Understanding the Path to Recovery
Lifelong management of treatment and schizophrenia requires a dedicated approach, but effective help is available. If you or a loved one has received a schizophrenia diagnosis, understanding your options is the first step toward recovery.
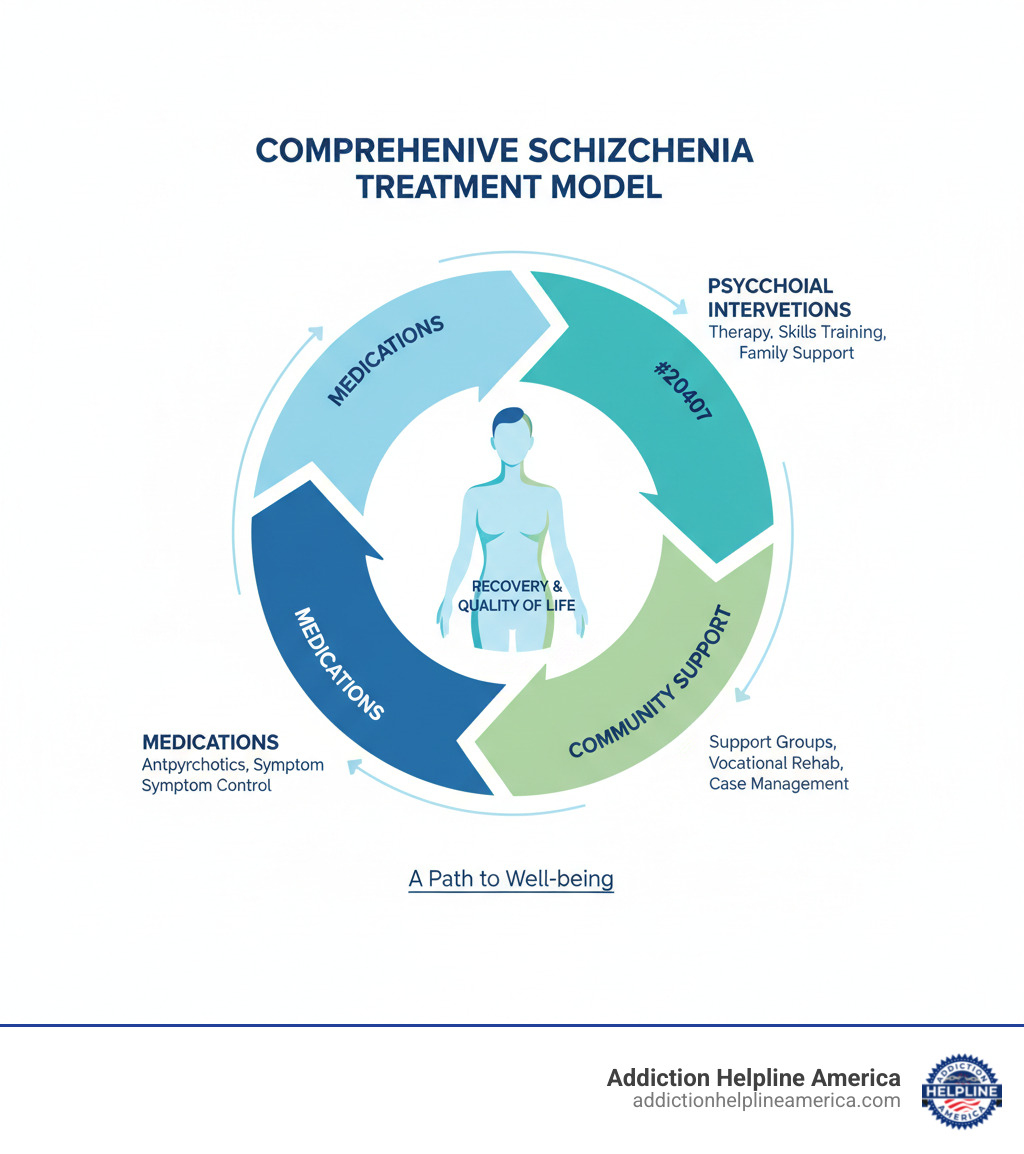
Quick Overview: Core Schizophrenia Treatments
- Antipsychotic Medications – First-line treatment targeting brain chemicals like dopamine and serotonin.
- Psychosocial Interventions – Therapy, skills training, and rehabilitation programs.
- Family Support & Education – Helping loved ones understand and assist in recovery.
