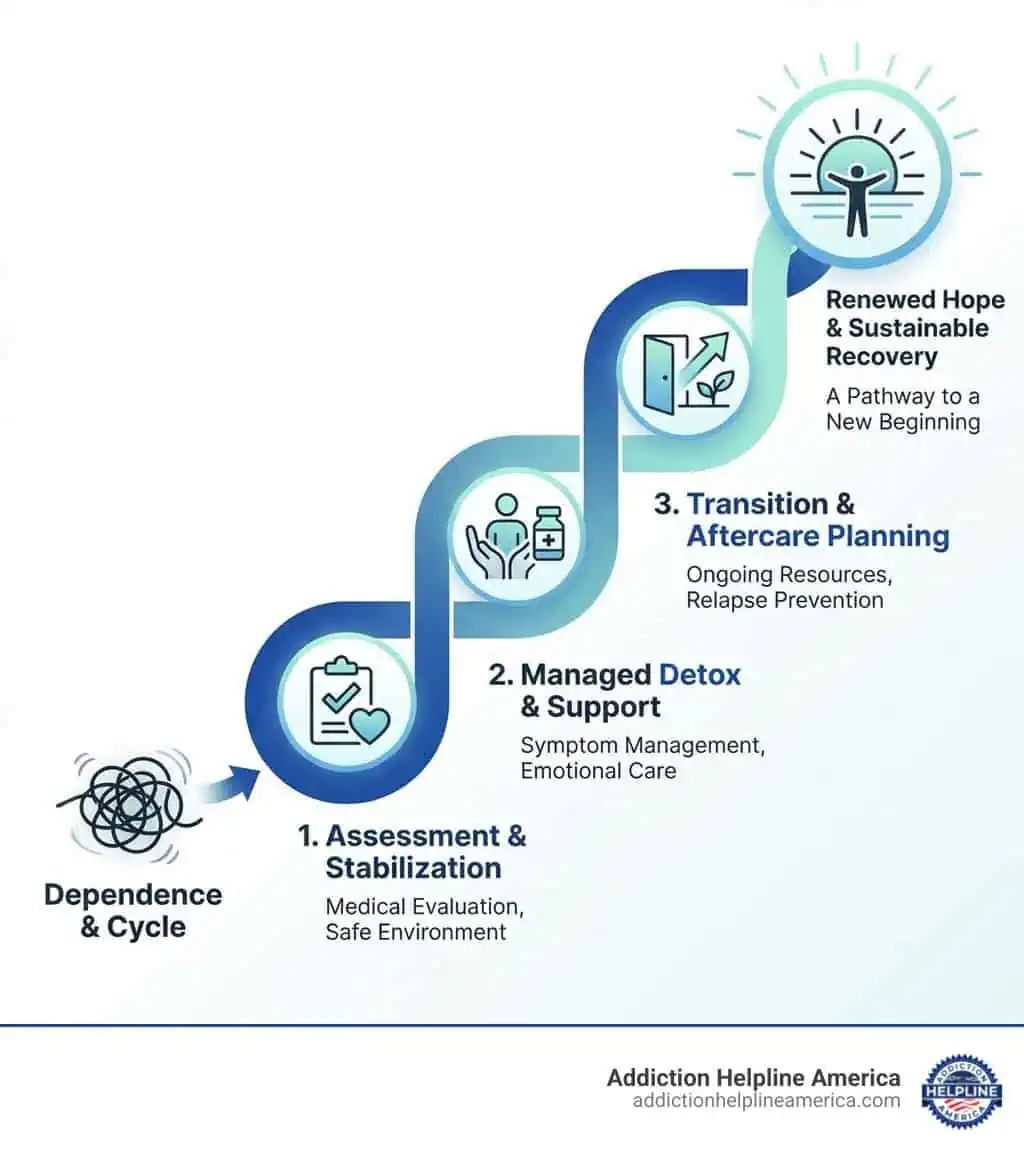
Opiate detox is the medically supervised process of helping someone safely stop using opioids while managing withdrawal symptoms. It’s often the first step toward recovery, though detox alone is rarely enough. While withdrawal symptoms can be extremely uncomfortable – including muscle aches, nausea, anxiety, and intense cravings – they are not typically life-threatening when managed properly.
However, attempting detox without medical help carries serious risks. Dehydration, complications from pre-existing conditions, and a dramatically increased risk of fatal overdose after relapse make supervised detox programs essential for safety.
