
Choosing to seek help for addiction is a monumental first step, but it often leads to a crucial question: what kind of help is right for you? The world of addiction treatment is vast, with numerous therapeutic approaches designed to address the complex nature of substance use disorders. Understanding the different types of addiction therapy is essential for finding a path that aligns with your personal needs, beliefs, and circumstances.
This isn’t a one-size-fits-all journey; successful recovery depends on finding the specific tools that work for you. This guide provides an in-depth look at the most effective and evidence-based therapies available today. We will explore the core principles, practical applications, and ideal use cases for a range of methods, from structured, skills-based approaches like CBT to supportive, peer-led models.
This detailed overview is designed to empower you with the knowledge needed to make a confident and informed decision for yourself or a loved one. By exploring these options, you can better identify a treatment style that resonates with your goals and start building a solid foundation for lasting recovery.
1. Cognitive Behavioral Therapy (CBT)
Cognitive Behavioral Therapy (CBT) is a cornerstone among the different types of addiction therapy, renowned for its structured, goal-oriented approach. Developed by Dr. Aaron Beck, this psychotherapy operates on the fundamental principle that our thoughts, feelings, and behaviors are interconnected. For addiction, CBT helps individuals identify and dismantle the automatic negative thought patterns and learned behaviors that fuel substance use.
The process is practical and hands-on. A therapist works with the client to recognize specific triggers, such as social anxiety or stress, that lead to cravings. From there, they collaboratively develop healthier, more effective coping strategies.
How CBT Works in Practice
CBT is not about endlessly discussing the past; it’s about building skills for the future. The goal is to equip individuals with the tools to become their own therapists.
- Functional Analysis: Clients learn to dissect the “before” and “after” of substance use, identifying high-risk situations and the consequences of their actions.
- Skills Training: Therapists teach concrete techniques like stress management, problem-solving, and assertive communication to handle triggers without resorting to substances.
For example, a person might use a “thought record” to log a craving, the thought that accompanied it (“I can’t handle this meeting without a drink”), and then work to challenge and reframe that thought (“This is just anxiety. I have practiced my talking points and can manage this”). This method is successfully integrated into programs like the Matrix Model for methamphetamine addiction and is a core component of treatment at facilities like the Betty Ford Center.
This infographic provides a quick reference for the typical structure and outcomes of CBT in an addiction treatment setting.
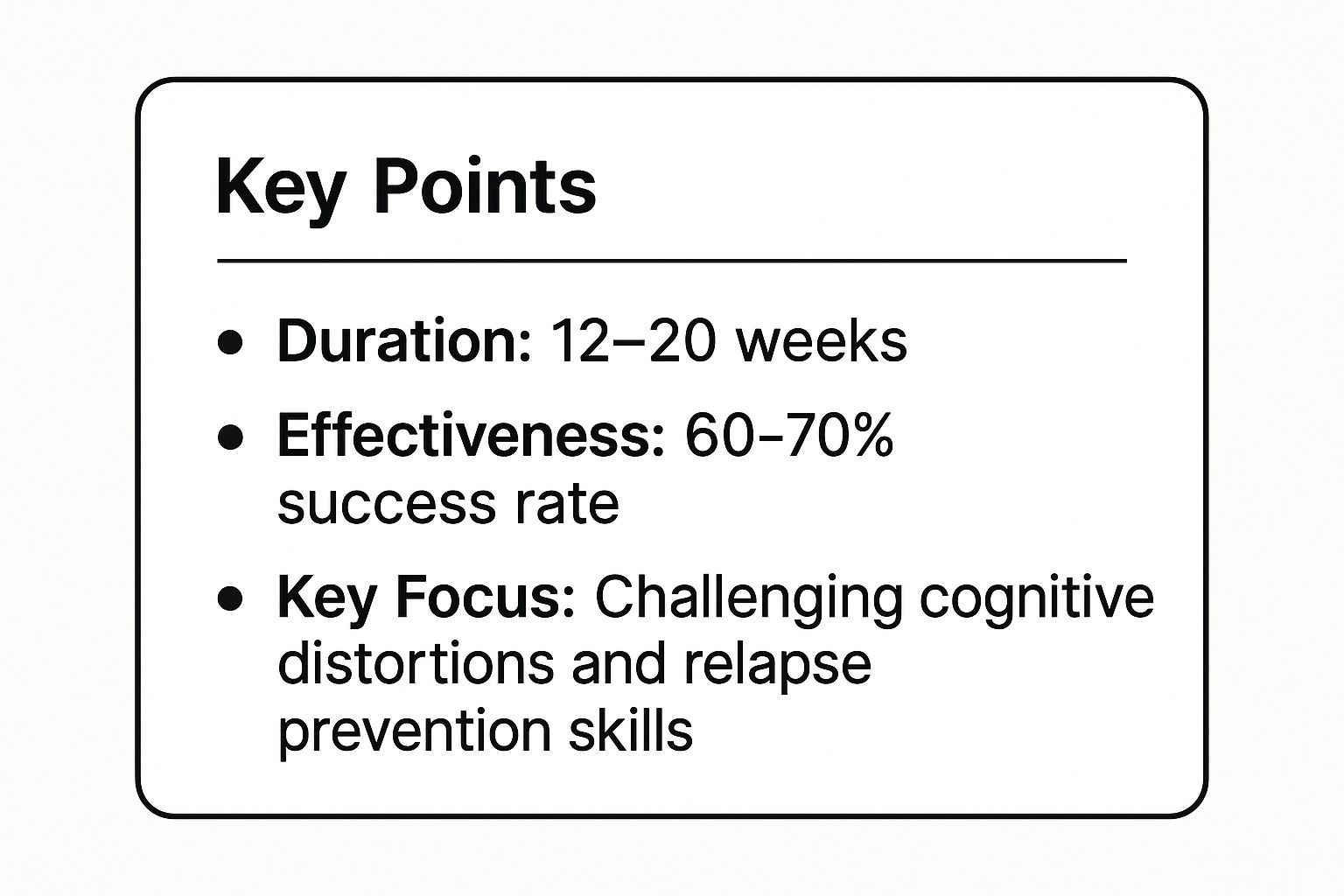
The data highlights that CBT is a time-limited, effective intervention focused on tangible skills for relapse prevention. For a more detailed exploration of its role in recovery, you can learn more about therapy in addiction recovery.
