Your First Step to Recovery: An Introduction to Suboxone Treatment
If you’re looking for a suboxone clinic near me, here’s what you need to know right now:
How to Find a Suboxone Clinic:
- Use the SAMHSA Buprenorphine Practitioner Locator at samhsa.gov (free, government-run directory)
- Call the SAMHSA National Helpline at 1-800-662-4357 (free, confidential, 24/7)
- Search FindTreatment.gov and filter by “Medication Therapy” and your location
- Contact your insurance provider for in-network clinics
- Ask your primary care doctor for a referral
What You’ll Get:
- Same-day or next-day appointments at many clinics
- Medicaid or private insurance-covered consultations (in most cases)
- Take-home medication after stabilization
- Virtual/online options available
Opioid addiction can feel like a prison, but medication-assisted treatment (MAT) with Suboxone offers real hope for recovery. Suboxone is a prescription medication combining buprenorphine and naloxone to reduce cravings and ease withdrawal symptoms without producing an intense high. It works like a reset button for your brain chemistry, quieting the noise of addiction while you rebuild your life.
This guide will walk you through finding a nearby Suboxone clinic, understanding how treatment works, and taking the first steps toward recovery. You’ll learn what to expect, how to compare options, and how to access care quickly.
At Addiction Helpline America, we’ve helped thousands find recovery from opioid addiction by connecting them with quality Suboxone clinics nationwide. We understand that reaching out is the hardest step, which is why we provide clear, judgment-free guidance.
Recovery is possible. Let’s get started.
Understanding Suboxone: How It Works and If It’s Right for You
Suboxone has helped hundreds of thousands of people reclaim their lives from opioid addiction. It’s not a magic cure, but it is a powerful tool that can give you the breathing room you need to start healing.
What is Suboxone and How Does It Work?
Suboxone is a prescription medication designed to treat opioid use disorder (OUD). It’s for people who use heroin, fentanyl, or other opioids and want to stop. Its unique formula contains two ingredients: buprenorphine and naloxone.
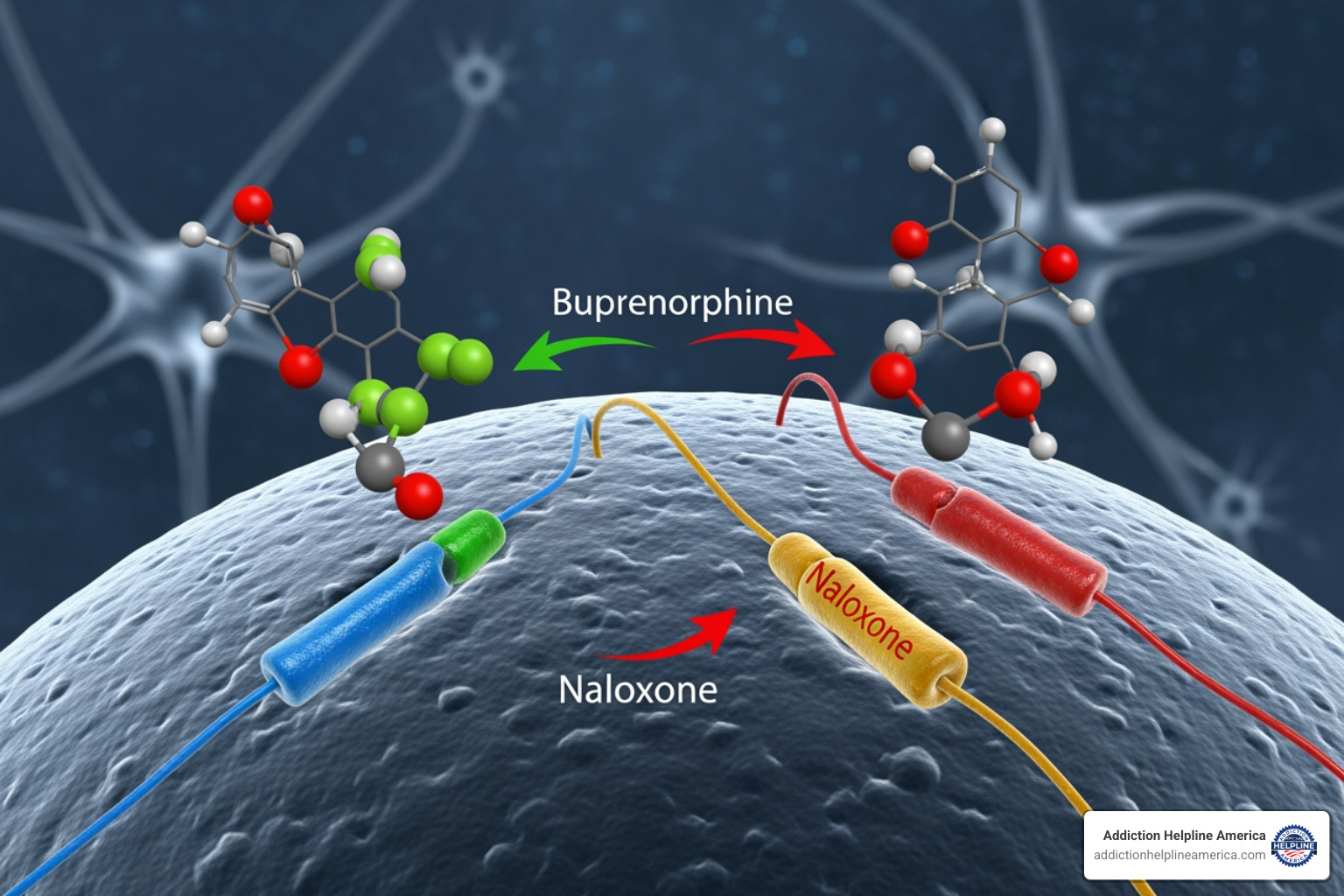
Buprenorphine is a partial opioid agonist. It activates your brain’s opioid receptors just enough to stop withdrawal symptoms and cravings, but not enough to get you high. It’s like turning down the volume on the addiction, allowing you to feel normal and stable. This “reset button” effect helps your brain chemistry stabilize, making the first difficult weeks of recovery manageable.
Naloxone is an opioid antagonist that acts as a safety mechanism. When you take Suboxone as prescribed (dissolving it under your tongue), the naloxone has little effect. However, if someone tries to inject it to get high, the naloxone activates, blocks the opioid effects, and triggers immediate withdrawal. This built-in safeguard discourages misuse and is a key reason many clinics prefer it.
Is Suboxone Therapy Right for You?
