
When someone’s life has been upended by severe Post-Traumatic Stress Disorder, PTSD inpatient treatment offers a structured, 24/7 therapeutic environment to begin healing. It’s an immersive program inside a residential facility, specifically designed to help people with debilitating symptoms find stability and start their recovery journey, away from the triggers and stressors of the outside world.
What PTSD Inpatient Treatment Really Means
It’s helpful to think of PTSD inpatient treatment less like a hospital stay and more like a dedicated healing sanctuary. This is an intensive, live-in program that intentionally removes you from the daily environment where your trauma symptoms are most likely to flare up. It gives you the space to pour all your energy into recovery, free from the constant pressures of work, family, and other obligations.
The need for this level of care is significant. The World Health Organization estimates that while 70% of people will go through a traumatic event in their lifetime, about 5.6% will develop PTSD. This statistic, further explored in global market analysis from Grandview Research, underscores just how many people are searching for effective solutions.
Here’s an analogy: if you shatter your leg, you wouldn’t keep trying to walk on it. You’d get a cast and let it rest completely so the bone could mend. Inpatient treatment acts as that “cast” for the mind. It provides the essential safety, structure, and expert guidance needed for deep psychological healing to finally begin.
When to Consider Inpatient Care
Making the choice to enter a PTSD inpatient treatment program is a major one. It’s often a step taken when other, less intensive forms of care haven’t been enough to turn the tide. Inpatient care is generally recommended when PTSD symptoms become so severe that they fundamentally disrupt your life, making it nearly impossible to function at work, at school, or even within your own family.
Key signs that inpatient care might be the right path include:
- Constant Daily Struggles: When symptoms like relentless hypervigilance, crushing anxiety, or disorienting flashbacks make even simple daily tasks feel like monumental efforts.
- Risk to Yourself or Others: If you’re having thoughts of self-harm or suicide, or are experiencing aggressive outbursts that could be dangerous. The 24/7 supervision of a residential facility is a critical safety net in these situations.
- Outpatient Efforts Aren’t Working: You’ve been diligent with outpatient therapy, medication, or support groups, but your symptoms are staying the same or even getting worse.
