Understanding Opioids: A Critical Health and Safety Guide
Opioids are a class of powerful drugs that include prescription pain relievers (like oxycodone), synthetic substances (like fentanyl), and illegal drugs (like heroin). They work by binding to receptors in your brain to block pain signals, but they also carry serious risks including addiction, overdose, and death.
Quick Facts About Opioids:
- What they are: Natural, semi-synthetic, or synthetic drugs derived from or mimicking compounds in the opium poppy plant
- How they work: Attach to opioid receptors to block pain signals and release dopamine
- Medical uses: Treating severe pain after surgery, injury, or from cancer
- Main risks: Addiction, respiratory depression, overdose, death
- Current crisis: In 2023, approximately 5.7 million people in the United States had opioid use disorder, and overdose deaths continue to rise, largely due to illicit fentanyl.
- Warning signs of overdose: Slow or stopped breathing, blue lips or fingernails, unconsciousness, pinpoint pupils
The opioid crisis is a sobering reality. It began with increased prescriptions of medications like oxycodone in the 1990s, and today, it’s driven by synthetic opioids like fentanyl, which is 50 to 100 times more potent than morphine. Tragically, about 75% of people in the U.S. who became addicted to street opioids such as heroin during the 2000s report that they started out taking prescription opioid drugs. Fentanyl is now often mixed into other drugs without the buyer’s knowledge, leading to a surge in accidental overdoses.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
But here’s what you need to know: opioid use disorder is treatable, and recovery is possible. Whether you’re taking prescription opioids for pain, worried about a loved one, or seeking help for addiction, understanding these drugs is the first step toward safety.
At Addiction Helpline America, we help individuals and families steer the complexities of opioid addiction and recovery. Our team of specialists connects people with life-saving treatment and support, providing accurate information and compassionate guidance for those dealing with prescription or illicit opioids.

Common opioids vocab:
What Are Opioids and How Are They Used?
What are opioids and where do they come from?
Opioids are drugs that interact with opioid receptors in your brain and body to produce powerful effects, especially pain relief. The term covers a broad family of substances, both natural and man-made.
While often used interchangeably, “opiate” and “opioid” have a slight difference. Opiates are natural compounds from the opium poppy plant, Papaver somniferum. Natural opioids (or true opiates) like morphine and codeine are extracted directly from this plant.
Semi-synthetic opioids are created in labs by chemically modifying natural opiates. This category includes prescription drugs like oxycodone (OxyContin, Percocet) and hydrocodone (Vicodin), as well as the illicit drug heroin.
Synthetic opioids are entirely man-made in labs to mimic the effects of opiates. Common examples include fentanyl and tramadol. Illicitly manufactured fentanyl is a primary driver of the current overdose crisis due to its extreme potency.
How do opioids work in the body?
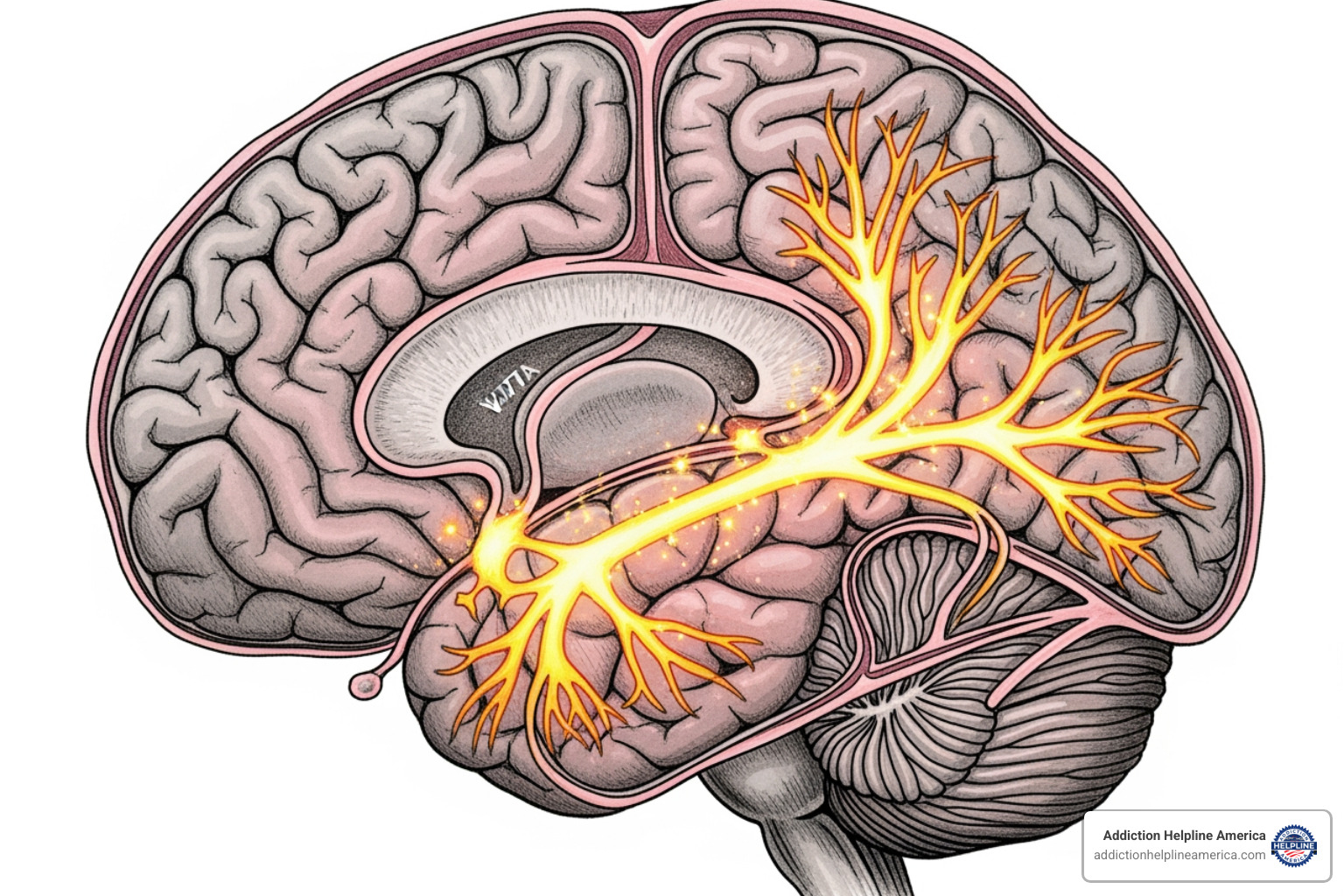