Only you and a qualified medical professional can answer this question, but if opioids have taken over your life and you’ve struggled to quit, Suboxone could be the missing piece.
A medical assessment is the essential first step. A provider will review your health and opioid use history to confirm an opioid use disorder (OUD) diagnosis. This evaluation will likely include a urine screening and other lab work to ensure Suboxone is safe for you. It’s crucial to be honest about your health and any other substances you use.
You don’t have to figure this out alone. At Addiction Helpline America, we connect people with compassionate providers who understand addiction as a medical condition. Finding the right clinic starts with a single phone call. Our team will listen and help you connect with a provider who can determine if Suboxone is right for your recovery journey.
The Suboxone Treatment Journey: What to Expect
Starting Suboxone treatment follows a roadmap with three phases: induction, stabilization, and maintenance. Understanding each stage can reduce anxiety about the journey ahead.
The Three Phases of Suboxone Treatment
1. Induction Phase: This is when you take your first dose under medical supervision. It’s crucial to be in mild to moderate withdrawal (usually 12-24 hours after your last opioid use) to avoid “precipitated withdrawal.” Your doctor will use a tool like the Clinical Opiate Withdrawal Scale (COWS) to find the right time. During this phase, which lasts a few days to a week, your team will monitor you and adjust your dosage to control cravings and ensure comfort.
2. Stabilization Phase: Here, your physician finds your optimal Suboxone dose—the “sweet spot” that keeps you free from cravings and withdrawal. Most people reach a stable dose within a week. During this time, you’ll also begin rebuilding routines and addressing the underlying causes of addiction.
3. Maintenance Phase: You’ll continue taking a steady dose of Suboxone while receiving ongoing support through regular appointments with your clinic. This phase provides the stability needed to focus on therapy, develop coping skills, and repair your life. Think of it as scaffolding that supports you while you rebuild.
Your First Appointment and Treatment Plan
Your first visit is an assessment. A physician will discuss your medical and opioid use history, support system, and recovery goals. Honesty is vital for your safety. You’ll likely provide a urine sample and may have other lab work done. Based on this, your provider will create a personalized treatment plan, explaining how Suboxone works and the follow-up schedule. Many clinics offer same-day or next-day appointments, so you can start quickly.
How Long Will I Need to Be on Suboxone Treatment?
Opioid use disorder is a chronic condition, so treatment duration varies. Some people use Suboxone for months, while others need it for years. Research shows that staying in treatment for at least one year significantly increases the likelihood of success. This isn’t a sign of weakness; it’s about giving your brain and life time to heal.