- Complex, Co-Occurring Conditions: When PTSD is intertwined with other serious challenges like a substance use disorder (addiction), severe depression, or an eating disorder. Inpatient programs are specifically designed to provide integrated treatment for these dual diagnoses at the same time.
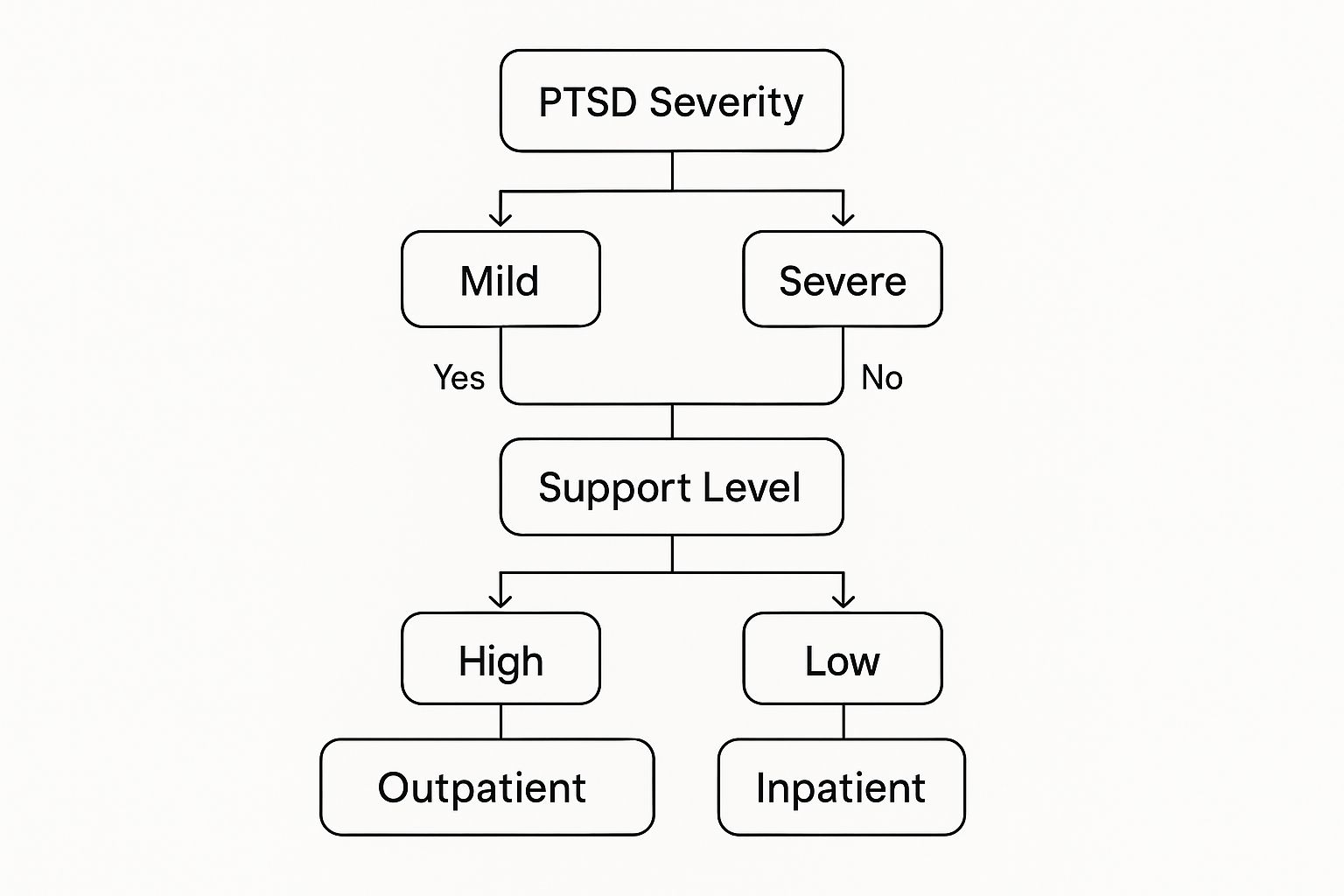
The image above helps visualize this decision. As the severity of PTSD symptoms climbs and a person’s support system at home dwindles, the recommendation for inpatient care becomes much stronger to ensure both safety and effective treatment.
Deciding between inpatient and outpatient care can be confusing. The table below breaks down the key factors that usually guide this important choice.
When to Consider Inpatient vs Outpatient PTSD Care
| Factor | Outpatient Care May Be Suitable | Inpatient Care Is Often Recommended |
|---|---|---|
| Symptom Severity | Symptoms are manageable; you can still function in daily life, though with difficulty. | Symptoms are severe, debilitating, and prevent normal daily functioning (work, school, self-care). |
| Safety Risks | No immediate risk of self-harm, suicide, or harm to others. | Presence of suicidal thoughts, self-harming behaviors, or aggression; immediate safety is a concern. |
| Life Stability | You have a stable, supportive home environment and a strong social support system. | Home environment is stressful, triggering, or lacks adequate support for recovery. |
| Co-occurring Issues | Any co-occurring conditions (like mild depression) are stable and being managed. | Dealing with complex, co-occurring disorders like active substance addiction or severe depression that require integrated care. |
| Previous Treatment | You are new to treatment or have had some success with less intensive therapies. | Previous attempts at outpatient therapy have not been effective or symptoms have worsened. |
Ultimately, the choice depends on your unique situation, but this comparison can help clarify which level of care might align best with your current needs.
A Sanctuary for Focused Healing
The greatest strength of residential care is its immersive design. By physically stepping away from the people, places, and situations that trigger your trauma responses, you give yourself the mental and emotional space required for profound therapeutic work.
“Inpatient treatment provides a unique opportunity to build a new foundation for life. It’s not just about managing symptoms; it’s about fundamentally rewiring your response to trauma in an environment built entirely around safety, support, and healing.”
