Understanding Suboxone: A Life-Saving Treatment for Opioid Addiction
Suboxone for opioid addiction is an FDA-approved medication combining buprenorphine and naloxone to help people recover from opioid use disorder. This treatment reduces cravings, prevents withdrawal, and lowers the risk of fatal overdose by approximately 50%.
Quick Facts About Suboxone for Opioid Addiction:
- What it is: A prescription medication with buprenorphine (a partial opioid agonist) and naloxone (an opioid antagonist).
- How it works: Fills opioid receptors without causing a high, blocking other opioids and stabilizing brain chemistry.
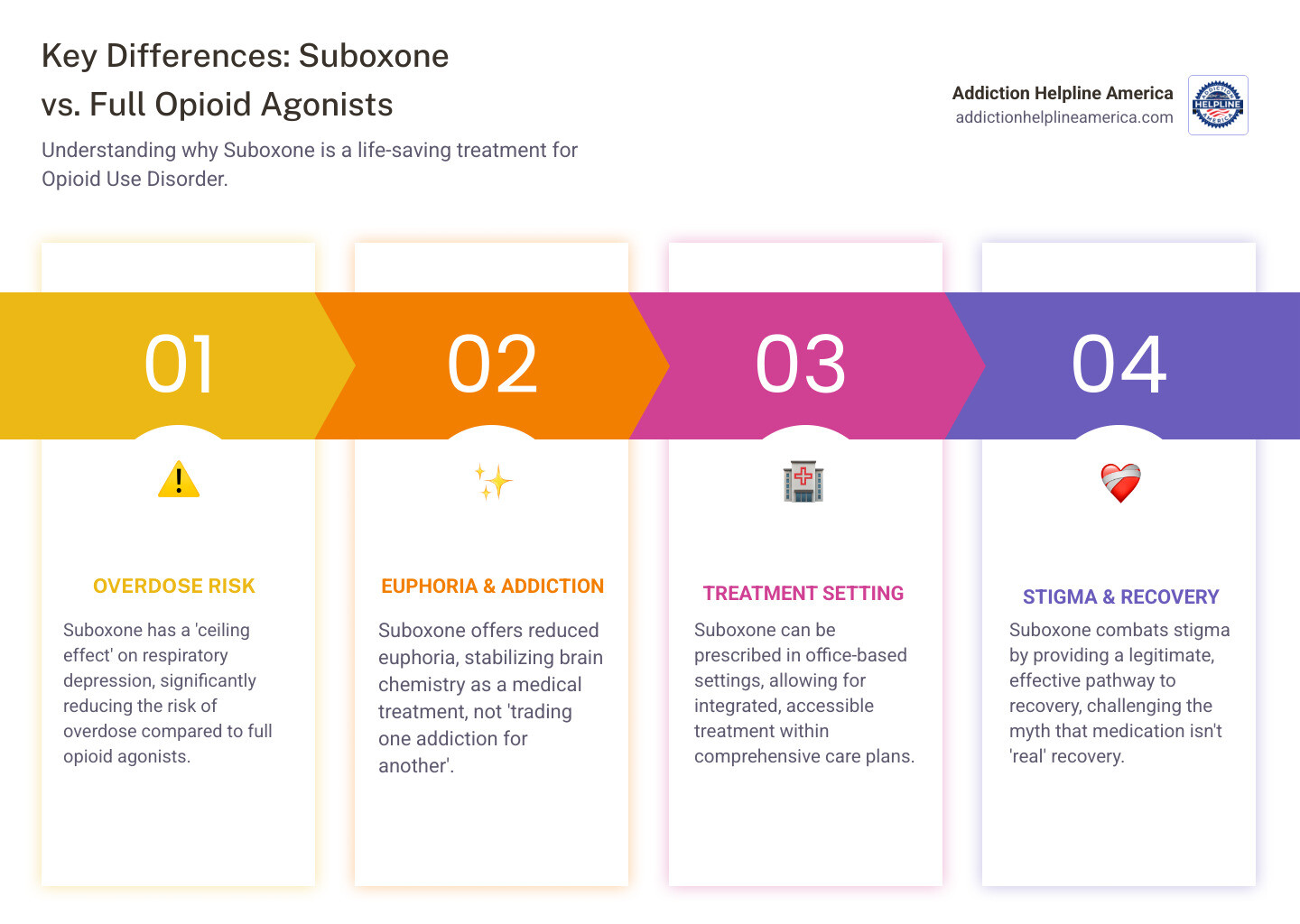
- Safety: Lower overdose risk than methadone due to a “ceiling effect” that limits respiratory depression.