When you take an opioid, it travels through your bloodstream to opioid receptors on nerve cells in your brain, spinal cord, and gut. The opioid molecule fits into these receptors like a key in a lock, setting off two main effects:
- It blocks pain signals from traveling up the spinal cord to your brain. This is why opioids are so effective at relieving severe pain.
- It triggers a flood of dopamine in the brain’s reward system. This creates a powerful sense of euphoria or well-being. Your brain is hardwired to repeat behaviors that cause this feeling, which is why opioids are so addictive, even when taken as prescribed.
Common Types of Opioids
The opioid family includes both legal medications and dangerous street drugs.
- Prescription Opioids: Legally prescribed for pain, these include oxycodone, hydrocodone, morphine, codeine, and fentanyl. When prescribed, fentanyl is reserved for the most severe pain, such as after major surgery or for advanced cancer.
- Illicit Opioids: These have no legitimate medical use. Heroin is a well-known semi-synthetic opioid made from morphine. Research shows about 75% of people who became addicted to heroin during the 2000s started with prescription opioid painkillers.
- Illicitly Manufactured Fentanyl: Unlike prescription fentanyl, this is made in illegal labs and often mixed into other drugs like heroin, cocaine, or counterfeit pills, frequently without the user’s knowledge. This is the main cause of the recent spike in overdose deaths.
TABLE: Comparing Potency, Origin, and Risk of Different Opioids
| Opioid Type | Origin | Potency (Relative to Morphine) | Common Uses | Risk Profile |
|---|---|---|---|---|
| Morphine | Natural | 1x (Baseline) | Severe pain (hospital, cancer) | High addiction, overdose risk |
| Codeine | Natural | 0.1x | Mild-moderate pain, cough | Moderate addiction, overdose risk |
| Heroin | Semi-Synthetic | 2-5x | Illicit use only | Very high addiction, overdose risk |
| Hydrocodone | Semi-Synthetic | 1x | Moderate-severe pain (prescription) | High addiction, overdose risk |
| Oxycodone | Semi-Synthetic | 1.5x | Moderate-severe pain (prescription) | High addiction, overdose risk |
| Fentanyl | Synthetic | 50-100x | Severe pain (prescription), illicit use | Extremely high addiction, overdose risk |
| Tramadol | Synthetic | 0.2x | Moderate pain (prescription) | Moderate addiction, overdose risk |
Medical Uses and Safe Prescription Practices
Despite the risks, opioids have legitimate medical uses when managed carefully.
They are most effective for acute pain management, such as after major surgery or a serious injury. For this purpose, they are typically needed for only a few days. They are also a cornerstone of palliative care for managing severe cancer-related pain.
Using opioids for chronic non-cancer pain is more complex and requires extreme caution due to the high risk of dependence. Medical guidelines now emphasize non-opioid alternatives first.
Following doctor’s instructions for safe use
If your doctor prescribes opioids, safe use is critical. Take the lowest possible dose for the shortest time necessary. Never share your prescription, as a dose safe for you could be fatal for someone else. Store medications securely in a locked cabinet and dispose of unused pills properly through pharmacy take-back programs.
