
Understanding The Real Crisis Behind The Statistics
The opioid crisis isn’t just about numbers; it’s about people. It’s the story of a parent prescribed opioids after an accident, slowly slipping into dependency without realizing it. It’s the young adult experimenting with pills at a party, completely unaware of addiction’s power. These are the human stories behind the headlines, and they show the true cost of this epidemic.
This didn’t happen overnight. Several factors contributed, like overprescribing painkillers for chronic pain, a misunderstanding of how addictive these drugs are, and the easy availability of illegal opioids like heroin and fentanyl. These factors created a perfect storm, pulling people from all walks of life into the devastating cycle of addiction. Opioid addiction is a global issue, with over 16 million people affected worldwide and 2.1 million in the United States alone. This widespread problem highlights the urgent need for effective treatment. In the U.S., roughly 3-12% of people treated with opioids for chronic pain can develop an addiction. For more information on the pervasiveness of this issue, check out this resource: The Opioid Crisis.
Beyond “Just Say No”: Why Traditional Approaches Fail
The old “just say no” approach to drug prevention, although well-meaning, misses the point about addiction. It sees addiction as a moral failing, a weakness, instead of the complex medical issue it actually is. Imagine trying to “just say no” to intense hunger after not eating for days. Like hunger, addiction involves powerful biological and psychological forces that often override rational thought. That’s why simply telling someone to stop using drugs is rarely effective.
The Importance of Multiple Treatment Paths
Effective opioid addiction treatment recognizes this complexity and offers different paths to recovery. There’s no one-size-fits-all solution for addiction, just like there isn’t one for heart disease or diabetes. Different people respond to different treatments. What works for one might not work for another. This is why treatment plans need to be personalized. They need to consider things like a person’s medical and mental health history, their support system, and their personal goals.
Recognizing the Signs and Breaking the Stigma
Knowing the early signs of opioid addiction is vital. These can include things like changes in behavior, mood swings, neglecting responsibilities, and increased secrecy. However, the stigma around addiction often stops people from asking for help. Many worry about being judged, feeling ashamed, or facing consequences for their jobs or relationships. Breaking down this stigma is key to creating a safe and supportive environment where people can get help. It’s a critical step in fighting back against this devastating epidemic. Understanding that addiction is a medical condition, not a moral failing, is the first step toward a more compassionate and successful response to the opioid crisis.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
How Modern Treatment Actually Works: Beyond Old Assumptions

Think of opioid addiction like managing diabetes. It’s a chronic condition needing ongoing care, not a moral failing fixable with willpower alone. This understanding is key. Modern research shows addiction is a complex brain disease, hijacking the pathways responsible for our decisions. It’s not about weakness; it’s about neurobiology.
Imagine a car with faulty brakes. No matter how hard the driver pushes the pedal, stopping is a struggle. Similarly, addiction disrupts the brain’s “braking system” for impulses, making it incredibly tough to resist drug use.
This means effective opioid addiction treatment needs to go deeper than addressing just the physical dependency.
It needs to address the psychological trauma, difficult social situations, and other mental health conditions that often contribute to addiction. It’s a whole-person approach recognizing the link between mind and body.
Top treatment programs now combine several evidence-based methods to create truly personalized treatment plans. This reflects the reality that one size doesn’t fit all in recovery.
The Power of Combined Approaches
Instead of a single solution, modern treatment centers often blend medication-assisted treatment (MAT) with counseling and behavioral therapies. MAT uses medications approved by the FDA to help stabilize brain chemistry and lessen cravings.
This gives people the space to focus on the psychological and emotional work of recovery without constantly fighting intense withdrawal.
Therapies like cognitive behavioral therapy (CBT) and motivational interviewing give individuals coping skills, relapse prevention plans, and the ability to navigate tricky situations without turning to drugs.
The Role of Family and Community
Family and community support are vital for building a solid recovery. Family therapy can help repair relationships damaged by addiction and empower loved ones to offer effective support.
Support groups, peer recovery coaches, and community resources offer continued encouragement and connection, reducing the isolation that can often trigger relapse.
The World Health Organization (WHO) recognizes the importance of this comprehensive approach, updating guidelines on opioid dependence treatment and overdose prevention to improve availability and save lives. You can learn more about their work at the provided link.