- Community Resources – Support groups, vocational training, and case management.
Schizophrenia is a serious mental health disorder affecting how a person thinks, feels, and behaves, often causing symptoms like hallucinations and delusions. While there is no cure, research shows that at least 1 in 3 people with schizophrenia can fully recover from symptoms with the right care.
Treatment works. With a combination of medication, therapy, and strong support, many people with schizophrenia manage their symptoms and lead meaningful lives. Early and consistent treatment significantly improves long-term outcomes.
At Addiction Helpline America, we understand that schizophrenia often co-occurs with substance use disorders, making treatment and schizophrenia particularly complex. Our team connects individuals and families with comprehensive, integrated care that addresses both conditions. We’re here to help you find resources and support that can make a real difference.
Relevant articles related to treatment and schizophrenia:
The Cornerstone of Care: Medical Treatment and Schizophrenia
When it comes to treatment and schizophrenia, medication is the foundation of care. Antipsychotics help stabilize symptoms like hallucinations and delusions, making other forms of treatment possible. The goal is to manage symptoms at the lowest effective dose, helping you function better in daily life. Most people need medication for 1-2 years after a first episode, and often longer to prevent relapse.
Finding the right medication can take several weeks, but consistency is key.
Antipsychotic Medications: How They Work
Antipsychotics work by affecting neurotransmitters in the brain, primarily dopamine and serotonin. Imbalances in these chemicals contribute to schizophrenia symptoms. Most antipsychotics block dopamine D2 receptors to reduce positive symptoms like hallucinations. Newer medications also target serotonin receptors, which may help with negative and cognitive symptoms.
These medications don’t work overnight; it can take several weeks to see significant improvement. For more information, review scientific research on antipsychotic effectiveness.
First-Generation vs. Second-Generation Antipsychotics
Antipsychotics fall into two main categories:
| Feature | First-Generation (Typical) Antipsychotics | Second-Generation (Atypical) Antipsychotics |
|---|---|---|
| Efficacy | Effective for positive symptoms (hallucinations, delusions) | Effective for positive symptoms; may also help with negative and cognitive symptoms |
| Side Effect Profile | Higher risk of movement disorders (extrapyramidal symptoms, tardive dyskinesia) | Lower risk of movement disorders; higher risk of metabolic side effects (weight gain, diabetes, high cholesterol) |
| Examples | Haloperidol, Chlorpromazine, Fluphenazine | Risperidone, Olanzapine, Quetiapine, Aripiprazole, Clozapine |
First-generation antipsychotics are effective but carry a higher risk of movement side effects, including tremors, stiffness, and tardive dyskinesia (involuntary movements).
Second-generation antipsychotics have a lower risk of movement disorders but a higher risk of metabolic side effects like weight gain and increased blood sugar. These require regular monitoring.
Long-Acting Injectable (LAI) Antipsychotics
For those who find it hard to take daily pills, long-acting injectable (LAI) antipsychotics are an excellent option. These are administered by a healthcare provider every few weeks or months.
LAIs improve medication adherence, provide stable medication levels, and may lead to better symptom control and fewer hospitalizations. They are convenient for anyone who prefers less frequent dosing. For more information, visit the Royal College of Psychiatrists’ information on depot medication.
Managing Medication Side Effects and Other Medical Options
Side effects like weight gain, drowsiness, and movement disorders are common but often manageable. Your doctor can help by adjusting your dose, suggesting lifestyle changes, or switching medications. Report any side effects, especially involuntary movements, to your provider immediately.
In cases of treatment-resistant schizophrenia, your doctor might recommend Electroconvulsive Therapy (ECT), a safe and effective procedure for severe symptoms that haven’t responded to other treatments.
Hospitalization may be necessary during a crisis to ensure safety, stabilize symptoms, and adjust medication in a supervised environment.
At Addiction Helpline America, we know substance use can complicate medication management. Our team can connect you with integrated treatment programs that address both treatment and schizophrenia and addiction recovery simultaneously.
Understanding the Path to Recovery
When you or someone you love receives a schizophrenia diagnosis, it can feel overwhelming—but recovery is possible. Treatment and schizophrenia go hand in hand: with the right care, at least 1 in 3 people can fully recover from symptoms. Early, consistent treatment improves long-term outcomes.