- Treatment setting: Can be prescribed in a doctor’s office, unlike methadone which requires specialized clinics.
- Duration: No set time limit; treatment can last months to years based on individual needs.
- Effectiveness: Most successful when combined with counseling, but medication alone is proven effective.
If you’re struggling with addiction to heroin, fentanyl, or prescription painkillers, Suboxone offers a medically proven path to recovery. It’s not “trading one addiction for another” but using medicine to treat a chronic medical condition, similar to how insulin treats diabetes.
The journey to recovery can feel overwhelming. Many worry about withdrawal, finding treatment, or if recovery is even possible. Suboxone breaks this cycle by allowing your brain to heal while you focus on rebuilding your life.
At Addiction Helpline America, we connect individuals with qualified providers for Suboxone for opioid addiction treatment. Our experience shows that with the right medical care, lasting recovery is not just possible—it’s probable.
How Suboxone Works: The Science of Recovery
Understanding how Suboxone for opioid addiction works can build confidence in the treatment. The science is reassuring: it’s designed to work with your brain to support recovery.
Suboxone contains two key ingredients: buprenorphine and naloxone. Buprenorphine stabilizes your brain chemistry, while naloxone acts as a safety guard to prevent misuse.
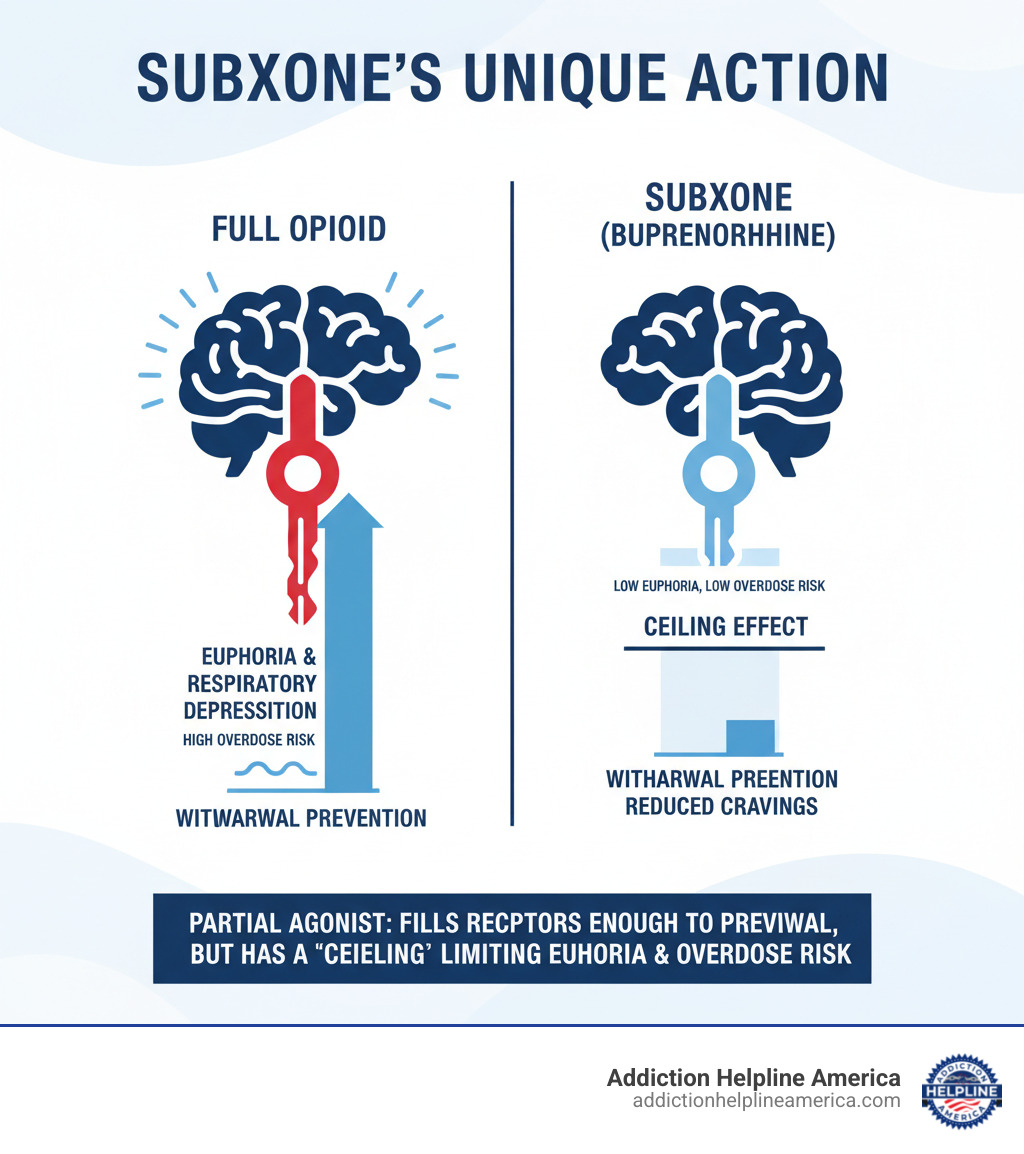
Buprenorphine is a partial opioid agonist. Unlike full opioids like heroin or fentanyl that completely activate your brain’s opioid receptors, buprenorphine only partially activates them. It provides just enough activation to prevent withdrawal and cravings without the dangerous highs.
This partial activation creates a “ceiling effect,” one of Suboxone’s most important safety features. Once you reach a certain dose, taking more won’t increase the effects, especially dangerous ones like slowed breathing. This makes it much safer than other opioids, significantly reducing overdose risk.