2. 12-Step Programs
Among the most widely recognized types of addiction therapy, 12-Step programs provide a peer-led, spiritual framework for recovery. Originating with Alcoholics Anonymous (AA) co-founders Bill Wilson and Dr. Bob Smith, this approach is built on a sequence of twelve guiding steps. The core principle involves admitting powerlessness over addiction, seeking help from a higher power as one understands it, and committing to a lifelong process of spiritual and personal growth.
The model fosters a powerful sense of community and mutual support, where members share their experiences to help one another achieve and maintain sobriety. It is not professional therapy but a fellowship that complements clinical treatment.

How 12-Step Programs Work in Practice
The power of a 12-Step program lies in its structured, accessible, and community-driven process. The goal is to create a profound personal transformation that removes the obsession to use substances.
- Sponsorship: New members are encouraged to find a sponsor, an experienced member who has worked through the steps and can offer guidance and support.
- Regular Meetings: Consistency is key. Attending meetings provides a safe space to share struggles and successes, reinforcing the commitment to recovery.
For example, a newcomer might be advised to attend “90 meetings in 90 days” to build a strong foundation. They work through the steps with their sponsor, moving from self-examination in steps like making a “searching and fearless moral inventory” to making amends to those they have harmed. This model is the foundation for groups like Narcotics Anonymous (NA) and is a core part of the philosophy at renowned centers like Hazelden Betty Ford.
The peer-to-peer structure offers continuous, free support, which is vital for long-term relapse prevention. To understand how these principles extend to supporting families, you can explore more about 12-Step programs.
3. Motivational Interviewing (MI)
Motivational Interviewing (MI) is a collaborative, client-centered counseling style for strengthening a person’s own motivation and commitment to change. Developed by psychologists William Miller and Stephen Rollnick, MI operates on the principle that lasting change is more likely when an individual resolves their own ambivalence, rather than being told what to do. For addiction, this therapy is exceptionally effective for those who are uncertain or resistant to treatment.
The approach is guided and non-confrontational. A therapist uses specific communication techniques to evoke the client’s own reasons for wanting to overcome addiction, fostering a partnership where the client becomes the primary advocate for their recovery.
How MI Works in Practice
MI is about guiding a conversation to resolve internal conflict, not winning an argument. The goal is to build a person’s intrinsic desire to change by exploring their values and goals.
- Exploring Ambivalence: Therapists help clients voice their mixed feelings about substance use (“I know it’s hurting my health, but it’s how I connect with my friends”) without judgment.
- Eliciting Change Talk: The focus is on listening for and reinforcing any statements the client makes that favor change. This “change talk” is the key ingredient for building momentum.