Effective care typically combines several pillars: antipsychotic medications to reduce hallucinations and delusions; psychosocial interventions (such as therapy, skills training, and rehabilitation) to build coping strategies and daily functioning; family education and support to strengthen the home environment; and community resources like support groups, vocational training, and case management.
Many people manage symptoms and lead meaningful lives when these elements work together. At Addiction Helpline America, we recognize that schizophrenia often co-occurs with substance use. Our team connects individuals and families with comprehensive, integrated treatment that addresses both conditions.
If you’re looking for additional information, you might find these articles helpful: mental hospital near by me, drug for bipolar disorder, and can i refuse mental health treatment.
The Cornerstone of Care: Medical Treatment and Schizophrenia
When it comes to treatment and schizophrenia, medication is often the first and most critical step. Think of it as the foundation of a house—everything else builds upon it. Pharmacotherapy addresses the chemical imbalances in the brain that contribute to symptoms, and while there’s no cure for schizophrenia, lifelong treatment with medicines and psychosocial therapy can significantly help manage the condition.
Antipsychotic medicines are the most prescribed drugs for schizophrenia, and they play a vital role in controlling symptoms and preventing relapse. The primary goal with medication is to manage symptoms at the lowest effective dose, allowing individuals to function better in their daily lives—going to work, maintaining relationships, and enjoying activities that matter to them.
Finding the right medication and dose can take time, sometimes several weeks, as healthcare professionals often try different drugs to see what works best with the fewest side effects. This process requires patience. Most people will need to take medication for an extended period, often for 1 to 2 years after their first psychotic episode, and longer if the illness recurs, to prevent further acute episodes.
Antipsychotic Medications: How They Work
Antipsychotic medications are designed to help control the symptoms of schizophrenia by influencing key neurotransmitters in the brain. Neurotransmitters are chemical messengers that allow brain cells to communicate with each other—think of them as the brain’s postal service.
In schizophrenia, imbalances in these chemicals, particularly dopamine and serotonin, are thought to play a significant role in symptoms. Most antipsychotics primarily work by blocking dopamine D2 receptors. By reducing the activity of dopamine in certain brain pathways, these medications can alleviate positive symptoms such as hallucinations (seeing or hearing things that aren’t there) and delusions (strong beliefs not based in reality).
Newer medications, known as second-generation antipsychotics, also often target serotonin receptors. This broader action can sometimes help manage a wider range of symptoms, including some negative symptoms like lack of motivation or emotional flatness, and cognitive symptoms like difficulty concentrating.
These medications don’t offer an instant fix, and that’s important to understand. It can often take several weeks to see whether a particular medicine helps symptoms improve. During this time, consistent adherence to the prescribed regimen is vital. Antipsychotic medications are a key part of treating schizophrenia, and their effectiveness has been widely studied, as highlighted in scientific research on antipsychotic effectiveness.
First-Generation vs. Second-Generation Antipsychotics
When discussing treatment and schizophrenia, it’s important to differentiate between the two main categories of antipsychotic medications: first-generation (typical) and second-generation (atypical) antipsychotics. These groups differ in their chemical structure, how they affect brain chemicals, and their potential side effect profiles.
First-generation antipsychotics (FGAs), developed in the 1950s, primarily work by blocking dopamine D2 receptors. While effective at reducing positive symptoms, they are more commonly associated with extrapyramidal symptoms (EPS), which are movement-related side effects. These can include dystonia (involuntary muscle contractions), akathisia (a feeling of inner restlessness), pseudoparkinsonism (tremors and stiffness), and tardive dyskinesia (involuntary, repetitive body movements, especially of the face and tongue, which can sometimes be irreversible).
Second-generation antipsychotics (SGAs), developed in the 1990s, have a more complex mechanism of action. They block dopamine D2 receptors but also significantly affect serotonin receptors. This broader action often leads to fewer extrapyramidal symptoms and a lower risk of tardive dyskinesia compared to FGAs—a significant advantage. However, SGAs come with their own set of potential side effects, often metabolic in nature, such as weight gain (which can be substantial), increased risk of diabetes, and high cholesterol.
| Feature | First-Generation (Typical) Antipsychotics | Second-Generation (Atypical) Antipsychotics |
|---|---|---|
| Primary Mechanism | Strong dopamine D2 receptor blockade | Dopamine D2 receptor blockade + significant serotonin receptor modulation |
| Efficacy | Very effective for positive symptoms (hallucinations, delusions) | Effective for positive symptoms; may also help with negative and cognitive symptoms |
| Movement Side Effects | Higher risk of extrapyramidal symptoms (dystonia, akathisia, pseudoparkinsonism, tardive dyskinesia) | Lower risk of extrapyramidal symptoms |
| Metabolic Side Effects | Lower risk | Higher risk of weight gain, diabetes, and high cholesterol |
| Examples | Haloperidol, Chlorpromazine | Risperidone, Olanzapine, Quetiapine, Aripiprazole, Clozapine |
The choice between these two generations, or specific medications within them, depends on an individual’s unique symptom profile, response to previous treatments, and tolerability of side effects. There’s no one-size-fits-all approach.
