Why Understanding Addiction Treatment for Specific Populations Matters
Addiction Treatment for Specific Populations recognizes that recovery is not one-size-fits-all. Different groups face unique challenges and needs when seeking help for substance use disorders.
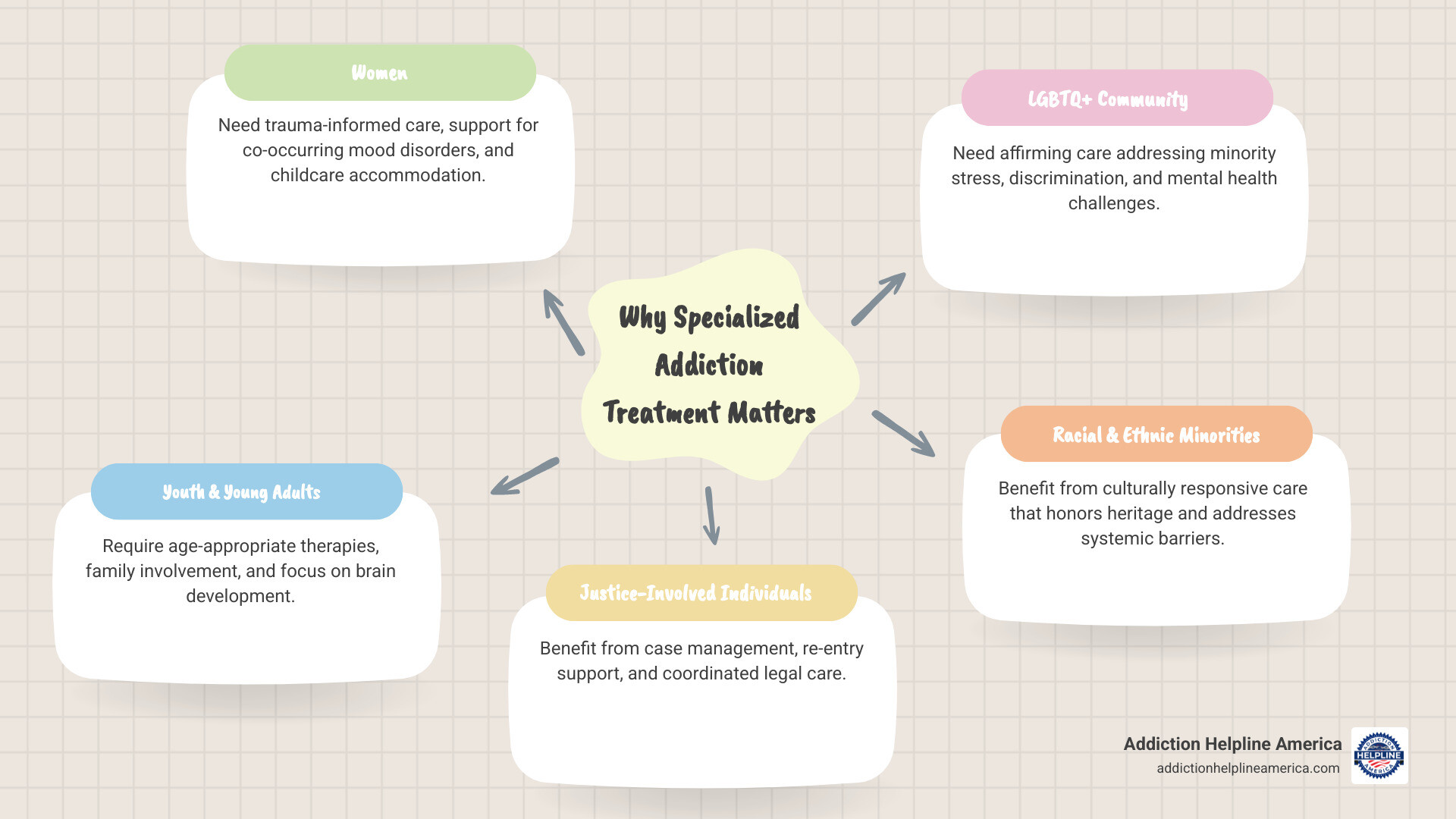
Key Populations Requiring Specialized Treatment:
- Women – Need trauma-informed care, support for co-occurring mood disorders, and accommodation for childcare responsibilities
- Youth and Young Adults – Require age-appropriate therapies, family involvement, and focus on brain development
- Justice-Involved Individuals – Benefit from case management, re-entry support, and coordinated care with legal systems
- LGBTQ+ Community – Need affirming care that addresses minority stress, discrimination, and higher rates of mental health challenges
- Older Adults – Require age-sensitive approaches addressing isolation, chronic pain, and medication interactions
- Racial and Ethnic Minorities – Benefit from culturally responsive care that honors heritage and addresses systemic barriers
- Veterans – Need trauma-focused treatment for combat-related PTSD and military cultural understanding
Addiction doesn’t look the same for everyone. A single mother struggling with opioid use faces different challenges than a teenager experimenting with alcohol or a veteran dealing with PTSD. Their paths to addiction are shaped by unique life experiences, trauma histories, cultural backgrounds, and social circumstances. Research confirms these differences; for example, the LGBTQ+ community experiences substance use at higher rates due to minority stress, and women may develop complications from alcohol use faster than men.
That’s why specialized treatment matters. When programs acknowledge these differences, recovery becomes more achievable. These aren’t just statistics—they’re real people who deserve care that sees them and provides the specific support they need to heal.
At Addiction Helpline America, we connect individuals with treatment programs that understand these unique needs. We know that effective Addiction Treatment for Specific Populations can make the difference between struggling alone and finding lasting recovery. We’re here to guide you to the right resources, free and confidentially, every step of the way.
Why a One-Size-Fits-All Approach Fails in Addiction Recovery
