Understanding Suboxone Withdrawal: What You Need to Know
Suboxone withdrawal symptoms are a critical concern for anyone considering stopping this medication. If you’re searching for quick answers, here’s what you need to know:
Common Suboxone Withdrawal Symptoms:
- Physical Symptoms: Nausea, vomiting, muscle aches, headaches, sweating, chills, diarrhea, insomnia, fatigue
- Psychological Symptoms: Anxiety, depression, irritability, mood swings, intense drug cravings, difficulty concentrating
- Timeline: Symptoms typically begin 12-48 hours after the last dose, peak within the first 72 hours, and physical symptoms usually subside within 10 days to a month
- Duration: While physical symptoms may resolve within a few weeks, psychological symptoms like cravings and depression can persist for several months
Nobody really talks enough about what it feels like to face these symptoms. Some days hit harder than you think they will. It’s not just the cravings—it’s the tiredness, the bad moods, the nights you can’t sleep even though you’re exhausted.
Suboxone is an FDA-approved medication designed to help people recover from opioid addiction. It contains buprenorphine (a partial opioid agonist) and naloxone (an opioid antagonist). While Suboxone saves lives by easing withdrawal from more dangerous opioids, your body can become physically dependent on it too. When you stop taking it—especially abruptly—your brain chemistry struggles to readjust, leading to withdrawal symptoms.
The good news? You don’t have to face this alone. With proper medical guidance and support, withdrawal can be managed safely and effectively.
At Addiction Helpline America, we’ve helped countless individuals and families steer the challenges of suboxone withdrawal symptoms, connecting them with compassionate, evidence-based treatment options 24/7. Our team understands that seeking help takes courage, and we’re here to provide the confidential guidance you need. Call us at 844-561-0606 anytime—day or night—to speak with someone who cares.
What is Suboxone and Why Does Withdrawal Occur?
Suboxone has become a cornerstone in the fight against the opioid crisis, offering a lifeline to many struggling with opioid use disorder (OUD). But what exactly is it, and why does stopping it lead to such challenging withdrawal symptoms?
Suboxone is an FDA-approved medication used in medication-assisted treatment (MAT) for opioid use disorder. It’s not a single drug but a combination of two active ingredients: buprenorphine and naloxone.
- Buprenorphine: This is a partial opioid-agonist. Think of it like a dimmer switch for opioid receptors in your brain. It activates these receptors, but only partially. This activation helps to reduce opioid cravings and withdrawal symptoms without producing the intense “high” associated with full opioid agonists like heroin or oxycodone. Buprenorphine also has a “ceiling effect,” meaning that after a certain dose, taking more won’t produce a proportionally greater effect, which reduces the risk of overdose.
- Naloxone: This is an opioid antagonist, or blocker. Its purpose in Suboxone is to deter misuse. If someone tries to inject Suboxone, the naloxone will block opioid receptors, potentially causing immediate and uncomfortable withdrawal symptoms. When taken as prescribed (sublingually), naloxone is poorly absorbed and doesn’t interfere with buprenorphine’s effects.
Why Withdrawal Occurs
The reason Suboxone withdrawal symptoms occur is rooted in how our bodies adapt to substances. When you regularly use opioids, even a partial agonist like buprenorphine, your body develops a physical dependence. This isn’t necessarily addiction, but rather a physiological adaptation where your brain and body become accustomed to the presence of the drug.
Opioids, including buprenorphine, interact with your brain’s reward system, particularly by influencing dopamine levels. Dopamine is a neurotransmitter associated with pleasure and motivation. When you consistently introduce an external substance that stimulates this system, your brain’s natural production and regulation of these chemicals can change.
When you suddenly reduce or stop taking Suboxone, your body is left scrambling. It’s like your brain’s chemistry is trying to rebalance itself after having a steady supply of buprenorphine. This sudden absence leads to a decrease in dopamine levels and other neurochemical imbalances, triggering the cascade of uncomfortable physical and psychological reactions we know as withdrawal. Your body essentially goes into overdrive trying to feel “normal” again without the medication it has grown to rely on.
Common Suboxone Withdrawal Symptoms
Experiencing withdrawal can feel overwhelming, but understanding what to expect is the first step toward managing it effectively. Suboxone withdrawal symptoms share many similarities with other opioid withdrawals, but they also have some unique characteristics due to buprenorphine’s properties.