For instance, a therapist might use the OARS technique (Open questions, Affirmations, Reflections, and Summaries) to steer the conversation. Instead of confronting a client’s resistance, the therapist “rolls with it,” acknowledging their perspective. This patient-first method is widely used for brief interventions in emergency departments and primary care and is often combined with other types of addiction therapy to prepare clients for more intensive work.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
4. Dialectical Behavior Therapy (DBT)
Dialectical Behavior Therapy (DBT) is a highly structured form of cognitive-behavioral treatment originally created by Dr. Marsha Linehan to treat borderline personality disorder. It has since proven remarkably effective for addiction, especially for individuals who also struggle with intense emotional dysregulation, self-harm, and chronic suicidal ideation. The core “dialectic” involves balancing acceptance of oneself as is, while simultaneously acknowledging the need for change.

For those battling addiction, DBT provides a framework to manage overwhelming emotions that often trigger substance use. It teaches that while pain is a part of life, suffering is optional, equipping clients with the skills to navigate distress without resorting to destructive behaviors.
How DBT Works in Practice
DBT is more than just talk therapy; it’s a comprehensive program built on four key skill modules. The goal is to build a life experienced as worth living.
- Skills Training Groups: Clients learn specific skills in mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness in a group setting.
- Individual Therapy: One-on-one sessions help clients apply these new skills to their specific life challenges and maintain motivation for recovery.
- Phone Coaching: Clients have access to their therapist for in-the-moment coaching to use DBT skills during real-world crises, preventing a lapse or relapse.
For instance, a person feeling an intense craving might use the “TIPP” distress tolerance skill: Temperature (splashing cold water on their face), Intense exercise, Paced breathing, and Paired muscle relaxation. This method is used in leading dual-diagnosis programs at facilities like McLean Hospital and has been adapted for adolescents with substance use disorders at Seattle Children’s Hospital. For more information from the source, visit the Behavioral Tech Institute, founded by Dr. Linehan.
5. Medication-Assisted Treatment (MAT)
Medication-Assisted Treatment (MAT) is a comprehensive, evidence-based approach among the different types of addiction therapy that integrates FDA-approved medications with counseling and behavioral therapies. This “whole-patient” method is primarily used for treating opioid, alcohol, and nicotine use disorders. MAT operates on the principle of treating addiction as a medical condition by stabilizing brain chemistry, blocking the euphoric effects of substances, and relieving physiological cravings.
This approach is highly effective in reducing withdrawal symptoms and lowering the risk of overdose, which allows individuals to engage more fully in the psychosocial aspects of their recovery. Pioneered by figures like Dr. Vincent Dole and Dr. Marie Nyswander and championed by organizations such as SAMHSA, MAT is a clinically proven standard of care.
How MAT Works in Practice
MAT is not about substituting one drug for another; it is a long-term strategy for managing a chronic brain disease. The goal is to create a foundation of stability from which a person can rebuild their life.
- Medication Management: Physicians prescribe medications like buprenorphine (Suboxone) to reduce opioid cravings, naltrexone (Vivitrol) to block the effects of opioids and alcohol, or methadone to stabilize individuals with severe opioid use disorder.
- Integrated Counseling: The medication component is always paired with therapy. This ensures individuals develop crucial coping skills, address underlying psychological issues, and build a strong support network for lasting recovery.
For example, a patient might receive a monthly injection of Vivitrol from their doctor while also attending weekly group therapy and individual counseling sessions. This dual approach, utilized by leading institutions like Johns Hopkins and Yale, addresses both the biological and behavioral dimensions of addiction. The data shows this combination significantly improves retention in treatment and reduces illicit drug use.
The key to success is understanding that medication provides the biological support needed to make therapeutic work possible. For an in-depth look at this modality, you can learn more about Medication-Assisted Treatment.
6. Contingency Management
Contingency Management (CM) is a highly effective behavioral therapy that uses positive reinforcement to help people sustain abstinence. Based on the principles of operant conditioning, this approach provides tangible rewards or incentives for verified evidence of positive behavioral change, such as a clean drug test. Pioneered by researchers like Stephen Higgins, CM operates on a simple yet powerful premise: reinforcing desired behaviors makes them more likely to be repeated.
The core of this therapy is a formal, structured system where clients earn prizes, vouchers, or privileges for meeting treatment goals. This method directly counteracts the immediate, powerful reinforcement of substance use by offering a competing, healthy alternative. It is one of the most effective types of addiction therapy for promoting initial abstinence and retaining clients in treatment, particularly for stimulants like cocaine and methamphetamine.