Long-Acting Injectable (LAI) Antipsychotics
For many individuals living with schizophrenia, consistent medication adherence can be a significant challenge. This is where long-acting injectable (LAI) antipsychotics come into play. LAIs are formulations of antipsychotic medications that are administered via injection, typically into the muscle, and release the medicine slowly over an extended period.
These are not new medications, but rather different delivery methods for existing antipsychotics. Some antipsychotics may be given as a long-acting shot in the muscle or under the skin. LAIs are given by a healthcare professional, usually in a clinic setting, which eliminates the daily need for oral pills.
Depending on the specific medication, LAIs can be administered every 2 weeks, 3 weeks, or even once a month or every few months. This greatly simplifies the medication regimen and offers several benefits. Improved medication adherence is the primary advantage—by receiving an injection periodically, individuals don’t have to remember to take a pill every day, which can be particularly helpful for those who struggle with consistency or have anosognosia (lack of insight into their illness). This consistent medication level helps stabilize symptoms and significantly lowers the chance of psychotic episodes and hospitalizations. LAI antipsychotics have shown superiority over oral antipsychotics in preventing hospitalizations in real-world settings.
The steady release of medication ensures more consistent drug levels in the body, potentially leading to more stable symptom control. For some, taking daily pills can be a reminder of their illness, and LAIs offer more discretion and privacy.
LAIs are particularly beneficial for individuals who have a history of poor adherence to oral medications, prefer not to take daily pills, experience frequent relapses due to inconsistent medication use, or live in situations where medication management is challenging. Before starting an LAI, healthcare providers will often conduct a short trial with the oral counterpart of the medication to ensure it’s well-tolerated and effective. For more information on depot medication, which is another term for long-acting injectables, you can explore resources from the Royal College of Psychiatrists.
Managing Medication Side Effects and Other Medical Options
While antipsychotic medications are crucial for managing schizophrenia, they can come with potential side effects. Our healthcare team is dedicated to helping individuals manage these effects to ensure the best possible quality of life. Understanding and addressing side effects is a key part of effective treatment and schizophrenia management.
Common side effects include weight gain, particularly with many second-generation antipsychotics. Management involves regular monitoring, dietary changes, and increased physical activity. Drowsiness or sedation can be more pronounced when starting medication or with certain drugs—adjusting the timing of the dose (such as taking it at night) or reducing the dose can help.
Movement disorders, technically called extrapyramidal symptoms, are more common with first-generation antipsychotics but can occur with some second-generation drugs. These include tremors, stiffness, and restlessness. Management might involve switching medications, adjusting the dose, or prescribing other medications to counteract these effects. Tardive dyskinesia, a more persistent movement disorder, requires careful monitoring.
Metabolic side effects like increased blood sugar and cholesterol levels are concerns, especially with SGAs. Regular blood tests are essential to monitor these, and lifestyle changes or additional medications may be needed. Some antipsychotics can affect heart rhythm or cause a drop in blood pressure when standing up, requiring regular ECGs and counseling patients to rise slowly. Other side effects can include dry mouth, blurred vision, constipation, sexual dysfunction, and hormonal changes. Specific strategies exist for each, from hydration to medication adjustments.
Continuous monitoring for medication side effects is crucial. We work closely with individuals to choose medications that minimize unwanted effects and adjust treatment plans as needed.
When to consider Electroconvulsive Therapy (ECT): For adults with schizophrenia who don’t respond to drug therapy, or for those experiencing severe catatonia or suicidal ideation, electroconvulsive therapy (ECT) might be considered. ECT is a medical procedure performed under general anesthesia where small electric currents are passed through the brain, intentionally triggering a brief seizure. While it sounds intimidating, it can be highly effective in certain situations where other treatments have failed.