At Addiction Helpline America, we provide free and confidential guidance to individuals and families seeking help with addiction. Our team has extensive experience connecting people to effective opiate detox programs that offer the medical support and compassionate care needed for a successful start to recovery.
The Opiate Withdrawal Experience: Symptoms and Timeline
Understanding the experience of opioid withdrawal is crucial for anyone considering or entering an opiate detox program. It’s important to differentiate between physical dependence and addiction. Physical dependence occurs when the body adapts to the presence of opioids, leading to withdrawal symptoms if use stops. Addiction, or opioid use disorder (OUD), is a chronic brain disease characterized by compulsive drug-seeking and use despite harmful consequences. You can learn more about this complex process in our Drug Withdrawal Complete Guide.
Withdrawal symptoms arise because the body has built a physical dependence on opioids. When the substance is no longer present or its dose is significantly reduced, the body struggles to adapt to its absence. While the experience is undeniably unpleasant and often intense, opioid withdrawal symptoms are generally not life-threatening on their own. In fact, opioid withdrawal is typically less medically dangerous than withdrawal from substances like sedative-hypnotics or alcohol.
However, this doesn’t mean it’s safe to attempt detox without medical supervision. Unsupervised detox carries significant dangers. Complications from pre-existing medical conditions, or issues related to injection drug use, can become life-threatening. Dehydration from severe vomiting and diarrhea, and even heart failure, are potential risks if withdrawal is untreated. Furthermore, one of the most perilous aspects of attempting to detox at home is the dramatically increased risk of overdose if a relapse occurs after a period of abstinence. Without medical oversight, detoxing without a clear motivation for abstinence or a follow-up plan significantly increases a patient’s risk for overdose and death.
Common Opiate Withdrawal Symptoms
Opioid withdrawal symptoms can range from mild to severe, often feeling like a terrible case of the flu. Most people experiencing opioid withdrawal will begin to feel symptoms within the first 8-24 hours after their last dose, sometimes even sooner.
Common symptoms include:
- Intense drug cravings
- Anxiety, agitation, restlessness
- Muscle and bone pain, muscle spasms
- Nausea and vomiting, abdominal cramps, stomach aches
- Diarrhea, gastrointestinal distress
- Insomnia and other sleep disturbances
- Increased body temperature, sweating, chills, diaphoresis
- Racing heart (tachycardia) and fluctuating blood pressure
- Runny nose and watery eyes
- Constricted pupils
- Tremors
Beyond the acute physical symptoms, individuals may also experience psychological distress. This can lead to a condition known as Post-Acute Withdrawal Syndrome (PAWS). PAWS can last up to a year or even longer after the acute withdrawal phase. Symptoms of PAWS are primarily psychological and can include:
- Mood swings, irritability, and anxiety
- Depression and anhedonia (inability to feel pleasure)
- Cravings (which can be intense)
- Fatigue and low energy
- Poor concentration and memory issues
- Sleep disturbances
- Abnormal stress reactivity
These protracted symptoms can make individuals vulnerable to relapse, emphasizing why detox is just the first step in a longer recovery journey.
The Opiate Withdrawal Timeline
The timeline for opiate withdrawal symptoms is highly variable and depends on several factors, including:
- Type of opioid: Short-acting vs. long-acting.
- Duration of use: How long the individual has been using.
- Dosage: The typical amount of opioid used.
- Frequency and method of use: How often and how the opioid was administered.
- Individual physiology: Metabolism, overall health, and co-occurring conditions.
Here’s a general overview of typical withdrawal timelines:
| Opioid Type | Onset of Symptoms | Peak Symptoms | Duration of Acute Withdrawal |
|---|---|---|---|
| Short-Acting Opioids | 8-12 hours after last use | 1-3 days | Up to 7 days (or 10 days) |
| (e.g., Heroin) | |||
| Long-Acting Opioids | Up to 36 hours after last use | Day 3-4 | Up to 14 days or more |
| (e.g., Methadone, Oxycodone, Fentanyl) |
For short-acting opioids like heroin, symptoms typically begin within 8-12 hours of the last dose, peak around 1-3 days, and generally subside within 7 days.
For long-acting opioids such as methadone, oxycodone, hydrocodone, and fentanyl, the first withdrawal symptoms may appear up to 36 hours after the last use. These symptoms tend to peak around day 3 or 4 and can continue for 14 days or more. Methadone withdrawal, for example, can typically last 10-20 days. Synthetic opioids like Suboxone, if misused, can also lead to prolonged withdrawal lasting two weeks or longer.