Redefining Success
Modern opioid addiction treatment programs also define success differently than older models. While abstinence is often a goal, the focus is broader. It’s about improved mental and physical health, stable housing, employment, and stronger relationships.
This shift acknowledges that recovery is a journey, with progress taking many forms. It’s about rebuilding a fulfilling life, not just stopping drug use. It’s about taking back control, finding purpose, and creating a future filled with hope.
Medication-Assisted Treatment: Science Meeting Hope
Medication-assisted treatment (MAT) offers real hope for those struggling with opioid addiction. It’s not about trading one addiction for another. Instead, think of MAT like using insulin to manage diabetes – it’s a medical tool for a medical condition. MAT uses medication to help the brain regain normal function while a person rebuilds their life.
Understanding the Three Main Medications
Three FDA-approved medications form the core of MAT: methadone, buprenorphine, and naltrexone. Each works differently and has distinct benefits. Let’s explore them individually.
- Methadone: This medication acts as a full opioid agonist. This means it activates opioid receptors in the brain, much like other opioids. However, methadone does this in a controlled way. It reduces cravings and withdrawal symptoms without the intense “high” of illicit opioids. This stabilization helps people focus on therapy and rebuilding their lives.
- Buprenorphine: This medication is a partial opioid agonist. It activates opioid receptors, but to a lesser extent than methadone or illicit opioids. This offers a middle ground: it reduces cravings and withdrawal symptoms with a lower risk of misuse and overdose. Suboxone is a common form of buprenorphine, combining it with naloxone to further discourage misuse.
- Naltrexone: This medication works differently than methadone or buprenorphine. It’s an opioid antagonist, meaning it blocks opioid receptors. This prevents other opioids from having their usual effects, making them less desirable and reducing the risk of relapse. Importantly, a person needs to be fully detoxed from opioids before starting naltrexone.
To help compare these three medications, take a look at the table below:
Medication-Assisted Treatment Options Comparison: This table provides a detailed comparison of the three main MAT medications, including how they work, administration methods, and typical treatment duration.
| Medication | How It Works | Administration | Treatment Duration | Best For |
|---|---|---|---|---|
| Methadone | Full opioid agonist; activates opioid receptors in a controlled manner | Oral | Long-term, often years | Individuals with severe opioid dependence who haven’t responded to other treatments |
| Buprenorphine | Partial opioid agonist; activates opioid receptors to a lesser degree | Sublingual (under the tongue) or buccal (between cheek and gum) | Varies, often long-term | Individuals who prefer a less intense opioid effect and lower risk of overdose |
| Naltrexone | Opioid antagonist; blocks opioid receptors | Oral or injection | Varies, can be short-term or long-term | Individuals who have successfully detoxed and want to prevent relapse |
As you can see, each medication offers a different approach to managing opioid addiction.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Combining Medication with Counseling for Long-Term Success
MAT isn’t just about medication. It’s most effective when combined with counseling and behavioral therapies. Think of it like this: medication addresses the physical aspects of addiction, while counseling tackles the underlying psychological and emotional roots.
The infographic below visually represents this integrated approach, showing various behavioral therapies often used alongside MAT.