This controlled setting is where the real work happens. Therapists can use intensive, evidence-based treatments much more frequently and with greater focus than is ever possible in a weekly outpatient appointment. You’re also surrounded by a community of peers who truly get what you’re going through and a clinical team providing round-the-clock medical and emotional support.
This powerful combination of structure, safety, and intensive therapy is what makes PTSD inpatient treatment a life-changing option for those who need it most, creating a solid launchpad for a lasting recovery.
The Core Therapies Driving Your Recovery

The real work of healing in PTSD inpatient treatment happens through a structured schedule of evidence-based therapies. In a residential facility, you aren’t just getting a single therapy session once a week. Instead, you’re immersed in intensive, daily work designed to get to the root of the trauma. The safe, supportive environment allows therapists to use these powerful methods with a consistency and depth that’s simply not achievable in outpatient care.
Think of it like physical rehabilitation after a major injury. Outpatient care might be a few physical therapy sessions a week. Inpatient treatment is like being at a specialized rehab center where therapists, doctors, and trainers work with you around the clock, creating a focused, integrated plan to rebuild your strength. That’s the level of intensity that fosters deep, lasting recovery from PTSD.
Rewriting the Stories Trauma Tells
A major focus of treatment is a family of therapies known as Trauma-Focused Cognitive Behavioral Therapy (TF-CBT). This isn’t just one technique; it’s a whole toolbox designed to help you find, challenge, and change the painful, distorted thoughts that trauma leaves behind.
Within this toolbox, you’ll likely encounter Cognitive Processing Therapy (CPT). Trauma can force you to write a story about yourself and the world that’s full of fear, shame, and blame. CPT is like sitting down with a compassionate editor who helps you go through that story line by line. Together with your therapist, you’ll find the parts that are no longer true and work on rewriting a new narrative—one that’s based on your strength, resilience, and a more accurate view of the past.
The goal isn’t to forget what happened. It’s to change how you think about it, which in turn changes how you feel, stripping the traumatic memories of their power to control your daily life.
Safely Confronting Painful Memories
Another vital part of treatment is exposure-based therapy. This can sound scary, but in an inpatient center, it’s done in a completely safe, gradual, and supportive way. The fundamental idea is to gently and repeatedly reduce the intense fear and anxiety that have become linked to your traumatic memories.
Two of the most trusted and effective forms are:
- Prolonged Exposure (PE): This therapy has two parts. You’ll carefully recount the traumatic event with your therapist in a safe setting, and you’ll also gradually start approaching the people, places, or activities you’ve been avoiding out of fear. By facing these things in a controlled way, you teach your brain that they are no longer dangerous, and the fear response naturally subsides.
- Virtual Reality (VR) Exposure Therapy: For certain traumas, like combat experiences or serious accidents, VR technology offers a unique solution. It can create an incredibly realistic simulation of the traumatic scene, allowing you to confront it in a setting that is 100% safe and controlled by your therapist.
“These aren’t just theories; they get real-world results. Inpatient programs using therapies like Prolonged Exposure (PE) and Cognitive Processing Therapy (CPT) see significant improvements. In fact, their use has been connected to a 23% reduction in suicide risk among veterans with PTSD, as highlighted in a detailed market report you can explore.”
Reprocessing Trauma with EMDR
Eye Movement Desensitization and Reprocessing (EMDR) is another key therapy used in PTSD inpatient treatment. It’s a unique method that helps your brain effectively process traumatic memories that have become “stuck,” blocking your natural ability to heal. In an EMDR session, you’ll focus on a specific memory while following a light or sound that moves back and forth.
A good way to understand it is to think of a traumatic memory as a corrupted computer file. Instead of being properly saved in the “past events” folder, it keeps popping up on your desktop, making you feel like it’s happening right now. EMDR acts like a repair tool, helping your brain properly file the memory away. The memory is still there, but it no longer carries the same intense emotional distress.
By weaving these different therapies together, an inpatient program addresses trauma from all angles—from your thoughts and beliefs to your body’s physical responses. This comprehensive strategy is what helps you move beyond just coping with symptoms to truly healing the wound at its core.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
What a Typical Day in Treatment Looks Like

One of the biggest hurdles to seeking help for PTSD is the fear of the unknown. What actually happens behind the doors of an inpatient center? It helps to know that the daily schedule isn’t just a rigid timetable; it’s a rhythm for healing, intentionally designed to create structure and safety.