Naloxone provides built-in protection against misuse. When taken as prescribed (dissolved under the tongue), very little naloxone is absorbed. If injected or snorted, the naloxone activates, blocking opioid effects and causing immediate withdrawal. This deters misuse.
You can learn more about the detailed mechanisms by visiting this resource: How buprenorphine works.
Understanding the Role of Suboxone for Opioid Addiction Treatment
Suboxone for opioid addiction works on multiple levels. Because buprenorphine binds strongly to opioid receptors, it blocks other opioids from taking effect. This means if you use other opioids while on Suboxone, you won’t feel the high, helping break the cycle of use.
More importantly, Suboxone stabilizes your brain chemistry so daily life becomes manageable again. Addiction changes how your brain works, creating intense cravings. By occupying opioid receptors with a safer medication, your brain can start to heal and function more normally.
This stabilization dramatically reduces illicit opioid use because you’re no longer driven by cravings or fear of withdrawal. The long-acting effects of buprenorphine (24-36 hours) mean you usually only need one dose per day. This stability breaks the cycle of active addiction, allowing you to focus on recovery, not just survival.
Is Suboxone Addictive and What is the Overdose Risk?
A common concern is “trading one addiction for another.” This is based on a misunderstanding.
Physical dependence is not addiction. Your body becomes dependent on Suboxone, like a person with diabetes depends on insulin. Addiction involves compulsive, harmful drug-seeking. Suboxone helps you regain control over these behaviors.
The overdose risk from Suboxone alone is extremely low due to its ceiling effect. It’s difficult to overdose on prescribed buprenorphine because of its built-in limit on respiratory depression.