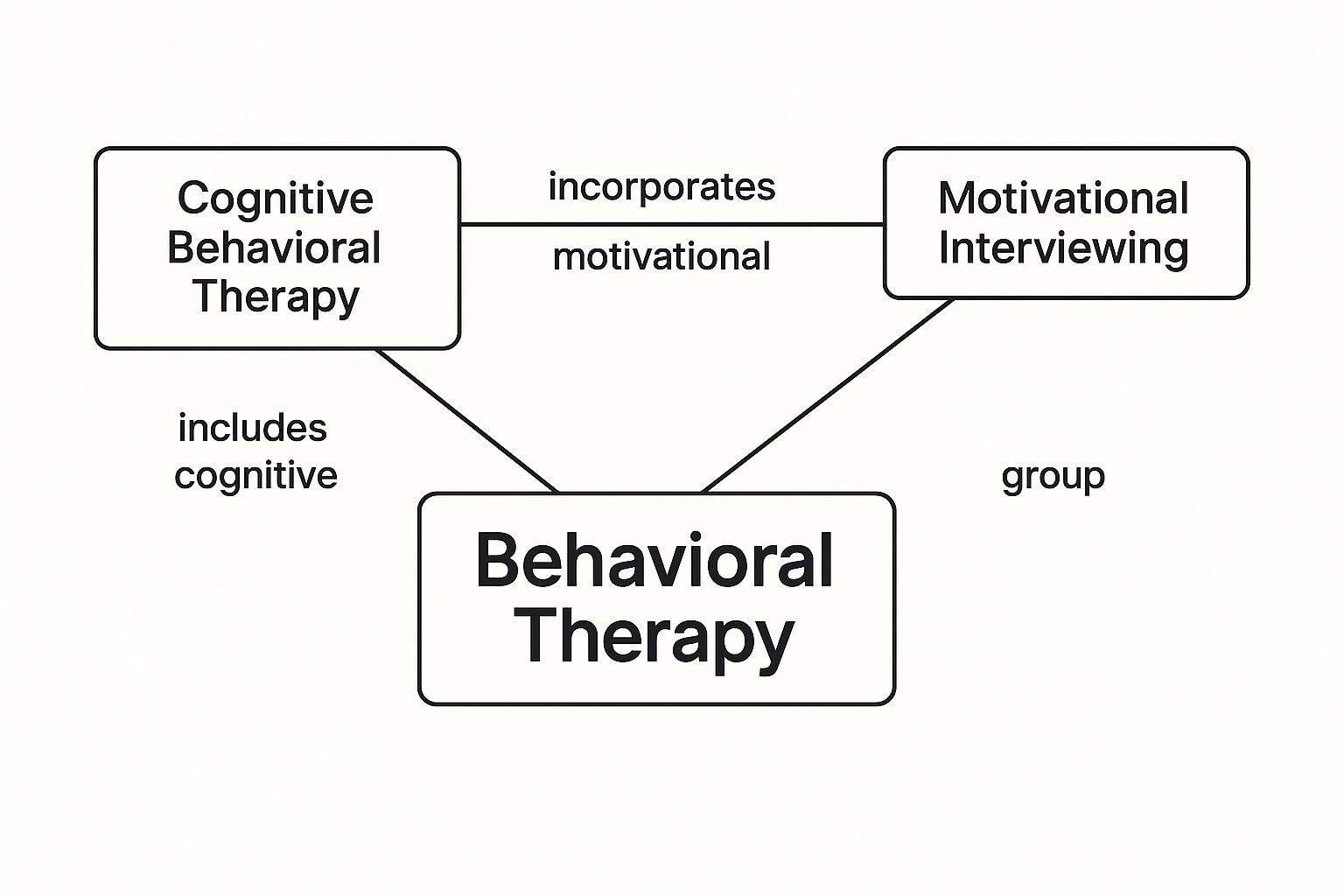
These therapies, including Cognitive Behavioral Therapy and Motivational Interviewing, offer multiple ways to address the emotional side of addiction, providing crucial coping skills and support networks.
Addressing Myths About MAT
Unfortunately, misconceptions about MAT are common. Some people believe it’s just replacing one addiction with another. However, research shows MAT is a vital tool. It helps stabilize individuals, reduce cravings, and allow them to focus on recovery.
It’s important to remember that MAT is a medical treatment backed by scientific evidence. Just like with any medical treatment, discussing these options with a healthcare professional is essential. By understanding how MAT really works and dispelling the myths surrounding it, we can encourage more people to seek help and begin their journey toward recovery.
Choosing Your Treatment Setting: What Really Matters

Finding the right opioid addiction treatment setting isn’t a matter of picking the “best” one, but the one that fits you like a glove. Think of it like choosing a suit: a tailored fit is always better than something off the rack. Recovery is deeply personal, so your treatment should be too. This means taking a close look at all the choices, from intensive residential programs to more flexible outpatient care.
Residential Treatment: 24/7 Support and Structure
Residential treatment provides a highly structured environment, with medical supervision and support available around the clock. This immersive experience can be incredibly helpful for people dealing with severe opioid addiction, especially if they also have other mental health challenges or lack a supportive home environment. Imagine it as a dedicated space where you can put all your energy into recovery, away from daily life’s triggers and distractions. For those considering this option, you might find this helpful: How to Prepare For Rehab.
Imagine it as hitting the “pause” button on life’s chaos, giving you the time and space needed to heal and build a solid foundation for sobriety.