The journey to recovery is deeply personal, making a single treatment model ineffective for everyone. A “one-size-fits-all” approach overlooks the complex factors contributing to substance use, risking high dropout rates and failing to provide the support people need.
Diverse groups face unique challenges. Stigma varies across populations, sometimes compounded by cultural taboos or fear of legal or personal repercussions, like losing child custody. Co-occurring mental health disorders like anxiety, depression, or PTSD are common and require integrated treatment. A history of trauma, prevalent in many vulnerable populations, demands a sensitive, trauma-informed approach to prevent re-traumatization.
Beyond personal factors, social determinants of health like poverty, homelessness, and systemic discrimination create immense barriers. Practical issues such as a lack of transportation or childcare can make attending appointments impossible, while affordability remains a significant hurdle for many.
These are fundamental obstacles that require custom solutions. Ignoring them means even well-intentioned programs will fail. That’s why specialized approaches for Addiction Treatment for Specific Populations are essential for effective recovery. If you’re wondering how to find a program that understands your situation, find out how to choose the right rehab for your unique needs.
The Role of Cultural Competency in Treatment
Cultural competency is about understanding and respecting the values and beliefs that shape an individual’s worldview and approach to healing. Culturally competent providers build trust, the cornerstone of effective therapy. This involves addressing language barriers with interpreters or bilingual staff and understanding non-verbal communication, family dynamics, and community structures.
For example, treatment for American Indian and Alaska Native women must be trauma-informed and address historical trauma, while care for Black/African American women can be more effective with an Afrocentric perspective and community involvement. Integrating culturally specific healing practices, such as traditional ceremonies or spiritual guidance, makes recovery more resonant. Training staff in cultural competency is crucial for providing sensitive, affirming care and improving treatment engagement. The Substance Abuse and Mental Health Services Administration (SAMHSA) offers valuable resources on cultural competence for providers.