However, the risk increases significantly when combined with other depressants like benzodiazepines (Xanax, Valium) or alcohol. These combinations can be dangerous.
This is why we recommend people on Suboxone and their loved ones keep naloxone kits available. Naloxone can reverse an opioid overdose and is an essential safety tool. You can learn more about accessing these life-saving kits through our Take Home Naloxone information.
The bottom line is that Suboxone, used as prescribed, offers a much safer path than continued illicit opioid use. It’s not about being “drug-free”—it’s about being free from the chaos of addiction.
The Benefits and Risks of Using Suboxone for Opioid Addiction
Suboxone for opioid addiction has helped thousands reclaim their lives. Like any medication, it’s important to understand both its benefits and risks.
The Life-Changing Benefits of Suboxone
The most compelling benefit of Suboxone is that it can save your life. Studies show medications for addiction treatment like Suboxone lower fatal overdose risk by 50%.
Beyond survival, Suboxone opens the door to living again. People on Suboxone show increased treatment retention, meaning they are more likely to stick with their recovery program, a strong predictor of long-term success.
The improved quality of life is profound. When not battling withdrawal or seeking drugs, you can focus on what matters: work, relationships, and personal interests. This path to normalcy is about reclaiming your identity and future.
Suboxone also offers practical advantages. Unlike methadone, which requires daily visits to specialized clinics, Suboxone can be prescribed in a regular doctor’s office. This allows you to receive treatment in your community, possibly from your regular doctor.
Understanding the Side Effects
While Suboxone is well-tolerated, knowing potential side effects helps you know what to expect.
Common side effects may occur in the first few weeks. Headaches and nausea are frequent but often improve. Constipation can be managed with diet, water, or over-the-counter remedies. Some people experience insomnia, increased sweating, or temporary mouth numbness.
More serious side effects are less common but require attention. Liver problems can occur, so your doctor may order blood tests. Warning signs include yellowing skin or eyes, dark urine, or persistent fatigue.
Dental decay has gained more attention recently. The acidity of sublingual buprenorphine can damage tooth enamel, so proper oral hygiene is important. While a lesser concern than active addiction, good dental health is part of overall recovery.
Allergic reactions are rare but can be serious. Seek medical attention for a rash, hives, or difficulty breathing. While Suboxone has a low risk of severe breathing problems, this risk increases significantly when combined with alcohol, benzodiazepines, or other sedatives.
For most, the benefits of Suboxone for opioid addiction far outweigh the risks. Side effects are manageable, whereas untreated addiction can be fatal. Your healthcare provider can help you weigh these factors and minimize any side effects.
Not everyone experiences side effects. Many find them minor compared to the distress of active addiction.
The Suboxone Treatment Journey
Starting Suboxone for opioid addiction is a planned journey that begins with finding the right provider and a personalized treatment plan. The path can feel overwhelming, but each step is designed for your safety and success. The right support makes all the difference.
How Suboxone is Prescribed and Administered
Your first appointment involves an initial assessment to gather information for a safe, effective treatment plan. Your provider will review your medical history, conduct an exam, and discuss your goals.
The induction phase requires precise timing. You must be in moderate withdrawal before your first dose to avoid precipitated withdrawal, an extremely uncomfortable reaction caused by taking Suboxone too soon after other opioids.
Your doctor will use the Clinical Opiate Withdrawal Scale (COWS) to assess your symptoms. For short-acting opioids like heroin or fentanyl, you’ll wait 12-24 hours after your last use. For long-acting opioids like methadone, the wait is 48-72 hours or longer.
You’ll start with a low dose (2mg or 4mg) and increase it gradually until withdrawal symptoms are managed.
Suboxone comes as a sublingual film or tablet. Place it under your tongue or in your cheek and let it dissolve completely. Do not chew, swallow, or cut it, and avoid food or drink until it’s dissolved for proper absorption.