Talk openly with your doctor about your pain levels, side effects, and any personal or family history of substance use. Ask about non-opioid alternatives like physical therapy, acupuncture, or anti-inflammatory medications. Before starting, review the FDA’s guide: What to Ask Your Doctor before Taking Opioids.
Understanding the Risks of Opioids: Misuse, Addiction, and OUD
Even when used as prescribed, opioids carry significant risks that range from uncomfortable side effects to life-threatening emergencies.
What are the risks and side effects associated with opioid use?
Common side effects include drowsiness, sedation, mental fog, nausea, vomiting, and severe constipation. These can occur even with short-term use.
Serious and long-term risks are more dangerous:
- Respiratory Depression: This is the most critical risk. Opioids slow breathing, and if it slows too much, it can lead to oxygen deprivation (hypoxia), brain damage, and death. This risk is magnified when opioids are mixed with alcohol or other sedatives.
- Tolerance and Dependence: Over time, your body adapts, requiring higher doses for the same effect (tolerance). Your body may also become physically dependent, meaning it needs the drug to function normally, leading to severe withdrawal symptoms if you stop suddenly.
- Opioid-Induced Hyperalgesia: Long-term use can paradoxically make you more sensitive to pain.
- Other Health Issues: Extended use can cause hormonal imbalances, cardiovascular changes, a weakened immune system, and an increased risk of depression and anxiety. Injecting opioids carries risks of HIV, hepatitis C, and heart infections (endocarditis).
How Opioid Use Disorder (OUD) develops
Opioid Use Disorder (OUD) is a chronic brain disease, not a character flaw. The intense dopamine rush from opioids rewires the brain’s reward system. Areas responsible for judgment, decision-making, and impulse control are fundamentally changed. The brain begins to treat the drug as necessary for survival, leading to compulsive use despite devastating consequences to health, relationships, and finances.
This brain change explains why the progression from prescription to illicit use is common. About 75% of people in the U.S. who became addicted to street opioids such as heroin during the 2000s report that they started out taking prescription opioid drugs. When prescriptions become too expensive or hard to get, the altered brain chemistry drives individuals toward cheaper, more accessible alternatives like heroin or fentanyl.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Signs of Opioid Misuse and Addiction
Recognizing the warning signs of misuse or addiction can save a life. Look for these changes:
Behavioral Signs:
- Isolating from family and friends; increased secrecy
- “Doctor shopping” (visiting multiple doctors for prescriptions)
- Neglecting work, school, or family responsibilities
- Sudden financial problems or stealing
- Obsessive focus on obtaining and using opioids
- Risky behaviors, such as driving while impaired
Physical Signs:
- Frequent drowsiness or “nodding off”
- Constricted, “pinpoint” pupils
- Unexplained weight loss or poor hygiene
- Withdrawal symptoms (anxiety, sweating, nausea, muscle aches) when unable to use
- Track marks from injecting drugs
Opioid addiction often co-occurs with other mental health challenges. Getting comprehensive support is crucial. Learn more about mental health helpline services that can help.
The Dangers of Fentanyl
Fentanyl, a synthetic opioid, is 50 to 100 times more potent than morphine. An amount as small as a few grains of salt can be lethal. While prescription fentanyl has medical uses, illicitly manufactured fentanyl has flooded the drug market because it is cheap to produce.
One of the greatest dangers is counterfeit pills. These are made to look exactly like prescription medications (e.g., oxycodone, Xanax) but contain deadly doses of fentanyl. This has led to a sharp rise in overdose deaths among adolescents who may experiment with what they believe is a safe pill.
Fentanyl is also frequently mixed into other drugs like heroin, cocaine, and methamphetamine, often without the user’s knowledge. This means any use of illicit drugs carries a risk of fatal fentanyl exposure. For more details, see this Information on Fentanyl from the CDC.
Recognizing and Responding to an Opioid Overdose

An opioid overdose is a life-threatening emergency. Knowing the signs and how to respond can save a life.
What is an opioid overdose, and what are its signs?
An overdose occurs when a person consumes more opioids than their body can handle, causing respiratory depression—breathing that becomes dangerously slow or stops completely. Without oxygen, brain damage, coma, and death can occur within minutes. Opioid overdose deaths are rising in the United States, primarily due to illicitly manufactured fentanyl.
Recognize these critical signs of an overdose:
- Unconsciousness: The person cannot be woken up.
- Breathing: Breathing is very slow, shallow, erratic, or has stopped.
- Discoloration: Lips, skin, and fingernails turn blue, gray, or purplish.
- Pupils: Pupils are constricted to a tiny pinpoint.
- Body: The body is limp.
- Sounds: Choking, gurgling, or loud snoring sounds (a “death rattle”).