Following the acute withdrawal phase, the protracted withdrawal period (PAWS) can last up to 6 months to a year or longer, characterized by psychological symptoms.
Exploring Different Types of Opiate Detox Programs
When facing opioid withdrawal, remember that individualized treatment plans are crucial for success. What works for one person may not work for another. Medically managed withdrawal is consistently recommended for both safety and comfort, providing significant benefits over attempting to detox at home. Our comprehensive Detox Programs guide offers more insights into various options.
Inpatient vs. Outpatient Detox Settings
The setting for your opiate detox program will depend on the severity of your dependence, your overall health, and your support system.
-
Inpatient Detox: This involves hospitalization or 24-hour medical care in a residential setting. It’s generally the preferred setting for opioid detoxification, especially for individuals with severe dependence, those dependent on multiple drugs, or those with complicated medical issues. In an inpatient setting, you receive around-the-clock medical monitoring, medication management, and a supportive environment free from external triggers. This ensures your safety and comfort during the most intense phases of withdrawal.
-
Outpatient Detox: This type of program allows you to live at home while attending regular visits to a clinic or treatment center. Outpatient detox can be suitable for individuals with less severe opioid dependence, a strong support system at home, and good overall health. These programs often include office-based treatment, medication management, and counseling sessions. Partial Hospitalization Programs (PHPs) are another form of intensive outpatient care that offers structured treatment for several hours a day, multiple days a week, allowing patients to return home in the evenings.
Medical Detox vs. Rapid Detox: A Safety and Efficacy Comparison
When exploring opiate detox programs, you might come across terms like “medical detox” and “rapid detox.” It’s critical to understand the significant differences between these approaches, particularly concerning safety and efficacy.
-
Medical Detox: This is the standard, evidence-based approach to opioid withdrawal. In a medical detox program, you undergo withdrawal under the supervision of medical professionals. The process is gradual, focusing on managing symptoms with appropriate medications to ensure safety and comfort. Enrolling in a medical detox program is considered the safest way to go through detox, offering many supports and medications to make the process more comfortable.
-
Rapid Detox: Rapid and ultra-rapid detox methods involve using varying levels of sedation or anesthesia while administering an opioid antagonist (like naloxone, naltrexone, or nalmefene). The theory is that this forces the body to detox more quickly by rapidly clearing opioids from receptors. While rapid detox may clear the drug from the body in a day or two, compared to a week or more for medical detox, studies do not show it to be any more effective than traditional detox methods.
The risks associated with rapid detox are substantial and often outweigh any perceived benefits:
- Safety Concerns: Rapid detox is not necessarily safe and can put a person at risk for several dangerous and avoidable conditions. Adverse side effects can include severe vomiting or diarrhea, low blood pressure, delirium, aspiration pneumonia, pulmonary edema, diabetic ketoacidosis, and in rare cases, sudden death. These severe withdrawal symptoms require close medical supervision and can be life-threatening.
- High Cost and Lack of Insurance Coverage: Rapid detox is often not covered by insurance and can be extremely expensive, ranging from $13,000-$15,000 out of pocket, with some centers charging upwards of $21,000+. This makes it inaccessible for many and financially burdensome for others.
Due to the significant risks and questionable efficacy compared to medically supervised detox, medical detox is almost universally considered the safer and more recommended choice for most individuals seeking an opiate detox program.
The Role of Medication and Therapy in Detox
A successful opiate detox program is always part of a comprehensive treatment plan that addresses not only the physical dependence but also the psychological, emotional, and social factors contributing to opioid use disorder. This includes addressing root causes and managing co-occurring mental health disorders, a common challenge for individuals with OUD. For more in-depth information on comprehensive care, refer to our Opioid Addiction Treatment Options guide.
Research indicates a higher risk of non-medical prescription opioid use among individuals with mental, personality, and substance use disorders. Therefore, individualized treatment plans must consider these co-occurring conditions, providing integrated care that treats both the substance use disorder and the mental health disorder simultaneously.
Medications Used to Manage Withdrawal
Medications play a vital role in managing withdrawal symptoms, reducing cravings, and easing the discomfort associated with detox. These medications are administered under medical supervision to ensure safety and efficacy.