In the maintenance phase, your doctor will find your optimal daily dose, typically 8mg to 16mg (up to 24mg for some). The goal is to eliminate cravings and withdrawal, block other opioids, and allow you to focus on recovery.
Tapering down is an option when you and your doctor agree. It requires medical supervision and a gradual schedule to minimize withdrawal and relapse risk. Never stop Suboxone abruptly.
The Crucial Role of Counseling and Support
While Suboxone for opioid addiction manages the physical side, true recovery involves more. The best outcomes occur when medication is part of a broader support system.
Behavioral therapy and counseling help you develop coping strategies and address underlying issues. Support groups like Narcotics Anonymous or SMART Recovery offer connection with peers who understand your experience, providing encouragement and accountability.
Addressing co-occurring disorders like depression or anxiety alongside addiction treatment improves your chances of success.
Important: While combining medication and therapy is ideal, medication alone is proven effective. If you can only access medication, that is still valid, life-saving care. Don’t let perfect be the enemy of good.
At Addiction Helpline America, we believe in comprehensive support. We can connect you with resources that address all aspects of recovery through our Addiction Helpline America resources.
Is Suboxone for Opioid Addiction a Long-Term Solution?
A common question is: “How long will I need Suboxone?” The answer is: it depends on you.
Treatment duration is highly individualized based on your needs, response to treatment, and personal goals. Some use it for months, others for years or indefinitely.
We approach opioid use disorder as a chronic medical condition. Like insulin for diabetes, some people benefit from long-term Suboxone maintenance to prevent relapse and maintain stability.
There’s no scientific evidence supporting short-term-only treatment. Research shows that longer treatment durations lead to better outcomes. The focus should be on sustained recovery, not arbitrary time limits.
When you and your provider decide to taper, it will be a slow, medically supervised process to prevent withdrawal and relapse. There is no pressure to rush this.
For more detailed information, you can read our expert guidance on Suboxone treatment duration.
Your recovery journey is unique. What matters is finding an approach that helps you reclaim your life and well-being.
Addressing Misconceptions and Setting Expectations
If you’re considering Suboxone for opioid addiction, you’ve likely encountered myths. These misconceptions create barriers to care. Let’s set the record straight with facts.
Many myths stem from outdated, abstinence-only views of recovery. We now understand addiction is a medical condition that often requires medical treatment, like diabetes or heart disease.
Common Myths About Suboxone
Myth: “You’re just trading one addiction for another.” This is the most harmful misconception. When prescribed, Suboxone doesn’t cause a high. It stabilizes brain chemistry, allowing for clear thinking and healthy choices. Think of it like insulin for diabetes—it’s medicine for a medical condition.
Myth: “You aren’t really in recovery if you’re on Suboxone.” This outdated thinking is harmful. Recovery is personal. What matters is that you’re no longer using illicit drugs and are rebuilding your life. People on Suboxone return to work, repair relationships, and become engaged parents and community members. That is recovery.
Myth: “Suboxone must be combined with therapy to be effective.” While combining medication and therapy is ideal, research shows Suboxone alone is effective and saves lives. Access to therapy can be difficult. Don’t let the perfect be the enemy of the good; medication is a huge step forward.
Myth: “Suboxone should only be used for a short time.” No scientific evidence supports short-term-only use. Studies show longer treatment leads to better outcomes. Treatment can last months, years, or be indefinite, based on your needs and your doctor’s advice.
Myth: “It’s as easy to overdose on Suboxone as other opioids.” This misinformation is dangerous. Suboxone’s “ceiling effect” makes it very difficult to overdose on it alone. While it shouldn’t be mixed with sedatives like alcohol or benzodiazepines, its safety profile is excellent compared to the risk of street drugs like fentanyl.
These myths persist due to stigma and ideological interests. At Addiction Helpline America, we’ve seen medication-assisted treatment work. The evidence is clear: Suboxone for opioid addiction is effective.
If you’re ready to move past the myths, we’re here to help you find qualified providers. For a deeper dive, check out this resource on Debunking 5 Suboxone myths.