When PTSD makes life feel chaotic and unpredictable, a predictable routine can be incredibly grounding. A typical day isn’t about just passing time—it’s about actively rebuilding your sense of safety and self, piece by piece.
A Structured Morning for Stability
Your day will likely start early with a gentle wake-up call and a nutritious breakfast. This simple act of starting the day on a schedule helps regulate sleep and metabolism, two things often thrown into disarray by trauma. Mornings are typically reserved for the most intensive therapeutic work when your mind is at its sharpest.
Individual Therapy: This is your dedicated, one-on-one time with a therapist. Here is where the deep work happens—processing traumatic memories using proven methods like EMDR or CPT and building coping skills tailored specifically to you. It’s a confidential space that serves as the foundation of your treatment.
Specialized Group Therapy: Following your individual session, you’ll usually join a small group. These aren’t just general chat sessions; they are focused on specific challenges tied to PTSD. You might discuss practical ways to manage hypervigilance, work on rebuilding trust, or navigate the complex feelings of guilt and shame that so often accompany trauma.
These morning sessions really set the tone. Hearing from others who get it is profoundly validating. It starts to break down the wall of isolation that trauma builds, reminding you that you are not alone.
Afternoon Focus on Skills and Connection
After lunch, the focus often shifts from deep emotional processing to building practical skills and reconnecting with your body. The goal is to give you real-world tools for life after treatment while helping you feel at home in your own skin again.
“A day in residential care is a microcosm of recovery. It combines deep psychological work with practical skill development and physical wellness, creating a balanced approach that addresses the mind, body, and spirit in unison.”
You’ll take part in a variety of activities designed to address different parts of your well-being:
Educational Workshops: Think of these as classes on the science of healing. You’ll learn about the neuroscience of PTSD, how triggers work, and powerful grounding techniques you can use to manage a flashback or a panic attack the moment it starts.
Holistic and Experiential Therapies: Trauma creates a disconnect between the mind and body. These therapies help bridge that gap. Activities like yoga, meditation, art therapy, or even equine therapy offer powerful, non-verbal ways to process feelings and release the physical tension PTSD holds in the body.
This combination of learning and doing is essential. It’s one thing to talk about managing anxiety; it’s another to actually feel your body calm down during a guided meditation. To get a broader sense of the entire inpatient experience, you can learn more about what to expect in rehab in our detailed guide.
Evening for Reflection and Community
Evenings are for winding down, reflecting on what you’ve learned, and connecting with peers in a more relaxed way. Dinner is usually a communal meal, which helps foster a sense of family and belonging that is so vital to healing.
After dinner, there might be a final, low-key group meeting—perhaps a 12-step meeting if you’re also dealing with substance use, or just a simple check-in to share what you’re taking away from the day. You’ll also have scheduled free time for journaling, reading, or just having a quiet chat with others. This structured downtime is crucial for letting the day’s lessons sink in and preparing for a restful night’s sleep, completing a full cycle dedicated to your recovery.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Why an Immersive Environment Is So Powerful
So, why would someone choose an inpatient setting to recover from PTSD? While seeing a therapist on an outpatient basis can be incredibly helpful, you’re still trying to heal while navigating the daily minefield of triggers and stressors that keep the symptoms alive. PTSD inpatient treatment offers something completely different: a dedicated, immersive environment where your healing is the one and only focus.
Think of it like this: trying to heal from PTSD while living your normal life is like trying to fix a badly broken leg while still walking on it. You might make a tiny bit of progress, but the constant pressure prevents the bone from ever truly setting and healing properly. Inpatient care is the equivalent of getting a proper cast and a set of crutches. It removes the “weight” of everything else—work deadlines, family tensions, environmental triggers—so the deep, structural work of recovery can finally happen without constant interruption.