How Contingency Management Works in Practice
CM is less about talk therapy and more about action and reward. The focus is on creating a consistent, motivating environment where positive choices are immediately and transparently acknowledged.
- Objective Verification: Success is not based on self-report. Positive behaviors, like abstinence, are verified through objective means such as urinalysis.
- Systematic Reinforcement: When a client provides a negative drug screen, they receive a reward. This can involve drawing from a fishbowl for prizes of varying value, where the number of draws increases with consecutive negative tests.
For example, the VA has successfully implemented CM programs for veterans with substance use disorders, rewarding them for negative tests with vouchers for goods and services. Similarly, voucher-based reinforcement therapy, developed at the University of Vermont, has shown powerful results in treating cocaine addiction. The key is that the rewards are immediate and meaningful, creating a strong link between abstinence and positive outcomes.
7. SMART Recovery
SMART Recovery (Self-Management And Recovery Training) is a science-based, self-empowering addiction recovery support group. As one of the more modern types of addiction therapy, it moves away from spiritual models and instead uses motivational and cognitive-behavioral methods. The program is built on the principle that individuals have the power to take control of their addictive behaviors by learning and applying practical, evidence-based tools.
The core of SMART Recovery is its 4-Point Program®, which helps participants gain independence from addiction. It is not a 12-step program; it is secular, adapts as scientific knowledge evolves, and encourages individuals to eventually “graduate” and move on, although they are welcome to stay as long as they find it helpful.
How SMART Recovery Works in Practice
The program focuses on actionable strategies for the present and future rather than dwelling on the past. Participants learn to manage their thoughts, feelings, and actions in the “here and now.”
- Building Motivation: Individuals explore their own reasons for wanting to change, creating a personal cost-benefit analysis to strengthen their commitment to sobriety.
- Coping with Urges: The program teaches specific techniques to handle cravings when they arise, such as distraction, visualization, and urge surfing.
- Managing Thoughts, Feelings, and Behaviors: Using tools derived from CBT, like the “ABC” (Activating Event, Belief, Consequence) worksheet, members learn to dispute irrational beliefs that lead to substance use.
- Living a Balanced Life: The final point focuses on setting meaningful long-term goals and finding healthy, enjoyable activities to replace the role addiction played.
SMART Recovery meetings, both online and in-person across more than 25 countries, provide a supportive, non-judgmental environment to practice these skills. Leading facilities like Caron Treatment Centers often integrate its principles into their programs, and specialized support is available through SMART Recovery Family & Friends. To learn more, visit the official SMART Recovery website.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
8. Eye Movement Desensitization and Reprocessing (EMDR)
Eye Movement Desensitization and Reprocessing (EMDR) is a powerful psychotherapy that addresses the deep-seated trauma often fueling substance use disorders. Developed by Dr. Francine Shapiro, EMDR operates on the principle that addiction is frequently a symptom of unresolved, distressing life experiences. This therapy helps the brain reprocess these traumatic memories, reducing their emotional charge and, in turn, diminishing the compulsion to use substances as a coping mechanism.
The process involves recalling a disturbing memory while engaging in bilateral stimulation, most commonly guided eye movements. This dual focus helps the brain store the memory adaptively, moving it from a state of raw, present-day distress to a resolved past event.
How EMDR Works in Practice
EMDR is not talk therapy; it focuses on how the brain stores memories and the associated physical and emotional sensations. The goal is to neutralize the trauma that drives addictive behavior.
- Targeted Memory Processing: The therapist helps the client identify specific traumatic memories, negative self-beliefs (“I am worthless”), and associated cravings that act as addiction triggers.
- Bilateral Stimulation: While focusing on the target memory, the client follows the therapist’s hand or another stimulus with their eyes. This bilateral movement is believed to facilitate the brain’s natural information processing system, much like during REM sleep.
For example, a veteran with PTSD and alcohol addiction might use EMDR to process a specific combat memory. By reprocessing the event, the associated feelings of terror and helplessness are reduced, which in turn lessens the urge to drink to numb those emotions. This approach is central to trauma-informed care and is used effectively in Veterans Affairs hospitals and specialized facilities like The Meadows and Promises Treatment Centers.