Generally, withdrawal symptoms can be categorized into physical and psychological. While early symptoms tend to be more physical, psychological symptoms can linger much longer, making them a significant challenge in recovery. Suboxone withdrawal symptoms often build up more slowly but can last longer than withdrawals from shorter-acting opioids, thanks to buprenorphine’s extended half-life.
Common Physical Suboxone Withdrawal Symptoms
The physical symptoms of Suboxone withdrawal can feel like a severe case of the flu, amplified and prolonged. We know these symptoms can be incredibly uncomfortable, and it’s why medical supervision is so important. Here’s a list of what you might experience:
- Nausea and vomiting: Often accompanied by stomach cramps and general digestive distress.
- Muscle aches and pains: These can range from mild discomfort to severe, widespread body aches.
- Headaches: Persistent and sometimes intense.
- Sweating: Profuse sweating, often accompanied by chills.
- Chills: Feeling cold, often with gooseflesh.
- Diarrhea: Can contribute to dehydration.
- Runny nose and watery eyes: Similar to allergy symptoms.
- Fatigue: Extreme tiredness and lethargy.
- Insomnia: Difficulty falling or staying asleep, even when exhausted.
- Dilated pupils: A common sign of opioid withdrawal.
- Overactive reflexes: Restlessness, particularly in the legs.
- Fast breathing and heart rate: Your body’s stress response.
- High blood pressure and body temperature: Further signs of physiological distress.
- Yawning: Frequent and uncontrollable yawning.
Physical symptoms commonly begin within 24 hours after the last dose and can last for approximately 10 days.
Psychological Suboxone Withdrawal Symptoms and Their Impact
While the physical discomfort of withdrawal is undeniable, the psychological Suboxone withdrawal symptoms can be just as, if not more, challenging. These symptoms can be insidious, eroding your motivation and making it incredibly difficult to maintain sobriety.
- Anxiety: A pervasive sense of unease, worry, and nervousness.
- Depression: Feelings of sadness, hopelessness, and a loss of interest in activities once enjoyed.
- Irritability: Short temper and increased frustration.
- Mood swings: Rapid and unpredictable shifts in mood, from anger to sadness to agitation.
- Intense cravings: A powerful urge to use opioids again to alleviate discomfort.
- Difficulty concentrating: Problems focusing, remembering, and making decisions.
- Restlessness: An inability to relax or sit still, often contributing to insomnia.
- Relapse dreams: Vivid dreams related to drug use.