A True Sanctuary from Triggers and Stress
The most immediate and powerful benefit of a residential program is the physical and emotional space it creates between you and your daily life. For many with PTSD, their own home, neighborhood, or even workplace can start to feel unsafe or hostile. The constant state of high alert and the sheer exhaustion it takes to get through the day drains the very energy you need to get better.
An inpatient facility provides a genuine sanctuary. It’s a controlled, safe space where your nervous system can finally stand down from its constant state of “fight or flight.” This feeling of safety isn’t just a nice-to-have; it’s an absolute requirement for effective therapy. It’s only when the mind and body feel fundamentally secure that you can begin to approach the difficult memories and emotions at the heart of the trauma.
“The 24/7 nature of inpatient care provides a crucial safety net. It means that support isn’t just an appointment on a calendar; it’s a constant presence. Whether a nightmare strikes at 3 a.m. or a wave of anxiety hits during a meal, skilled medical and emotional support is always on hand to help you through it.”
This round-the-clock supervision is especially critical for anyone dealing with severe symptoms, like intense flashbacks, thoughts of self-harm, or overwhelming panic. It ensures that help is there in the moment it’s needed, preventing a crisis from derailing your recovery.
Integrated Care for Complex Challenges
Many people struggling with severe PTSD are fighting other battles at the same time. Trauma is often deeply intertwined with co-occurring conditions like substance use disorders, major depression, or crippling anxiety. Trying to treat each of these issues separately with different outpatient providers can feel disjointed and, frankly, ineffective.
This is where a PTSD inpatient treatment program really shines. It offers a truly integrated approach, addressing every aspect of your health under one roof. Your entire team—psychiatrists, therapists, medical doctors, and addiction counselors—works together to create a single, unified treatment plan that makes sense for you.
This means the medication you take for anxiety is managed in lockstep with your trauma therapy. If you’re also struggling with addiction, you’ll get specialized support from people who understand that substance use is often a way of coping with unbearable traumatic stress. This integrated model ensures one part of your health isn’t neglected while another is treated, leading to a much more stable and sustainable recovery.
The table below breaks down the key advantages you get from this kind of immersive care model.
Key Advantages of PTSD Inpatient Treatment
| Benefit | Description | Impact on Recovery |
|---|---|---|
| 24/7 Medical & Clinical Support | Immediate access to medical staff and therapists ensures safety and provides real-time support during moments of crisis or distress. | You’re never alone in your most difficult moments, which builds confidence and prevents setbacks. |
| Trigger-Free, Safe Environment | Removing yourself from daily stressors allows your nervous system to calm down, creating the stability needed for deep therapeutic work. | Your body and mind can finally relax enough to engage in therapy without being in constant survival mode. |
| Intensive & Focused Therapy | A structured schedule of daily individual and group therapy accelerates the healing process far more quickly than weekly appointments. | Progress that might take months or years outpatient can often be achieved in a much shorter, concentrated timeframe. |
| Integrated Co-Occurring Disorder Treatment | Seamlessly addresses related issues like substance abuse or severe depression in a unified, comprehensive plan. | Treats the whole person, not just one symptom, which is essential for lasting stability and well-being. |
| Peer Support Community | Living alongside others who truly understand your struggle reduces feelings of isolation and builds a powerful network of mutual support. | You realize you aren’t broken or alone, fostering a sense of hope and shared purpose that is incredibly healing. |
Ultimately, the power of an immersive environment lies in its singular focus. It gives you the rare and invaluable gift of time and space—time to concentrate completely on your well-being, and space to finally heal without the world pressing in on you from all sides.
How to Navigate Admissions Costs and Insurance
Deciding to pursue PTSD inpatient treatment is a major, courageous step. But once you’ve made that decision, the practical side of things—like admissions and costs—can feel incredibly daunting. My goal here is to demystify this process, turning what seems like a mountain of logistics into a clear, manageable path toward healing.
The journey usually kicks off with a simple, confidential phone call. This leads to a thorough clinical assessment where a professional works to understand your specific situation, the severity of your symptoms, and any other co-occurring conditions you might be facing. From that point on, the admissions team is there to walk you through everything, making sure you know exactly what to expect on your first day. It’s a process designed for clarity and support right from the start.