- Buprenorphine (often combined with naloxone as Suboxone): This medication is a partial opioid agonist, meaning it activates opioid receptors to a lesser degree than full agonists like heroin or oxycodone. It helps alleviate withdrawal symptoms and control cravings without producing a euphoric high. Studies show that when patients receive buprenorphine instead of clonidine for opioid withdrawal, they are significantly more likely to succeed. For instance, in one study, 77% of inpatients assigned to buprenorphine completed a 13-day taper program, compared to a much lower rate for clonidine.
- Methadone: A full opioid agonist, methadone is often used to manage severe opioid withdrawal symptoms, particularly from heroin, and supports long-term recovery by stabilizing individuals. It prevents withdrawal symptoms and reduces cravings.
- Clonidine: An alpha-2 adrenergic agonist, clonidine is used off-label to help reduce many physical symptoms of opioid withdrawal, such as anxiety, muscle aches, sweating, and high blood pressure. While effective for symptom management, buprenorphine has shown higher success rates in full detox completion.
- Naltrexone: This is an opioid antagonist that blocks opioid receptors, preventing opioids from having an effect. It is typically used after detox is complete to prevent relapse and reduce cravings, as it can precipitate severe withdrawal if opioids are still in the system.
- Ancillary Medications: In addition to the primary medications, other medications may be used to manage specific withdrawal symptoms. These can include over-the-counter medications like loperamide (for diarrhea), meclizine or dimenhydrinate (for nausea/vomiting), acetaminophen or NSAIDs (for pain/headaches), and antihistamines (for sleep). Antidepressants or benzodiazepines may also be prescribed for anxiety or panic attacks, especially in cases of co-occurring mental health disorders.
The Importance of Medication-Assisted Treatment (MAT) and Therapy
Medication-Assisted Treatment (MAT) is an evidence-based approach that combines medications with counseling and behavioral therapies. It is crucial for long-term recovery and is highly recommended as part of a broader treatment plan. The principal purpose of supervised withdrawal is often to safely and successfully transition the patient to medication for opioid use disorder.
The reality is that detox alone is rarely sufficient for lasting abstinence. Studies have shown that people who complete a detox soon after stopping illicit opioids have a very high chance of returning to opioid use – in some studies, more than 90% of individuals who completed detoxification returned to opioid use within a few months. This highlights that supervised withdrawal alone does not generally result in sustained abstinence from opioids, nor does it address the underlying reasons for dependence or the damage addiction has caused to relationships, employment, finances, and overall well-being. Few patients can remain abstinent without continued treatment with medications immediately after detox.
Behavioral therapies are essential components of MAT, helping individuals address the root causes of their addiction and develop coping skills for a sober life. These include:
- Cognitive Behavioral Therapy (CBT): Helps individuals identify and change negative thought patterns and behaviors related to drug use.
- Contingency Management: Provides incentives for positive behaviors, such as negative drug tests.
- Family Behavior Therapy: Involves family members in the treatment process to improve communication and support.
Support groups, such as 12-step programs, also provide invaluable peer support and a sense of community, which are critical for sustained recovery. Our Heroin Treatment Programs Guide offers further details on comprehensive treatment approaches.
Life After Detox: Finding a Program and Building Long-Term Recovery
It’s vital to understand that detox is merely the first stage of opioid addiction treatment. While it addresses physical dependence, it doesn’t cure addiction, which is a chronic, manageable condition. Continued care is crucial for rebuilding health, avoiding relapse, and achieving broader life goals. We believe that addiction is not cured but can be managed, enabling people to live fulfilling lives without substances.
The long-term recovery prospects are significantly improved with ongoing treatment. However, relapse can be a part of the recovery journey, and it’s important not to view it as a failure. Relapse can be particularly dangerous after a period of abstinence due to a loss of tolerance, increasing the risk of overdose. Detoxification may even be needed more than once in a person’s treatment course due to the high risk of relapse.
How to Find and Choose Suitable Opiate Detox Programs
Finding the right opiate detox program is a critical step. We provide free and confidential guidance to connect you with suitable treatment options.
Here are factors to consider when choosing a program:
- Individual Needs: Treatment plans should be custom to your specific needs, considering your history of opioid use, overall health, and any co-occurring mental health disorders.
- Accreditations and Staff Credentials: Ensure the facility is accredited and employs licensed, experienced medical and clinical staff.
- Treatment Philosophy: Look for programs that align with evidence-based practices, including the use of Medication-Assisted Treatment (MAT) and comprehensive therapies. Avoid programs that discourage or do not offer MAT after detoxification.