These psychological symptoms are not just unpleasant; they are a potent cause of relapse. The emotional distress and persistent cravings can push individuals back to substance use, even when they desperately want to quit. This is why comprehensive treatment, including therapy and ongoing support, is so vital. After one month, users will likely still be experiencing intense cravings and depression, highlighting the prolonged battle against these invisible symptoms.
If you or a loved one are facing these challenging symptoms, you don’t have to go through it alone. Call Addiction Helpline America at 844-561-0606 to speak with a compassionate specialist who can guide you toward help.
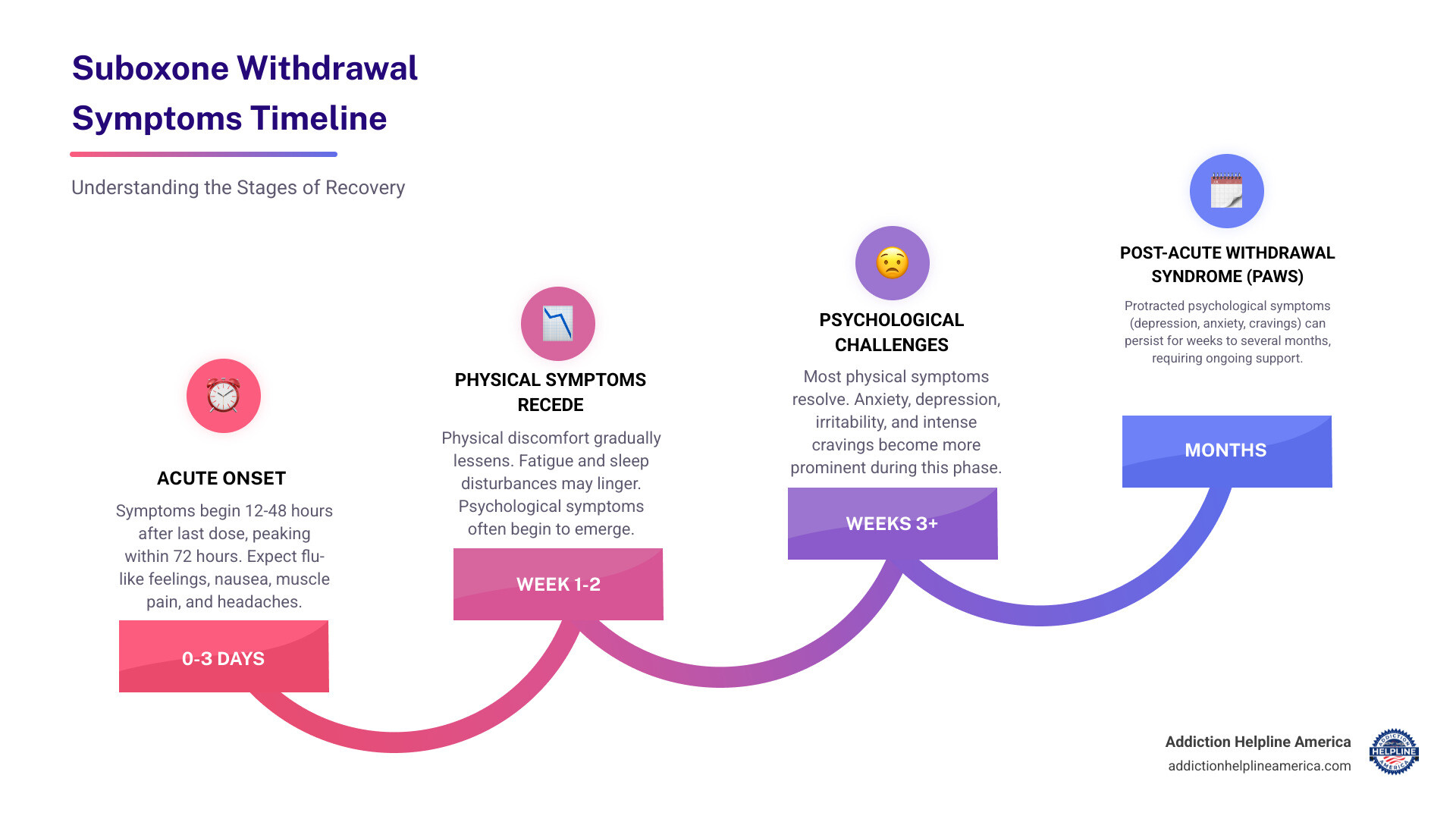
Understanding the Suboxone Withdrawal Symptoms Timeline
Navigating Suboxone withdrawal symptoms can feel like an endless journey, but understanding the typical timeline can provide much-needed clarity and help you prepare. This is a general guide; individual experiences can vary based on factors like dosage, duration of use, overall health, and genetics.
A key factor influencing the timeline is buprenorphine’s long half-life, which can range from 28 to 37 hours when dissolved under the tongue. This means it takes a longer time for the drug to be eliminated from your system, leading to a delayed onset and often a more prolonged, though generally less acute, withdrawal compared to shorter-acting opioids.
Typically, withdrawal symptoms usually start anywhere between 12 and 48 hours following the last dosage. For some individuals, symptoms may even occur within 24 hours. The initial days are often the most challenging, with symptoms gradually subsiding over the following weeks.
We understand that every moment can feel like an eternity when you’re going through withdrawal. If you need immediate guidance or just someone to talk to, please call Addiction Helpline America at 844-561-0606. We’re here 24/7 to help.
First 72 Hours: The Acute Phase
This is often when Suboxone withdrawal symptoms hit their peak. After you stop taking Suboxone, it usually takes 3-5 days before enough of the drug is removed from the body to produce significant withdrawal symptoms. However, as mentioned, symptoms can start earlier for some.
During these first three days, you can expect the physical symptoms to be at their worst. This phase often feels like a severe flu, characterized by:
- Intense body aches and muscle pain
- Nausea and vomiting
- Headaches
- Profuse sweating and chills
- Diarrhea
- Difficulty sleeping
- General malaise and extreme fatigue
While incredibly uncomfortable, it’s crucial to remember that this acute phase is temporary. Medical support during this time can make a world of difference in managing these intense feelings. For more information on what to expect during acute opioid withdrawal, you can refer to resources like this information on acute opioid withdrawal.