Understanding the Costs Involved
Let’s be upfront about the costs of PTSD inpatient treatment. Transparency is key to planning. The total cost isn’t just for a room; it covers a wide range of services that create the immersive, therapeutic environment essential for real recovery. Think of these not as line items on a bill, but as the fundamental components of your healing journey.
This investment in mental health is part of a much larger trend. The global market for PTSD treatment was valued at roughly USD 2.37 billion in 2025 and is projected to climb to USD 3.42 billion by 2034. This growth shows just how much society is beginning to prioritize mental healthcare.
So, what are you actually paying for?
- Specialized Therapeutic Care: This includes your daily one-on-one therapy sessions, group work, and proven modalities like EMDR or CPT.
- 24/7 Medical and Clinical Staffing: Having doctors, psychiatrists, and nurses available around the clock is crucial for your safety and well-being.
- Accommodations and Meals: This covers your room, board, and nutritious meals specifically planned to support both physical and mental health.
- Holistic and Experiential Activities: Many programs include therapies like yoga, art, or equine therapy, which are often covered in the overall cost.
Decoding Your Insurance Coverage
Trying to understand your health insurance policy can feel like learning a whole new language. It’s a frustrating but critical part of accessing care. The good news is that most plans, including those on the Affordable Care Act (ACA) marketplace, are required to cover mental health services like inpatient treatment. The catch? The level of coverage can vary dramatically from one plan to another.
Your first step should always be to verify your benefits. An admissions coordinator at your chosen facility can be a lifesaver here—they will contact your insurance provider directly to figure out exactly what’s covered and what your out-of-pocket costs might be.
Key Insurance Terms to Know:
- Medical Necessity: This is the standard insurance companies use to determine if care is essential. The facility’s clinical assessment provides the formal documentation to prove it.
- Pre-authorization: Many plans require a green light before you’re admitted. The admissions team handles this paperwork and communication for you.
- Deductible, Co-pay, and Co-insurance: These are the three parts of the cost that you are responsible for. Getting a clear breakdown of these helps you prepare financially.
To get a head start, we’ve put together a resource that walks you through using your policy for treatment. Take a look at our guide on finding insurance that covers rehab for more information.
Exploring Other Financial Pathways
If your insurance doesn’t cover the full cost, or if you don’t have insurance, please don’t lose hope. Several other financial options exist that can make PTSD inpatient treatment possible. Quality facilities are deeply committed to helping people find a way to get the help they need.
Many centers offer flexible arrangements to close the financial gap. It’s always worth asking about these possibilities:
- Facility Payment Plans: Some treatment centers will work with you to create a structured payment plan, allowing you to pay your share over time.
- Sliding-Scale Fees: Certain non-profits and state-funded programs may adjust their fees based on your income, making care much more affordable.
- Specialized Grants and Scholarships: Grants are often available for specific groups, such as military veterans, first responders, or survivors of violent crime.
Sorting through the financial details is a vital part of the process, but you absolutely do not have to do it alone. The admissions team at a treatment center is your best resource for understanding costs, maximizing your insurance benefits, and exploring every available option to make recovery your new reality.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Preparing for Life After Inpatient Treatment
Leaving the protective bubble of a PTSD inpatient treatment center can feel overwhelming, like you’re stepping onto a whole new planet. The real goal of any good program isn’t just to get you stable for the moment; it’s to get you ready for the long road ahead. In many ways, recovery doesn’t end when you check out—that’s when it truly begins.
Think of it like this: your time in residential care was like learning to fly in a high-tech simulator. You learned the controls and practiced in a perfectly safe environment. Your aftercare plan is the pre-flight checklist and flight path for navigating the real, unpredictable sky. A top-tier program works with you to create this plan, building a solid bridge from the structured support you’ve had to the realities of your daily life.
Building Your Post-Treatment Support System
One of the first and most important parts of your plan is setting up your ongoing professional care. Before you even pack your bags to go home, your treatment team should be working to connect you with outpatient therapists, psychiatrists, or specialized support groups right in your community.