The decision to taper off Suboxone should always be made with your doctor once you have achieved long-term stability. They will assess your readiness by considering your coping skills, support systems, and overall mental and physical health. A helpful resource for understanding this is this guide from CAMH (see Chapter 8). The goal isn’t to rush off medication; it’s to build a life worth living.
Comparing Your Treatment Options
When you’re ready for recovery, you have several paths to consider. Let’s walk through your options so you can make the best choice for you.
Benefits of Suboxone Treatment
If you’re looking for Suboxone treatment, you’re on the right track. Suboxone is a leading treatment because it tackles the two biggest obstacles to recovery: withdrawal symptoms and cravings. This allows you to focus on rebuilding your life instead of just surviving each day.
Key advantages include:
- Convenience: After stabilization, you can take Suboxone at home, allowing your recovery to fit into your life, not the other way around.
- Safety: The main ingredient, buprenorphine, has a “ceiling effect,” which dramatically reduces overdose risk compared to other opioids. The addition of naloxone also deters misuse.
- Long-Term Support: Suboxone provides the stability needed to engage in therapy, repair relationships, and find yourself again beyond addiction.
Suboxone vs. Other Medication-Assisted Options
While Suboxone is effective, it’s helpful to see how it compares to methadone, another common MAT medication. The main difference is how they work. Suboxone is a partial opioid agonist, while methadone is a full opioid agonist. This affects safety and daily routines.
| Feature | Suboxone (Buprenorphine/Naloxone) | Methadone |
|---|---|---|
| Mechanism | Partial opioid agonist (buprenorphine) plus opioid antagonist (naloxone). Partially activates receptors to reduce cravings and withdrawal. | Full opioid agonist. Fully activates opioid receptors. |
| Safety Profile | Ceiling effect reduces overdose risk. Naloxone deters injection misuse by causing withdrawal. | Higher overdose risk without ceiling effect. Requires careful dose monitoring. |
| Clinic Visit Frequency | Initial frequent visits, then often weekly or monthly with take-home doses. | Typically requires daily clinic visits, especially early in treatment. Take-homes earned over time. |
| Stabilization Time | Often within 7 days or less. | Usually around 2 weeks. |
| Administration | Sublingual film or tablet taken at home once daily (after stabilization). Monthly injectable form (Sublocade) also available. | Oral liquid taken once daily, usually dispensed at clinic. |
| Drug Interactions | Dangerous when combined with alcohol, benzodiazepines, and other CNS depressants. | Dangerous when combined with alcohol, opioids, cocaine, barbiturates, benzodiazepines, and tranquilizers. |
| Common Side Effects | Constipation, headaches, nausea, hypogonadism. | Constipation, sweating, sedation, sexual dysfunction, hypogonadism. |
| Pregnancy Considerations | Buprenorphine alone may reduce risk of neonatal abstinence syndrome. Requires detailed discussion with healthcare provider. | Used safely for decades in pregnancy. Prevents dangerous opioid withdrawal. NAS risk remains. |
Is Online Suboxone Treatment Effective?
Yes, online Suboxone treatment is just as effective as in-person care. Telemedicine has removed major barriers to treatment, such as transportation, time off work, and privacy concerns.
Through secure video consultations, you can connect with licensed physicians, often receiving a same-day prescription sent to your local pharmacy. This convenience and confidentiality help many people stick with treatment longer, which is a key factor in successful recovery. At Addiction Helpline America, our network includes physicians who provide high-quality online care, delivering thorough assessments and personalized plans directly to you.
Once stabilized, you can typically take your medication at home, with a once-daily sublingual film or tablet. For those who prefer not to manage daily dosing, Sublocade, a once-monthly injection administered by your provider, is also an option. This flexibility allows you to manage your recovery independently while receiving medical oversight, building confidence for the long term.