Week 1-2: Physical Symptoms Subside
After the initial 72-hour peak, many physical Suboxone withdrawal symptoms begin to gradually lessen in intensity. You might notice that the severe body aches aren’t as crippling, and nausea might become more manageable.
However, lingering physical discomforts are common. Fatigue can persist, and sleep disturbances often remain a significant challenge. You might find yourself exhausted but unable to achieve restful sleep.
As physical symptoms start to recede, psychological symptoms often become more prominent. Anxiety, irritability, and mood swings can intensify, making this period emotionally taxing. It’s a tricky time because while your body might feel a bit better, your mind is still very much in the throes of withdrawal.
Week 3 to Month 1+: The Post-Acute Phase
By the third week, most of the acute physical Suboxone withdrawal symptoms have typically subsided. You might feel a sense of relief, but the journey isn’t over. This phase is largely dominated by persistent psychological symptoms, which can be just as debilitating as the physical ones.
Common symptoms during this post-acute phase include:
- Depression: Feelings of sadness and lack of motivation can be profound.
- Anxiety: A lingering sense of worry, unease, or panic.
- Cravings: Intense urges to use opioids, which can come and go in waves.
- Mood swings: Emotional volatility can make daily life challenging.
- Difficulty concentrating: Mental fog and impaired cognitive function.
These lingering psychological symptoms are often referred to as protracted withdrawal symptoms or, in some cases, Post-Acute Withdrawal Syndrome (PAWS). PAWS can involve a collection of symptoms that may persist for weeks, months, or even a year or more after acute withdrawal. For Suboxone, these prolonged symptoms are more commonly known as protracted withdrawal symptoms.
The statistics tell us that while most physical symptoms disappear within a month, users will likely still be experiencing intense cravings and depression after one month. This highlights the critical need for continued support and therapeutic intervention well beyond the initial detox period.
How to Safely Manage Suboxone Withdrawal
The thought of enduring Suboxone withdrawal symptoms can be daunting, and for good reason. It’s a challenging process, but it’s crucial to approach it safely and strategically. The most important takeaway here is the absolute necessity of medical supervision. Trying to manage withdrawal alone can be not only incredibly uncomfortable but also dangerous.
We cannot emphasize enough that discontinuing Suboxone should always be done under the guidance of a healthcare professional. They can help you develop a personalized plan, monitor your symptoms, and intervene if complications arise.
The Dangers of Quitting Cold Turkey
Quitting Suboxone “cold turkey” is a path fraught with risks, and we strongly advise against it. While withdrawal from Suboxone itself is rarely fatal, the severe and intense symptoms can lead to dangerous situations.
- Intense and Severe Symptoms: Abrupt cessation can lead to an onslaught of severe physical and emotional distress. Imagine the worst flu you’ve ever had, combined with extreme anxiety and depression. This level of discomfort is not only agonizing but can also be overwhelming.
- Increased Risk of Relapse: The primary danger of quitting cold turkey is the significantly increased risk of relapse. When faced with unbearable Suboxone withdrawal symptoms, individuals often return to opioid use to find relief. This is particularly perilous because after a period of abstinence, your opioid tolerance is reduced. If you use the same dosage you did before withdrawal, the risk of accidental overdose becomes incredibly high.
- Potential for Medical Complications: Although direct fatality from Suboxone withdrawal is rare, severe vomiting and diarrhea can lead to significant dehydration and electrolyte imbalances. In extreme cases, these complications can be life-threatening, especially if not medically managed. Research on opioid withdrawal fatalities indicates that deaths from opioid withdrawal usually occur due to these secondary complications, often in unmonitored environments like jails where medical care is scarce (only 10-12% of U.S. county jails have drug detox services available).
Medically-Supervised Tapering
The recommended and safest approach to discontinuing Suboxone is through a medically-supervised tapering plan. This involves gradually reducing your dose over time, allowing your body to slowly adjust to less and less of the medication. This process helps to minimize the severity of Suboxone withdrawal symptoms, making the experience much more tolerable.
A physician, often a Suboxone doctor or addiction specialist, will work with you to create a personalized tapering schedule. This might involve dose reductions of no more than 5-10% every two to three weeks. The key is flexibility: if withdrawal symptoms emerge and become too uncomfortable, your doctor can slow down the taper or even pause it until you stabilize. This controlled and compassionate approach significantly improves your chances of a successful and lasting recovery. You can find more comprehensive patient information on Suboxone use directly from the manufacturer.