Overcoming Barriers to Accessing Care
Accessing addiction treatment can be a maze of practical and societal barriers. Financial constraints and lack of insurance are primary obstacles, as high deductibles or limited networks can make care unaffordable. For parents, especially single mothers, childcare responsibilities can make intensive programs impossible. Lack of reliable transportation also prevents consistent attendance.
Fear of legal or social consequences—such as losing a job, housing, or child custody—deters many from seeking help. The powerful stigma associated with addiction leads people to suffer in silence.
To address these challenges, low-barrier care models are essential. These models prioritize immediate access by reducing lengthy intake processes, rigid schedules, or sobriety requirements for admission. They focus on meeting individuals where they are. SAMHSA’s Advisory on Low Barrier Models of Care outlines principles for creating more accessible pathways to ensure more people get the help they need, when they need it.
Understanding the Unique Needs of Specific Populations
Tailoring treatment means acknowledging that each person’s story is unique. Effective Addiction Treatment for Specific Populations creates safe, affirming spaces that address not only the substance use but also the underlying risk factors and co-occurring issues prevalent within certain groups. This empowers individuals to heal in a way that respects their identity and lived experience.
Addiction Treatment for Women
Women often face distinct pathways to substance use, requiring specialized approaches. They may develop physiological complications from substances like alcohol faster than men and experience higher rates of co-occurring mood disorders like depression and anxiety. Over two-thirds of women with a substance use disorder (SUD) also reported a mental illness in the past year.
Trauma-informed care is essential, as women are more likely to have histories of trauma linked to SUDs. Treatment must provide a safe environment and help women develop coping strategies for PTSD. Childcare and family responsibilities are also significant barriers, so programs offering on-site childcare or flexible scheduling are vital. For pregnant women with opioid use disorder, specialized care that addresses the unique stresses of pregnancy is crucial.
Benefits of gender-specific programs for women include:
- A safe space to discuss sensitive issues.
- Focus on gender-specific topics like body image and relationships.
- Integrated treatment for co-occurring disorders.
- Parenting support and family therapy.
- Trauma therapy custom to women’s experiences.
- Prenatal and postnatal care.
- Supportive housing that accommodates children.
For an in-depth guide on treatment for women, SAMHSA’s resources offer further insights.
Addiction Treatment for Youth and Young Adults
Adolescence is a period of significant change, making youth vulnerable to substance use. Their treatment needs differ from adults due to ongoing brain development, peer influence, and their role within family and school systems. The adolescent brain’s developing prefrontal cortex makes them more susceptible to risky behaviors. Treatment must be engaging and age-appropriate.
Peer pressure is a powerful force, so youth programs often use group therapy to build refusal skills and positive peer support. Family involvement is also paramount, with counseling to improve communication and address family dynamics. Effective programs also collaborate with schools to support academic progress. Early intervention is key, focusing on building life skills like emotional regulation and healthy coping mechanisms.
Addiction Treatment for Justice-Involved Individuals
Individuals in the justice system face a cycle of addiction, crime, and incarceration. Upon release, they face immense pressure from probation requirements, housing instability, and employment difficulties, all of which can trigger relapse. Effective treatment requires intensive case management, coordinating care across legal, healthcare, and social service systems.
Re-entry support is crucial for navigating the return to society. Because many have histories of trauma and untreated mental illness, integrated, trauma-informed care is vital. Coordination with legal systems helps ensure treatment compliance is supported, not penalized, breaking the cycle and offering a path to sustainable recovery.
Affirming Addiction Treatment for Specific Populations: The LGBTQ+ Community
The LGBTQ+ community experiences higher rates of substance use disorders, often due to minority stress from societal discrimination and stigma. Fear of judgment from providers can be a major barrier to seeking care, leading to delayed treatment. Co-occurring mental health challenges like depression and anxiety are also prevalent.
Specialized programs with affirming and knowledgeable staff are crucial. They create a safe, welcoming environment where individuals feel understood and respected.
Benefits of specialized LGBTQ+ programs include:
- Staff trained in LGBTQ+ cultural competency.