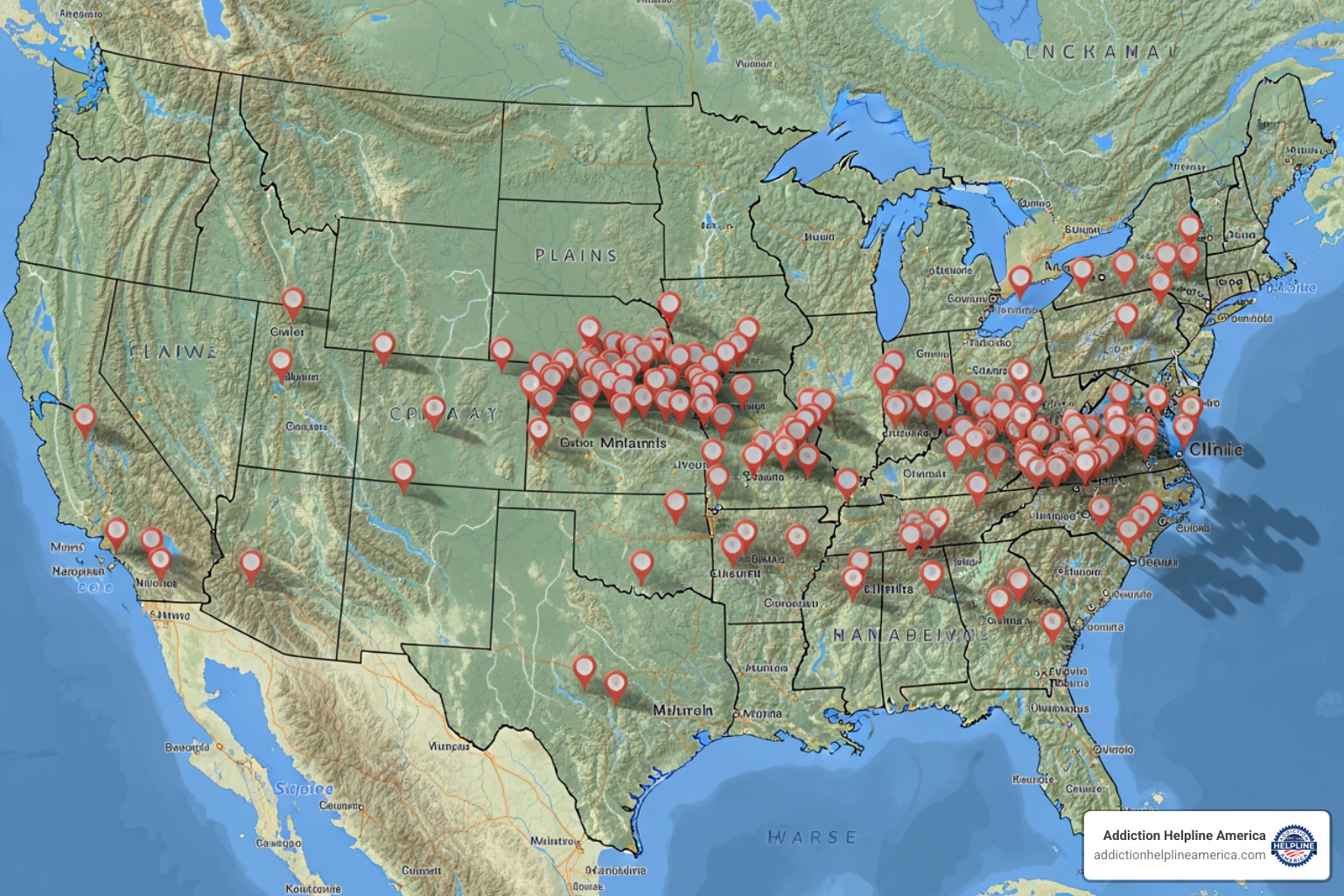
How to Find a Suboxone Clinic Near Me
Finding the right clinic is a crucial step. With the right resources, you can quickly connect with quality treatment that fits your life.
Using Trusted Resources to Find a Suboxone Clinic Near Me
The most reliable way to locate a clinic is through official, government-backed directories. These resources are free, confidential, and regularly updated.
- SAMHSA Buprenorphine Practitioner Locator: Found at samhsa.gov, this tool helps you find local practitioners authorized to treat opioid dependency with buprenorphine.
- SAMHSA Opioid Treatment Program Directory: Located at dpt2.samhsa.gov/treatment/, this directory provides a comprehensive list of accredited programs by state.
- FindTreatment.gov: This is SAMHSA’s anonymous search tool for all substance use and mental health facilities. Use the filters to narrow your search by “Medication Therapy” to find clinics offering Suboxone.
When using these directories, filter your search by distance, type of care, and payment options to find the best fit. Always call the clinic directly to confirm they are accepting new patients for Suboxone treatment and to ask about appointment availability. Many clinics have eliminated waitlists and offer same-day or next-day appointments.
If you need help navigating these options or understanding insurance, Addiction Helpline America can guide you to providers who are ready to help.