Medications and Support for Withdrawal
Even with a careful taper, some Suboxone withdrawal symptoms are likely to occur. The good news is that there are various medications and supportive strategies available to help manage these discomforts.
-
Comfort Medications:
- Lucemyra (lofexidine hydrochloride): This is an FDA-approved medication specifically for opioid withdrawal. It works by reducing norepinephrine, a neurotransmitter involved in withdrawal symptoms. Unlike Suboxone, Lucemyra does not contain an opioid agonist.
- Clonidine: An older blood pressure medication, clonidine for withdrawal symptoms can be used off-label to regulate central nervous system functions and alleviate symptoms like anxiety, sweating, and muscle aches.
- Buspirone (Buspar): This anti-anxiety medication has shown effectiveness in treating opioid withdrawal symptoms. One small study even found Buspar to be as effective as a methadone taper for alleviating opioid withdrawal symptoms.
- Sleep Aids: Medications like zopiclone or eszopiclone (Lunesta) can be useful for managing insomnia, a common and frustrating withdrawal symptom.
- Other Supportive Medications: Your doctor might also prescribe mood stabilizers, gastrointestinal medications for nausea and diarrhea, or nonsteroidal analgesics (like ibuprofen) and acetaminophen for pain relief.
-
Therapeutic Support: Medications can manage the physical aspects, but therapy is crucial for addressing the psychological and emotional challenges. Individual and group counseling can provide coping strategies, address underlying issues, and help you steer the emotional rollercoaster of withdrawal.
- Coping Strategies: Beyond medication, self-care and behavioral strategies are vital. Engaging in social activities, pursuing hobbies, and practicing relaxation techniques can help distract from cravings and ease emotional distress. Adopting a positive outlook, even when it’s tough, can help replace feelings of shame with satisfaction and pride in your recovery journey.
If you’re struggling with Suboxone withdrawal symptoms and need to discuss treatment options, please don’t hesitate to call Addiction Helpline America at 844-561-0606. Our compassionate team can help you understand your choices and connect you with the right support.
Finding Professional Help for Long-Term Recovery
Successfully navigating Suboxone withdrawal symptoms is a monumental achievement, but it’s often just the first step on a longer journey toward lasting recovery. We’ve learned that detox alone is rarely sufficient for long-term abstinence. Comprehensive treatment that addresses the underlying causes of addiction is essential.
At Addiction Helpline America, we understand this journey intimately. We connect individuals across our vast network in states like Alabama, Arizona, California, Florida, Illinois, New York, Texas, and many more, to custom treatment solutions. We believe in providing personalized guidance to help you find the right program. For a free, confidential consultation to explore your options, call Addiction Helpline America at 844-561-0606.
Professional help typically involves:
- Medical Detox: This initial phase focuses on safely managing withdrawal symptoms under medical supervision. It provides a controlled environment where discomfort can be minimized, and any medical complications can be immediately addressed.
- Inpatient vs. Outpatient Rehab: After detox, individuals transition into either inpatient (residential) or outpatient programs. Inpatient programs offer 24/7 care and a structured environment, ideal for those needing intensive support. Outpatient programs allow individuals to live at home while attending therapy and group sessions, suitable for those with strong support systems and fewer severe symptoms.
The Role of Therapy in Recovery
Therapy is not just helpful; it’s often considered the key to maintaining sobriety for the long term. Without it, the risk of relapse significantly increases. Therapy helps individuals understand the roots of their addiction, develop healthy coping mechanisms, and build a fulfilling life without substances. According to NIDA’s guide to treatment approaches, various therapeutic modalities are effective:
- Cognitive-Behavioral Therapy (CBT): Helps individuals identify and change negative thought patterns and behaviors that contribute to substance use.
- Dialectical Behavior Therapy (DBT): Focuses on emotional regulation, mindfulness, and distress tolerance.
- Contingency Management (CM): Uses positive reinforcement to encourage abstinence.
- Individual Counseling: Provides a one-on-one setting to explore personal issues, trauma, and develop coping strategies.
- Group Therapy: Offers peer support, shared experiences, and a sense of community, reducing feelings of isolation.
- Family Therapy: Involves family members in the recovery process, addressing family dynamics and improving communication.
Support Groups and Aftercare
Building a strong support network and having a solid aftercare plan are crucial for sustained recovery.