9. Family Therapy and Systemic Approaches
Family Therapy and Systemic Approaches treat addiction not as an individual’s problem, but as a symptom of a larger family system. This form of therapy acknowledges that family dynamics, communication patterns, and unresolved conflicts can all fuel addictive behaviors. Pioneered by figures like Virginia Satir, it involves key family members in the recovery process to heal relationships and build a supportive home environment.
The core principle is that the family unit operates as an interconnected system; a change in one member affects the entire group. Therapists work to untangle codependency, address enabling behaviors, and restructure unhealthy family roles. This approach is crucial because a supportive family is one of the strongest predictors of long-term recovery.
How Family Therapy Works in Practice
The goal is to improve the functioning of the entire family, not just to “fix” the person with the addiction. It focuses on creating new, healthier patterns of interaction.
- Systemic Restructuring: A therapist helps the family identify and change dysfunctional communication and behavioral patterns. This might involve learning to express feelings constructively or setting firm, loving boundaries.
- Education and Skill-Building: Families learn about the disease of addiction, which reduces blame and stigma. They are taught practical skills through models like Community Reinforcement and Family Training (CRAFT), developed by Robert Meyers, to positively influence their loved one’s behavior.
For instance, a family might learn to stop making excuses for their loved one’s missed obligations and instead allow them to face the natural consequences, a key tenet of CRAFT. Another powerful model is Multidimensional Family Therapy (MDFT), which has proven highly effective for adolescent substance abuse by addressing issues across individual, family, and community contexts.
This approach transforms the family from a potential source of stress into a powerful network of support. For a deeper understanding of how these dynamics play out in treatment, you can learn more about family therapy in addiction recovery.
10. Mindfulness-Based Relapse Prevention (MBRP)
Mindfulness-Based Relapse Prevention (MBRP) is a modern approach among the types of addiction therapy that merges cognitive-behavioral strategies with mindfulness practices. Developed by researchers like Sarah Bowen and Alan Marlatt, it operates on the principle of increasing awareness of one’s own internal experiences, such as thoughts and cravings, without judgment or automatic reaction. For addiction, MBRP empowers individuals to observe these triggers as temporary events, giving them the space to choose a more skillful response than substance use.
The process is centered on cultivating a non-reactive, present-moment awareness. A therapist guides clients through meditation and mindfulness exercises to help them recognize and tolerate discomfort, effectively “riding the wave” of a craving until it subsides.
How MBRP Works in Practice
MBRP is not about stopping thoughts or cravings, but about changing one’s relationship to them. The objective is to build a “mental muscle” that allows for conscious response rather than impulsive reaction.
- Awareness Training: Clients practice mindfulness meditation to become more attuned to their thoughts, feelings, and bodily sensations as they arise in real-time. This helps in recognizing early warning signs of a potential relapse.
- Skillful Responding: Instead of automatically acting on a craving, individuals learn techniques like “urge surfing.” They mindfully observe the craving, noticing how it intensifies and eventually fades on its own, much like an ocean wave.
For example, a person might use a brief, guided meditation when feeling stressed, noticing the physical sensations of anxiety without reaching for a substance. This allows them to see that the feeling is transient. This method is used in programs developed at the Addictions Research Center at the University of Washington and is integrated into various treatment settings, including the community-based Recovery Dharma model.
The skills developed in MBRP are core to long-term recovery. For a deeper understanding of building these defenses against relapse, you can explore these relapse prevention tips.