- Group therapy addressing unique issues like coming out and discrimination.
- Integrated treatment for co-occurring mental health disorders.
- Safe spaces for transgender and non-binary individuals.
- Peer support from other LGBTQ+ individuals in recovery.
These programs offer custom support for more effective recovery. To learn more, explore The Ultimate Guide to LGBTQ+ Rehab Programs and Learn more about LGBTQ+ Inpatient Rehab.
Specialized Programs and Therapies: Keys to Effective Addiction Treatment for Specific Populations
Effective Addiction Treatment for Specific Populations uses a holistic approach, integrating mental and physical health care with evidence-based practices custom to individual needs. This involves a range of therapeutic modalities and support systems that address an individual’s full well-being to create a sustainable path to recovery.
The Power of Trauma-Informed and Dual Diagnosis Care
Trauma and addiction are often intertwined, as many people use substances to cope with the pain of past abuse, neglect, or violence. Trauma-informed care is a critical approach that recognizes the widespread impact of trauma. Its core principles are creating safety, trustworthiness, peer support, collaboration, and empowerment, all to avoid re-traumatization during treatment and promote healing.
Equally important is dual diagnosis care, or integrated treatment for co-occurring disorders. Many people with substance use disorders also have mental health conditions like anxiety, depression, or bipolar disorder. Treating both conditions simultaneously is far more effective, as they are often interconnected. In Arizona, for example, many facilities specialize in this integrated approach; you can find Dual Diagnosis treatment centers in Arizona that understand these complex needs.
Effective Group Therapy Models
Group therapy is a cornerstone of addiction treatment, offering support and skill development. Various models are used for Addiction Treatment for Specific Populations, as outlined by SAMHSA’s Treatment Improvement Protocol (TIP) Series, No. 41:
- Psychoeducational Groups: Educate clients about substance abuse, its consequences, and the recovery process to increase awareness and motivation.
- Skills Development Groups: Cultivate practical skills needed to maintain abstinence, such as managing urges, refusing substances, and coping with stress.
- Cognitive-Behavioral Therapy (CBT) Groups: Help individuals identify and change problematic thinking patterns and behaviors that contribute to substance use.
- Support Groups: Provide emotional sustenance, encouragement, and a sense of community where members share experiences and offer mutual aid.
- Interpersonal Process Groups: Use the group’s “here and now” dynamics as a therapeutic tool to explore relationship patterns and improve communication.
- Relapse Prevention Groups: Teach strategies to anticipate and manage high-risk situations that could lead to relapse.
Here’s a quick comparison of two foundational group models:
| Feature | Psychoeducational Groups | Skills Development Groups |
|---|---|---|
| Primary Focus | Education about addiction, consequences, and recovery | Teaching practical coping and life skills for abstinence |
| Goal | Increase knowledge, motivation, and understanding | Build behavioral competencies, self-efficacy |
| Activities | Lectures, discussions, videos, handouts, expert sharing | Role-playing, practice exercises, homework assignments |
| Leadership | Facilitator as educator/expert | Facilitator as coach/trainer |
The Role of Community and Long-Term Support
Recovery is a marathon, not a sprint, and it extends far beyond initial treatment. Sustained recovery relies on robust community and long-term support systems. Community-based services like outpatient clinics and peer support groups provide accessible, ongoing care. Peer support specialists, who have lived experience in recovery, offer invaluable guidance and empathy.
Aftercare programs are crucial for transitioning back to daily life, reinforcing coping skills through group meetings or individual counseling. Supportive housing is essential for those needing a stable, substance-free living environment, such as women with children or justice-involved individuals. Building a sober social network through 12-step programs, SMART Recovery, or other groups provides a sense of belonging and accountability. This continuing care provides the scaffolding necessary to build a fulfilling life in recovery.