- 12-Step Programs: Peer support groups like Alcoholics Anonymous (AA) and Narcotics Anonymous (NA) have proven beneficial for millions. The 12-Step treatment structure offers a philosophy and group session style that provides positive support and guidance in recovery.
- Peer Support Networks: Connecting with others who have similar experiences can provide invaluable empathy, understanding, and accountability.
- Relapse Prevention Planning: Developing strategies to identify and manage triggers, cope with cravings, and steer high-risk situations is a critical component of aftercare.
- Building a Sober Life: Long-term aftercare often includes continued therapy, sober living arrangements, vocational training, and engagement in healthy activities to foster a fulfilling, substance-free life.
Frequently Asked Questions about Suboxone Withdrawal
We hear many questions about Suboxone withdrawal symptoms, and get clear, accurate answers. Here are some of the most common inquiries we address:
How long do Suboxone withdrawal symptoms last?
The duration of Suboxone withdrawal symptoms can vary significantly from person to person, but we can outline a general timeline:
- Acute Phase: Physical symptoms typically begin 12-48 hours after the last dose, peak within the first 72 hours, and generally subside within 10 days to a month. Most physical symptoms disappear within a month.
- Psychological Symptoms: These can be more tenacious. Symptoms like anxiety, depression, mood swings, and intense cravings can persist for several weeks or even months after the physical discomfort has faded.
- Post-Acute Withdrawal Syndrome (PAWS): For some, a lingering collection of symptoms known as PAWS can occur, lasting for a year or more. For Suboxone, this is often referred to as protracted withdrawal symptoms.
Overall, while the worst of the physical symptoms typically pass relatively quickly, the entire withdrawal process, especially the psychological aspects, usually doesn’t last more than a few months.
Is Suboxone withdrawal worse than from other opioids?
This is a common question, and the answer is nuanced. Suboxone withdrawal symptoms are generally considered less acutely intense than withdrawal from full opioid agonists like heroin or powerful prescription painkillers. This is because buprenorphine is a partial agonist and has a ceiling effect, meaning it doesn’t activate opioid receptors as fully or intensely.
However, due to buprenorphine’s long half-life (up to 42 hours), Suboxone withdrawal tends to be more prolonged. Symptoms may take longer to appear and can linger for a longer duration compared to shorter-acting opioids, where withdrawal symptoms hit faster and harder.
The severity and duration of withdrawal are also influenced by individual factors such as:
- Age and gender
- General health, including liver and kidney function
- Genetic predispositions
- The dosage and duration of Suboxone use
- The presence of co-occurring mental health conditions or other substance use.
Can you die from Suboxone withdrawal?
Withdrawal from Suboxone withdrawal symptoms on its own is rarely fatal. This is a crucial distinction from withdrawal from certain other substances, like alcohol or benzodiazepines, which can be directly life-threatening.
However, this doesn’t mean Suboxone withdrawal is without risks. The severe discomfort, particularly from intense vomiting and diarrhea, can lead to significant dehydration and electrolyte imbalances. If these are not medically managed, they can indeed become serious and, in rare instances, life-threatening. This risk is amplified when individuals attempt to withdraw without medical supervision.
Therefore, while direct fatality from Suboxone withdrawal is extremely rare, the potential for severe complications underscores why medical supervision is absolutely critical during the detoxification process. It ensures that any adverse effects are promptly addressed, keeping you safe and as comfortable as possible.
Start Your Recovery from Suboxone Dependence Today
Facing Suboxone withdrawal symptoms can feel like an impossible challenge, but we want you to know that overcoming dependence is absolutely possible. Your journey toward a healthier, substance-free life can begin today, and you don’t have to walk it alone.
Professional help is not just an option; it’s a key to navigating withdrawal safely and building a foundation for lasting recovery. At Addiction Helpline America, we pride ourselves on providing free, confidential, and personalized guidance. We connect individuals nationwide—from Alabama to Wyoming, and every state in between—to the right addiction and mental health treatment centers within our vast network. Our goal is to assess your unique needs and help you find a recovery program that fits you perfectly.
Whether you’re just starting to explore your options, are ready to begin a medically-supervised taper, or need support for the psychological challenges of protracted withdrawal, we are here for you. Our team of compassionate experts is available 24/7 to listen, understand, and guide you without judgment.
Take the courageous first step toward your recovery and connect with the help you deserve.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.