What to Do in an Overdose Emergency
If you suspect an overdose, act immediately. Every second counts.
- Call 911 right away. This is the most important step. Give your exact location and report a possible overdose.
- Administer naloxone (e.g., Narcan) if available. It is safe to use even if you’re unsure it’s an opioid overdose. Follow the instructions on the package.
- Try to keep the person awake and breathing. Talk to them loudly and rub your knuckles hard on their breastbone.
- Lay them on their side. If they are unconscious, place them in the recovery position to prevent choking if they vomit.
- Begin rescue breathing if they are not breathing. Tilt their head back, pinch their nose, and give one breath every five seconds until help arrives.
- Stay with the person. Monitor them closely. If they don’t respond to naloxone in 2-3 minutes, give a second dose if you have one.
For more detailed guidance, review these resources from the CDC: How to respond to an overdose from the CDC.
The Role of Naloxone
Naloxone is a life-saving medication that can reverse an opioid overdose. As an opioid antagonist, it has a stronger bond to the brain’s opioid receptors than opioids do. When administered, it knocks the opioids off the receptors and temporarily blocks their effects, restoring normal breathing within minutes.
Naloxone is safe, non-addictive, and increasingly available without a prescription at pharmacies and through community programs. If you or someone you know uses opioids for any reason, carrying naloxone is a critical safety measure. It buys essential time until emergency medical help arrives and can be the difference between life and death.
Prevention, Treatment, and Recovery from Opioid Addiction
Opioid addiction is a treatable disease. With effective prevention, treatment, and support, long-term recovery is achievable.

What are the strategies for preventing opioid misuse and addiction?
Prevention starts with awareness and taking proactive steps to reduce risk.
- Safe Medication Practices: If prescribed opioids, take the lowest effective dose for the shortest time needed. Never share your medication. Taking a pill in any way other than prescribed is misuse and dramatically increases risk.
- Secure Storage and Disposal: Keep opioids in a locked cabinet. Dispose of unused medication safely through pharmacy take-back programs to prevent diversion and accidental exposure.
- Explore Non-Opioid Pain Therapies: For many types of pain, especially chronic pain, alternatives like physical therapy, acupuncture, NSAIDs, and nerve blocks can be more effective and safer than opioids. Discuss these options with your doctor.
- Patient and Community Education: Understanding the risks of opioids is vital, especially for young people. Many teen overdose deaths involve counterfeit pills laced with fentanyl. Open conversations about these dangers save lives.
How Opioid Use Disorder is Treated
Opioid Use Disorder (OUD) is a treatable medical condition, not a moral failing. The most effective approach is Medication-Assisted Treatment (MAT), which combines FDA-approved medications with behavioral therapy. MAT is the gold standard for treating OUD, as it addresses both the physical and psychological aspects of addiction.
Three FDA-approved medications are used in MAT:
- Buprenorphine: A partial opioid agonist that reduces cravings and withdrawal symptoms without producing a strong high. It can be prescribed in a doctor’s office, making treatment highly accessible.
- Methadone: A full opioid agonist that eliminates withdrawal and cravings. It is dispensed in specialized clinics, providing structure and daily support.
- Naltrexone: An opioid antagonist that blocks the effects of opioids, preventing a high if a person relapses. It is available as a daily pill or a monthly injection (Vivitrol) and is best for those who have completed detox.
These medications are safe, effective, and recommended even for pregnant individuals with OUD. They work best when combined with behavioral therapies like Cognitive Behavioral Therapy (CBT) and counseling. These therapies help individuals change thought patterns, manage triggers, and develop healthy coping skills. Support groups like Narcotics Anonymous provide a vital community of peers who understand the challenges of recovery.
For more information on treatment, explore our intensive outpatient program options or learn about managing withdrawal symptoms. Ongoing scientific research on OUD medications continues to improve outcomes and offer hope.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Conclusion: Finding Hope and Help for Opioid Addiction
The opioid crisis has had a devastating impact, but behind the staggering statistics are real people who deserve compassion and a chance to heal.
Here is the most important message: recovery from opioid use disorder is absolutely possible. This is a medical fact supported by decades of research. With evidence-based approaches like Medication-Assisted Treatment (MAT), which combines medication with counseling, people can and do rebuild their lives.
If you or someone you love is struggling with opioids, seeking help is an act of tremendous courage. Addiction is a treatable medical condition, and you do not have to face it alone.
At Addiction Helpline America, we provide free, confidential, and personalized guidance to connect you with the right addiction and mental health treatment. Our mission is to help you steer the path to recovery without judgment. We listen to your unique situation and match you with a program from our vast network that fits your needs.
The journey to recovery begins with a single step. Don’t wait. Treatment works, and a healthier, hopeful future is possible. Find confidential, personalized guidance for recovery at Addiction Helpline America today. We’re ready when you are.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.