Sometimes, individuals don’t respond adequately to several trials of antipsychotic medications—this is known as treatment-resistant schizophrenia. In these cases, a specific second-generation antipsychotic called clozapine is often considered the most effective option. However, clozapine requires careful monitoring due to its unique side effect profile, including a risk of a serious blood condition called agranulocytosis.
Hospitalization may be necessary during crisis periods, when symptoms are acutely severe, or if an individual poses a danger to themselves or others. A hospital stay provides a safe, structured environment where medication can be stabilized, and basic needs like nutrition, sleep, and hygiene can be ensured. We’ll discuss hospitalization in more detail in the FAQ section.
Beyond Medication: The Role of Psychosocial Interventions
While medication is essential for treatment and schizophrenia, it’s not the whole story. Psychosocial interventions work alongside medication to help individuals manage symptoms, build life skills, and improve their overall quality of life. These therapies are custom to each person’s goals, whether it’s challenging distorted thoughts, improving social connections, or finding meaningful work. Together with medication, they create a comprehensive treatment plan that addresses the whole person.
Individual Therapy for Schizophrenia Treatment
Individual therapy offers a safe space to develop coping strategies. Several types are effective:
- Cognitive Behavioral Therapy for Psychosis (CBTp): This specialized approach teaches individuals to identify, challenge, and find healthier ways of interpreting distorted thoughts, delusions, and hallucinations. It helps reduce the distress associated with psychotic symptoms.
- Supportive Psychotherapy: This therapy focuses on building a trusting relationship with a therapist who provides emotional support, practical guidance, and help navigating daily stressors.
- Cognitive Improvement Therapy (CET): Also called cognitive remediation, CET uses computer-based exercises and group sessions to strengthen cognitive skills like attention, memory, and problem-solving.
For more information about mental health services and how they can support recovery, visit Addiction Information.
The Importance of Family and Social Support
Schizophrenia affects the entire family, making their involvement in treatment essential.
- Family Therapy and Psychoeducation: These services educate families about the illness, improve communication, and teach problem-solving skills. A supportive home environment is proven to reduce relapse rates.
- Social Skills Training (SST): SST helps individuals learn and practice communication skills and appropriate social behaviors, making it easier to build and maintain relationships.
- Peer Support Groups: Connecting with others who have similar experiences can be incredibly validating. These groups provide a safe space to share coping strategies and break the isolation that often accompanies mental illness.
Vocational Rehabilitation and Supported Employment
Having a purpose, like a job or volunteer work, is fundamental to recovery. Vocational rehabilitation and supported employment programs are designed to help people with schizophrenia find and keep jobs that match their abilities and interests.
These programs offer job coaching, resume preparation, and on-the-job support to ensure success. Building work-related skills and achieving financial independence boosts confidence and proves that schizophrenia does not define a person’s capabilities. Programs like Assertive Community Treatment (ACT) often integrate vocational support, providing a team of professionals to assist with all aspects of recovery.
Navigating Daily Life and Building a Support System
Living with schizophrenia means learning to manage a chronic condition, but many people lead fulfilling lives with the right strategies. Treatment and schizophrenia management is about creating a stable, supportive environment where recovery can flourish.
Essential Coping Strategies for Patients and Loved Ones
Managing schizophrenia is a team effort. These practical strategies can make a real difference:
- Educate Yourself: Understanding the illness reduces fear and helps you make informed decisions about care.
- Set Realistic Goals: Start with small, achievable targets to build confidence and momentum.
- Manage Stress: Regularly practice calming techniques like deep breathing, meditation, journaling, or gentle yoga.
- Prioritize Sleep: A consistent sleep routine is crucial, as poor sleep can worsen symptoms.
- Create a Routine: A predictable schedule for meals, medication, and activities provides stability.
- Partner with Your Treatment Team: Open communication with doctors and therapists ensures you get the best care.
- Use Social Services: Your care team can connect you with resources for housing, transportation, and other practical needs.
- Prepare for Appointments: Write down questions and symptoms beforehand. Consider bringing a trusted friend or family member for support. Explore more tips for staying on track.
Why Avoiding Alcohol and Drugs is Critical for Schizophrenia Treatment
Using alcohol or recreational drugs can derail schizophrenia treatment. While substances may seem to offer temporary relief, they make everything harder in the long run.
- They worsen psychotic symptoms. Substances like cannabis and stimulants can trigger or intensify hallucinations and delusions.