Questions to Ask a Potential Suboxone Clinic Near Me
When you call a potential clinic, asking the right questions helps you determine if it’s a good match. Good clinics welcome your questions.
- “Are you accepting new patients for Suboxone treatment?” Confirms they have immediate availability.
- “What does a typical treatment plan include?” Listen for mentions of induction, stabilization, maintenance, and counseling.
- “Will my insurance cover treatment?” Verify your specific coverage for consultations and medication.
- “What role does counseling play in your program?” The most effective programs integrate medication with behavioral therapies like CBT.
- “What are your policies on take-home doses and urine screenings?” Understand the program’s expectations from the start.
- “How quickly can I start treatment?” Many modern clinics offer access within 24-48 hours.
- “Do you offer online or telehealth options?” Virtual treatment is a convenient and confidential option that is just as effective as in-person care.
Key Aspects of Your Suboxone Program
Once you’ve found a nearby clinic, it’s helpful to understand the practical details of treatment, including costs, side effects, and the role of counseling.
Will My Insurance Cover Suboxone Treatment?
Money worries shouldn’t be a barrier to recovery. Many insurance plans, including Medicaid and private insurance, cover Suboxone treatment. However, coverage varies, so it’s important to verify your specific benefits.
- Contact your insurance provider: Call the number on your card and ask about coverage for “Medication-Assisted Treatment (MAT)” for opioid use disorder.
- Talk to the clinic’s staff: They can often help you verify your insurance and understand any out-of-pocket costs.
- Explore assistance programs: If you’re uninsured, state and federal programs can help cover the cost of treatment.
At Addiction Helpline America, we can help you steer insurance questions and find affordable treatment options.
What are the Potential Side Effects of Suboxone?
Suboxone is generally well-tolerated, but some side effects can occur. Most are manageable.
- Constipation: This is the most common side effect. Manage it by increasing fiber and water intake and staying active. Your doctor can recommend stool softeners if needed.
- Headaches and Nausea: These often occur early in treatment and usually improve as your body adjusts. Check with your doctor before taking any over-the-counter pain relievers.
- Other Side Effects: Less common effects include sweating or dizziness. Long-term use may lead to hypogonadism (reduced hormone levels); talk to your doctor if you experience decreased energy, mood changes, or low libido.
Warning: Mixing Suboxone with other central nervous system depressants like alcohol, benzodiazepines, or other opioids can be fatal. Be completely honest with your doctor about all substances you use for your safety.
The Vital Role of Counseling in Suboxone Treatment
Suboxone is a powerful tool, but it works best when combined with counseling and behavioral therapy. Medication addresses the physical dependence, giving you the stability to work on the psychological and behavioral aspects of addiction.
Counseling helps you:
- Address underlying issues like trauma or co-occurring mental health conditions.
- Develop healthy coping skills to handle stress and triggers without turning to substances.
- Change negative thought patterns through therapies like Cognitive-Behavioral Therapy (CBT).
Support groups like Narcotics Anonymous (NA) or SMART Recovery also provide a valuable sense of community and peer support.
Are There Any Support Groups or Additional Resources Available?
Recovery is not a journey you have to take alone. In addition to your treatment team, a network of support is available.
- Co-occurring Disorder Treatment: Many people with OUD also have depression, anxiety, or PTSD. Integrated treatment is crucial for overall recovery.
- Naloxone Kits (Narcan): These kits can reverse an opioid overdose and save a life. They are often available for free from clinics and community organizations.
If you or someone you know needs immediate help, these resources are available 24/7:
- 988 Suicide & Crisis Lifeline: Dial 988 for any mental health or substance use crisis.
- Veterans Crisis Line: Confidential support for veterans via phone, chat, or text.
- SAMHSA National Helpline: Call 1-800-662-HELP (4357) for free, confidential treatment referral and information.
Take the Next Step Towards a Healthier Future
Finding a nearby Suboxone clinic is the first step toward a healthier future. If you’re struggling with opioid use disorder, know that recovery is possible and happens for people just like you every day.
Suboxone is a proven tool that provides the stability to break free from addiction. It quiets cravings and eases withdrawal, giving you the space to engage in counseling, rebuild relationships, and reconnect with your life. But it’s most powerful when combined with professional guidance and support.
That’s where we come in. At Addiction Helpline America, we make the next steps simple and supportive. We provide free, confidential, and personalized guidance to connect you with the right treatment program from our vast network of centers across the country.
You don’t have to do this alone. Your journey to recovery begins with a single step. Reach out today—let us help you find the support, care, and hope you deserve.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.