The goal is a seamless handoff, with no gaps in your care. You should leave with appointments already on the calendar and contact numbers in your phone. This professional network is your crew on the ground.
But it’s not just about professionals. Involving family and close friends is just as critical. Many facilities offer family therapy sessions during your stay, and continuing these can make a world of difference. It helps your loved ones understand what you’re going through and how they can be a genuine help, not a source of stress. Building this circle of care is one of the most powerful things you can do for your long-term health. For a deeper look, you can read more about why these relationships are fundamental to recovery.
“Your aftercare plan is your personal recovery playbook. It outlines the strategies, resources, and support systems you’ll rely on to maintain your progress and confidently handle challenges as they arise.”
Creating a Relapse Prevention Strategy
Heading home means you’ll eventually run into the people, places, and situations that might trigger your PTSD symptoms. That’s why a solid relapse prevention strategy is a non-negotiable part of your aftercare plan. It’s about getting ahead of your triggers, not just reacting when they pop up.
Your strategy should be a practical, written guide that includes:
- Trigger Identification: A specific list, created with your therapist, of your personal internal triggers (like memories or feelings) and external ones (like sounds or locations).
- Coping Skill Reinforcement: A cheat sheet of the exact grounding techniques, mindfulness practices, or communication scripts you found most effective during treatment.
- Crisis Planning: A clear, step-by-step action plan for moments of intense distress. Who do you call first? What’s the second step? Having this mapped out removes the guesswork when you’re feeling overwhelmed.
This isn’t about walking on eggshells for the rest of your life. It’s about engaging with the world wisely. Armed with a clear plan, you shift from being reactive to your trauma to being proactive about your well-being. It’s how you take the foundation built during your PTSD inpatient treatment and use it to construct a resilient, meaningful life, no matter what challenges come your way.
Answering Your Questions About PTSD Inpatient Programs
Even after you see the value in getting help, the idea of checking into a PTSD inpatient program can bring up a lot of practical questions. It’s normal to feel a bit overwhelmed by the details. Getting straight answers can give you the confidence you need to make the right choice for your future. Let’s walk through some of the most common questions people have.
How Long Will I Need to Be There?
There’s no magic number here; the length of your stay is entirely based on your unique situation. Most programs run anywhere from 30 to 90 days, but the final timeline really depends on the severity of your PTSD and how you’re progressing through treatment. Your clinical team will work with you to figure out what makes the most sense for your long-term recovery.
“The goal isn’t to stick to a rigid calendar. It’s about making sure you’ve built a solid foundation of coping skills and feel ready to step back into your daily life with confidence.”
Can I Still Talk to My Family and Friends?
Absolutely. Connection with your support system is a huge part of healing. However, that contact is usually structured to help your recovery, not get in the way of it.
Most centers set aside specific times for phone calls. Many also bring family into the process through therapy sessions, which can happen in person or online. This is a powerful way to mend relationships and teach your loved ones how to best support you when you return home.
Expect contact to be a bit limited when you first arrive. This isn’t a punishment; it’s a way to help you fully settle in and focus on your healing without distractions from the outside world.
What if I Have Other Health Issues or Need Medication?
This is exactly where an inpatient program shines. When you’re admitted, you’ll go through a thorough medical and psychiatric evaluation to give the team a complete picture of your health. The facility’s medical staff is there to manage all your needs from day one.
Here’s what that integrated care looks like:
- Medication Management: The on-site medical team will handle any medications you’re taking, whether for PTSD or another condition.
- Whole-Person Health: Your physical and mental well-being are treated as two sides of the same coin, because they are deeply connected.
- Constant Medical Support: You have 24/7 access to medical professionals who can handle any health concerns that pop up, ensuring you are safe and properly cared for around the clock.
Finding the right path to recovery can feel complicated, but you don’t have to figure it out on your own. If you or someone you care about is struggling, Addiction Helpline America is available 24/7. We offer confidential support and can help guide you toward the treatment that fits your needs. Reach out today by visiting us at https://addictionhelplineamerica.com.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.