- They interfere with medication. Alcohol and drugs can prevent antipsychotics from working properly, leading to breakthrough symptoms or dangerous interactions.
- They increase the risk of relapse. Even one-time use can trigger a severe relapse, potentially requiring hospitalization.
At Addiction Helpline America, we know schizophrenia and substance use disorders often occur together (a dual diagnosis). This requires specialized, integrated care that addresses both conditions simultaneously. We can help you understand how to help someone with addiction and find free addiction treatment options.
Finding Strength in Community: Support Groups
No one should face schizophrenia alone. Support groups dissolve isolation and replace it with understanding, shared experiences, and hope.
Connecting with peers who truly understand is validating and empowering. These groups are a source of practical wisdom and non-judgmental emotional support. Family members and caregivers need support too. Organizations like the National Alliance on Mental Illness (NAMI) offer specific groups where families can share experiences, learn coping strategies, and find relief. These groups help families become more effective advocates for their loved ones.
We encourage anyone touched by schizophrenia to explore what’s available. You can learn more about joining a support community through NAMI. Building a strong support system is the foundation for recovery.
Frequently Asked Questions about Schizophrenia Treatment
Navigating treatment and schizophrenia brings up many questions. Here are answers to some of the most common ones we hear.
What are the primary goals of schizophrenia treatment?
The goals go beyond just symptoms to focus on the whole person:
- Reduce Symptoms: Alleviate distressing experiences like hallucinations, delusions, and disorganized thinking.
- Prevent Relapse: Maintain stability through consistent medication and therapy to avoid the return of severe symptoms.
- Improve Functioning: Help individuals rebuild relationships, develop social skills, and find meaningful work or education.
- Improve Quality of Life: Promote satisfaction, purpose, hope, and a sense of empowerment.
- Promote Independence: Support individuals in managing their daily lives and making their own choices.
What is the typical prognosis for individuals with schizophrenia?
The prognosis for schizophrenia is more hopeful than many believe. With comprehensive treatment and schizophrenia management, the outcomes are varied:
- Recovery is possible: Research shows at least 1 in 3 people can fully recover from symptoms with proper care.
- Early intervention is key: Diagnosing and treating schizophrenia promptly leads to better long-term outcomes and fewer hospitalizations.
- Consistent treatment matters: Sticking with medication and therapy significantly reduces relapse rates and allows people to build stable, meaningful lives.
While some individuals face persistent challenges and life expectancy can be reduced due to related health issues, recovery is a realistic goal. For more statistics, the National Institute of Mental Health offers comprehensive data.
Under what circumstances is a hospital stay necessary?
Most treatment occurs in the community, but a short-term hospital stay is sometimes the safest option. Hospitalization may be necessary for:
- Severe crisis periods: When psychotic symptoms become overwhelming and a person loses touch with reality.
- Danger to self or others: If someone is suicidal or their symptoms pose a risk to others, call or text 988 or 911 immediately. Safety is the top priority.
- Inability to care for basic needs: If a person cannot manage eating, sleeping, or hygiene.
- Medication stabilization: To safely start or adjust medications under close medical supervision.
- Diagnostic evaluation: To conduct a thorough assessment when symptoms are complex or unclear.
The goal of hospitalization is to stabilize the crisis and create a solid plan for returning to community-based care.
Conclusion
Schizophrenia is a lifelong condition, but we want you to remember this: with the right combination of treatment and schizophrenia management, recovery is not just possible—it’s a reality for many.
Comprehensive care is key. This includes antipsychotic medications to balance brain chemistry, psychosocial therapies like CBTp to rebuild life skills, and strong support systems to foster connection. Lasting stability is built on daily coping strategies, avoiding substances that derail progress, and consistent engagement with treatment.
Early intervention makes a real difference. The sooner someone receives care, the better their long-term outlook. When families get involved and create a supportive environment, quality of life improves dramatically.
At Addiction Helpline America, we know that schizophrenia often co-occurs with substance use disorders. Our team specializes in connecting people to integrated care that addresses both conditions together, because treating one without the other rarely works.
You don’t have to figure this out alone. Our team is here with free, confidential support to help you find the right treatment center, steer your options, or simply talk to someone who understands. No judgment, just real help.
Recovery looks different for everyone, but it is always worth pursuing. You deserve support, hope, and a path forward.
If you’re ready to take the next step, please reach out. Find professional help for schizophrenia and co-occurring disorders through Addiction Helpline America. We’re here to help.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.