Frequently Asked Questions about Suboxone Treatment
It’s natural to have questions about Suboxone for opioid addiction. Here are answers to some common concerns about the practical details of treatment.
How much does Suboxone cost and is it covered by insurance?
Suboxone for opioid addiction treatment is more affordable and accessible now, but costs vary.
- Cost: Without insurance, the medication can cost $300-$450 per month, depending on brand vs. generic, dosage, and pharmacy.
- Generics: Since 2018, FDA-approved generics have provided a more affordable option. They work just as effectively as brand-name versions for a lower cost.
- Insurance: Most health insurance plans, including Medicaid and Medicare, cover Suboxone. However, details like co-pays, deductibles, and prior authorization vary. Call your insurance company to understand your specific benefits.
- Parity Laws: The Mental Health Parity and Addiction Equity Act of 2008 requires most plans to cover substance use disorders like other medical conditions, making treatment more accessible.
What are the considerations for pregnant women?
Pregnancy with opioid addiction is scary, but effective treatment is available. Treatment is far safer for you and your baby than continued illicit opioid use.
- Gold Standard:Buprenorphine is a first-line treatment during pregnancy. Untreated addiction risks miscarriage, premature birth, and stillbirth, making medication crucial for the health of both mother and baby.
- Prescription: Some providers prescribe buprenorphine alone (Subutex) during pregnancy to minimize naloxone exposure, though combination products are also considered safe. Your healthcare team will determine the best option for you.
- Reduced Risks: Buprenorphine treatment protects you from overdose, infections, and unpredictable street drugs, creating a safer environment for your baby.
- NOWS: Babies born to mothers on buprenorphine may experience Neonatal Opioid Withdrawal Syndrome (NOWS), but it is well-understood and treatable. Symptoms are often milder than with methadone or street opioids, and hospital staff are experienced in managing it.
How do I find Suboxone treatment near me?
Finding a provider for Suboxone for opioid addiction is easier than ever. Here’s how to connect with care:
- Your Doctor: Your primary care physician is a good starting point. They can either prescribe it or refer you to someone who does.
- Treatment Locators: The Substance Abuse and Mental Health Services Administration (SAMHSA) has online treatment locators to find qualified providers in your area.
- Addiction Helpline America: Connecting people with treatment is what we do. We work with a nationwide network of providers and can help you find one that fits your needs, location, and insurance. Our guidance is free and confidential. Find Suboxone treatment with Addiction Helpline America to get started.
- Telehealth: Telehealth has expanded access to buprenorphine, especially for those in rural areas or with transportation issues. You may be able to meet a provider and get a prescription virtually.
Taking this step is brave. You deserve support, and effective help is available.
Take the First Step Toward Recovery
Recovery from opioid addiction is happening every day. Suboxone for opioid addiction is a genuine lifeline, offering hope where there seemed to be none.
The journey from addiction to recovery can feel overwhelming. Many feel trapped in a cycle of cravings and relapse. But we’ve learned that with the right medical care and support, recovery is not only possible, it’s probable.
Suboxone is a life-saving tool that does more than manage withdrawal. It provides the stability to rebuild your life, work, and relationships. It reduces overdose risk and gives your brain a chance to heal, supporting long-term recovery.
Hope is within reach. Taking the first step by calling is crucial. We’re struck by how quickly things can turn around with the right treatment. People who felt hopeless begin planning for the future.
At Addiction Helpline America, we know no one should steer recovery alone. We provide personalized, confidential guidance based on your needs, insurance, and location. Finding the right provider can be hard, so we’ve built a nationwide network of trusted treatment centers to simplify the process.
Whether you’ve tried to quit before or this is your first time seeking help, you deserve compassionate support from people who understand.
Your story doesn’t have to end with addiction. Reaching out for help can be the start of a new chapter. Take that first step toward freedom from opioid addiction today, and let us help you find the right recovery program for you.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.