Building a Bridge to Recovery: Innovations and Support
The landscape of addiction treatment is constantly evolving to be more accessible and effective. Adapting services to meet people where they are—rather than forcing them into rigid systems—is a cornerstone of modern care, leveraging technology and community partnerships to create a comprehensive support network.
How Healthcare Facilities Can Adapt
To effectively serve diverse populations, healthcare facilities must accept flexibility and inclusivity. This includes offering flexible program schedules, such as evening or weekend sessions, and providing on-site childcare to accommodate parents. Integrated services that house multiple types of care under one roof streamline the process and improve coordination.
Mandatory staff training in cultural competency ensures all personnel respect the diverse backgrounds of their clients. Creating a welcoming environment means actively promoting an atmosphere of non-judgment and safety, especially for vulnerable groups like the LGBTQ+ community. Using person-first language, such as saying “a person with a substance use disorder” instead of “addict,” is a simple but powerful way to foster dignity.
Leveraging Technology and Telehealth
Technology, especially telehealth, has revolutionized addiction treatment by bridging access gaps. For individuals in rural areas or those who are homebound, telehealth eliminates barriers like transportation and makes care more convenient. Virtual support groups also foster a sense of community regardless of geographic location.
Mobile health apps provide tools for relapse prevention, mood tracking, and medication reminders directly on a smartphone. This constant connection is invaluable for maintaining sobriety. Telehealth also improves continuity of care by allowing individuals to stay connected with their treatment team after leaving an inpatient program, reducing the risk of relapse. By embracing these advancements, we can expand the reach of addiction treatment. If you’re looking for flexible options, we can help you find a treatment center that offers telehealth services.
Frequently Asked Questions about Specialized Addiction Treatment
What is gender-specific addiction treatment?
Gender-specific addiction treatment recognizes that men and women often have different pathways to addiction, unique co-occurring issues, and distinct recovery needs. These programs create a safe environment where individuals can focus on recovery without societal pressures or distractions related to gender. For women, this often involves addressing trauma, family roles, childcare needs, reproductive health, and co-occurring mood disorders. Programs for men may focus on emotional expression, societal expectations of masculinity, anger management, and family responsibilities. By tailoring the environment and therapeutic content, gender-specific programs improve engagement and improve outcomes.
How do I know if I need a specialized addiction program?
If you feel your identity, past experiences, or specific life circumstances are a major factor in your substance use, a specialized program may be beneficial. Consider if you belong to a group with unique challenges, such as being a veteran, a member of the LGBTQ+ community, a pregnant woman, a parent, or someone with a history of significant trauma or a co-occurring mental health diagnosis. If you’ve tried traditional treatment and found it didn’t fully address your underlying issues, a specialized approach might be the key. A confidential assessment with a qualified professional can help determine the best fit for your unique situation.
Where can I find help for a crisis right now?
If you or someone you know is in immediate crisis, you can connect with people who can support you by calling or texting 988 anytime in the United States. The 988 Suicide & Crisis Lifeline is free, confidential, and available 24/7. For veterans, the Veterans Crisis Line is also available by calling 988 and pressing 1, or by texting 838255. These resources can provide immediate support and connect you with local services.
Your Personalized Path to Healing Starts Here
Recovery is not just a possibility; it’s a reality for millions of Americans, and the right support can make all the difference. Taking the first step towards seeking help is often the bravest decision an individual can make, and we want you to know that you are not alone in this journey.
At Addiction Helpline America, we believe that effective Addiction Treatment for Specific Populations is crucial for lasting recovery. We are dedicated to connecting individuals nationwide to treatment centers that understand your unique needs, whether you’re a woman seeking trauma-informed care in California, a young adult needing age-appropriate therapy in Texas, or an LGBTQ+ individual looking for affirming support in New York. Our guidance is always free and confidential, providing you with personalized options from our vast network of trusted providers across the United States.
Find the right program for you or a loved one by calling our 24/7 helpline at 844-561-0606 or visiting our guide on choosing the right rehab. Your personalized path to healing starts now.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.