Addiction Therapy Methods Comparison
| Approach | Implementation Complexity 🔄 | Resource Requirements ⚡ | Expected Outcomes 📊 | Ideal Use Cases 💡 | Key Advantages ⭐ |
|---|---|---|---|---|---|
| Cognitive Behavioral Therapy (CBT) | Moderate – structured sessions (12-20 weeks) | Requires trained therapists, client engagement | 60-70% success rates in clinical trials | Addiction with cognitive distortions, relapse prevention | Evidence-based, skills-focused, cost-effective |
| 12-Step Programs | Low – peer-led, no professional needed | Minimal resources, wide availability | Varies; decades of success stories | Individuals seeking peer support, spiritual recovery | Free, strong community support, accessible 24/7 |
| Motivational Interviewing (MI) | Moderate – requires therapist training (40+ hours) | Skilled counselors needed, adaptable | Improves engagement, reduces dropout | Resistant clients, pre-treatment engagement | Enhances motivation, respects autonomy |
| Dialectical Behavior Therapy (DBT) | High – combines individual, group therapy, coaching (6-12 months) | Specialized therapists, longer duration | Effective for dual diagnosis, reduces self-harm | Addiction with co-occurring emotional dysregulation | Comprehensive skills training, strong research backing |
| Medication-Assisted Treatment (MAT) | Moderate – medical supervision required | Access to FDA-approved meds, ongoing monitoring | 40-60% reduction in illicit use, overdose prevention | Opioid, alcohol, nicotine addictions | Reduces cravings, overdose risk, improves retention |
| Contingency Management | Moderate – time-limited rewards system | Cost for incentives, monitoring systems | 2-3x higher abstinence rates during treatment | Stimulant use disorders, treatment engagement | Rapid behavior change, combines well with other therapies |
| SMART Recovery | Low to Moderate – peer and facilitator-led | Requires motivated participants | Variable; science-based approach | Those seeking self-empowerment, secular options | Evidence-based, flexible, personal responsibility focus |
| Eye Movement Desensitization and Reprocessing (EMDR) | High – requires certified therapists, trauma focus | Specialized training and protocols | Rapid trauma processing, effective for PTSD-related addiction | Trauma-related addiction triggers | Strong trauma resolution, relatively fast results |
| Family Therapy and Systemic Approaches | Moderate to High – multiple participants, skilled therapists | Involves family members’ time and commitment | 64% success engaging resistant individuals (CRAFT) | Addiction influenced by family dynamics | Improves family support, addresses systemic issues |
| Mindfulness-Based Relapse Prevention (MBRP) | Moderate – 8-week structured group program | Trained facilitators, participant commitment | Reduces craving, increases acceptance | Managing stress, preventing relapse | Long-term coping skills, complements other therapies |
Finding Your Fit and Taking the Next Step
The journey through addiction recovery is not a one-size-fits-all process. As we have explored, the landscape of addiction treatment is rich and varied, offering a diverse toolkit to support individuals wherever they are in their path to healing. From the logical, skill-building framework of Cognitive Behavioral Therapy (CBT) to the profound community connection of 12-Step programs, and the vital medical stabilization offered by Medication-Assisted Treatment (MAT), each modality provides a unique and powerful lens through which to approach recovery.
The central takeaway is that empowerment comes from choice. Understanding the different types of addiction therapy allows you to become an active participant in your own recovery. You are no longer just a passive recipient of a pre-determined plan but a collaborator in building a strategy that resonates with your personal history, your psychological needs, and your life circumstances. Perhaps the structured, goal-oriented approach of SMART Recovery appeals to your sense of self-reliance, or maybe the trauma-informed care of EMDR is the key to unlocking underlying issues that fuel substance use.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Synthesizing Your Options for a Personalized Path
The most effective treatment plans are rarely built on a single therapeutic pillar. Instead, they often blend elements from several approaches to create a comprehensive, dynamic support system. For instance, a person might use MAT to manage cravings and withdrawal symptoms, attend CBT sessions to develop coping mechanisms for triggers, and participate in Family Therapy to heal relational dynamics.
This integration is where true, sustainable recovery is forged. It acknowledges that addiction is a complex condition with biological, psychological, and social components. Therefore, an effective response must be equally multifaceted. Don’t view these therapies as competing options but as complementary tools in your recovery arsenal.
Actionable Next Steps to Begin Your Journey
Feeling informed is the first step, but taking action is what transforms knowledge into progress. Here’s how you can move forward:
- Self-Assessment: Reflect on the descriptions of the therapies. Which ones resonated most with you? Consider your personality, past experiences with therapy, and whether you have a co-occurring condition like anxiety or PTSD that needs to be addressed.
- Professional Consultation: The most critical step is to consult with an addiction specialist, therapist, or treatment center. They can conduct a formal assessment to provide a clinical recommendation for which types of addiction therapy are best suited for your specific situation.
- Embrace Flexibility: Be prepared to be flexible. The therapy that works for you in the early stages of recovery might be different from what you need a year later. Recovery is an evolving process, and your treatment plan should evolve with you.
Ultimately, the goal is to find a path that not only helps you stop using substances but also builds a life that is meaningful, fulfilling, and resilient. The journey requires courage, but you do not have to walk it alone. Professional guidance can illuminate the way, ensuring you find the therapeutic fit that gives you the best foundation for lasting change and a healthier future.
Navigating the various types of addiction therapy can feel overwhelming, but expert help is available to guide you. The compassionate team at Addiction Helpline America can connect you with qualified treatment providers who will help you understand your options and find the right program for your needs. Take the definitive step toward recovery by reaching out to Addiction Helpline America today.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.