- Cost and Insurance Coverage: The cost of opiate detox programs can vary. Many programs offer services on a sliding scale based on income. Health insurance, including Medicare and Medicaid, can often be applied. The Affordable Care Act of 2010 mandated comparable insurance coverage for mental health and substance use disorder claims, which can help cover costs. It’s always best to check with your insurance provider to understand your benefits.
We can help you steer these considerations and find a suitable opiate detox program. You can find a treatment facility with our complete guide.
Your Rights and Long-Term Support
It’s important to know your rights when seeking care for substance use disorders. Hospitals are legally responsible for providing effective care to people with substance use disorder. Federal laws such as the Emergency Medical Treatment and Labor Act (EMTALA), the Americans with Disabilities Act (ADA), and Title VI of the Civil Rights Act apply to hospitals providing care for substance use disorders. This means hospitals cannot deny appropriate medical screening and stabilizing treatment, discriminate based on a substance use disorder, or treat patients differently based on race. Hospitals have legal obligations to treat addiction and provide evidence-based care.
Long-term support systems are crucial for maintaining recovery after detox. These can include:
- Family Therapy: Involving loved ones in the recovery process can strengthen support networks and improve communication.
- 12-Step Programs: Groups like Alcoholics Anonymous (AA) and Narcotics Anonymous (NA) provide peer support, shared experiences, and a structured path to recovery. You can find an AA meeting or find an NA meeting near you.
- Ongoing Counseling and Therapy: Continued individual or group therapy helps address underlying issues, develop coping mechanisms, and prevent relapse.
- Sober Living Environments: These provide structured, supportive housing for individuals transitioning from inpatient treatment back into independent living.
Building a sober life is a continuous journey that benefits immensely from a robust support system and ongoing commitment to recovery.
Frequently Asked Questions about Opiate Detox
Is opiate withdrawal life-threatening?
While extremely uncomfortable, opioid withdrawal symptoms are generally not life-threatening on their own. However, complications from pre-existing medical conditions (like heart conditions or diabetes) or health issues related to injection drug use can make it dangerous. Risks like severe dehydration (from vomiting and diarrhea) and heart failure are potential dangers if withdrawal is untreated or unsupervised. This is why medical supervision during detox is so important.
How long does opiate detox last?
The duration of opiate detox programs varies significantly based on the type of opioid used, the length and intensity of use, and individual factors.
- For short-acting opioids (like heroin), acute withdrawal typically lasts 5-7 days.
- For long-acting opioids (like methadone or oxycodone), the acute phase can extend to 14 days or more.
Beyond the acute physical symptoms, Post-Acute Withdrawal Syndrome (PAWS) can cause psychological symptoms that last for several months, sometimes even a year or longer.
What is the success rate of opiate detox programs?
It’s important to clarify what “success” means in this context. Detox alone is not a measure of long-term recovery or sustained abstinence. In fact, studies show a very high chance of relapse for those who only complete detox without follow-up care. In some research, over 90% of people who completed detoxification returned to opioid use over the next few months.
The true success of an opiate detox program depends on its ability to transition individuals into long-term treatment and sustained recovery. When detox is followed by Medication-Assisted Treatment (MAT) and comprehensive therapy, outcomes significantly improve. For example, patients receiving buprenorphine during withdrawal are more likely to successfully complete detox and engage in further treatment. Detox serves as a crucial first step, but it must be integrated into a broader, ongoing treatment plan for lasting success.
Take the Next Step on Your Recovery Journey
Understanding opiate detox programs is the first critical step toward freedom from opioid dependence. We’ve explored the uncomfortable but manageable symptoms of withdrawal, the varying timelines based on opioid type, and the crucial differences between medical and rapid detox. We’ve also emphasized the indispensable role of medication-assisted treatment and comprehensive therapy in achieving long-term recovery.
While detox can be challenging, it is a manageable process with the right medical help and support. Hope for recovery is not just a possibility; it’s a reality for millions.
If you or a loved one is struggling with opioid dependence, know that you don’t have to face it alone. Addiction Helpline America is here to provide free, confidential, and personalized guidance to help you find the right recovery program from our vast network of treatment centers. We are dedicated to connecting individuals nationwide to the resources they need to begin their journey toward a healthier, substance-free life.
Take that brave next step. Reach out today.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.