Outpatient Treatment: Flexibility and Integration
Outpatient treatment, on the other hand, offers more flexibility. This allows people to continue working, attending school, or taking care of family responsibilities while getting the treatment they need. Outpatient options run the gamut from intensive outpatient programs (IOPs) with several sessions per week, to partial hospitalization programs (PHPs) offering daytime hospital-level care.
Outpatient programs empower individuals to gradually weave recovery skills into their everyday lives, like adding new threads to a tapestry. This can be particularly beneficial for those who have strong support systems and stable living situations.
Making the Decision: Factors to Consider
Choosing between residential and outpatient treatment for opioid addiction means carefully weighing a number of factors:
- Severity of Addiction: If your opioid dependence is severe, or if you’ve relapsed in the past, the structured environment of residential care might be a better fit. If your addiction is less severe, outpatient care could offer enough support.
- Support System: A strong network of family and friends can be a real asset for those choosing outpatient treatment. If you don’t have that kind of support, residential treatment offers built-in community and encouragement.
- Work/Family Obligations: Outpatient programs let you keep up with work and family, but if these become too much to handle, residential care can provide the space to really focus on getting better.
- Co-occurring Disorders: If you have other mental health conditions alongside addiction, the integrated care offered in many residential programs can be particularly helpful. Outpatient can also address these, but requires careful coordination with other health professionals.
- Financial Resources and Insurance: Residential and outpatient settings have very different costs. It’s essential to understand your insurance coverage and look at your financing options.
To help you visualize these factors, let’s take a look at a comparison table:
Treatment Setting Comparison Guide
Side-by-side comparison of residential and outpatient treatment options, including intensity levels, duration, and suitability factors
| Treatment Type | Time Commitment | Living Situation | Cost Range | Best Suited For |
|---|---|---|---|---|
| Residential | 30-90 days (or longer) | On-site at the treatment facility | Typically higher | Severe addiction, co-occurring disorders, lack of strong support system |
| Outpatient (IOP/PHP) | Varies, typically several hours per week/day | At home | Typically lower | Mild to moderate addiction, strong support system, need to maintain work/family obligations |
This table offers a quick snapshot of the key differences between these two settings. Choosing the right setting for you is crucial for success.
The Spectrum of Care: Finding the Right Fit
Remember, treatment isn’t one-size-fits-all. Your needs may change as you move forward in recovery. You might begin with residential care, then step down to an IOP or PHP, and eventually to individual therapy and support groups. It’s about finding the right level of care for where you are right now in your recovery journey. This personalized, step-by-step approach is key to long-term success. Choosing the appropriate setting is a critical step in rebuilding a fulfilling life free from the grip of opioid addiction.
Therapy That Goes Beyond Talk: Rebuilding From Within

Recovery from opioid addiction isn’t simply about stopping the drug use. It’s a deeper process of addressing the underlying issues and rebuilding a life filled with purpose and meaning. Imagine a house damaged by a storm: you wouldn’t just fix the broken windows. You’d need to repair the foundation to make it truly strong again. Therapy provides that foundational work, offering various approaches to mend the psychological damage caused by addiction.
Cognitive Behavioral Therapy: Rewiring Your Thoughts
Cognitive Behavioral Therapy (CBT) helps individuals recognize and modify negative thought patterns that contribute to drug use. For example, someone struggling with addiction might believe they absolutely need opioids to handle stress. CBT helps challenge that belief and develop healthier coping mechanisms. It’s like rewiring a faulty electrical circuit in the brain, replacing the damaged wires with new, functional ones.
Imagine learning to drive. At first, it feels overwhelming, but with practice, it becomes automatic. CBT works similarly, training your brain to react to stress in healthier ways.
Motivational Interviewing: Finding Your Inner Drive
Motivational Interviewing (MI) is all about fostering inner motivation. Rather than telling someone what to do, therapists using MI guide individuals to discover their own reasons for wanting to recover. It’s a collaborative approach that empowers individuals to take ownership of their recovery journey.
Think of it like a personal trainer. They don’t lift the weights for you; they encourage and support you to reach your own fitness goals. MI helps individuals find their inner drive to get better.
Group Therapy: The Power of Shared Experience
Group therapy offers a safe and supportive space for people to share their stories, learn from others, and build strong connections. Hearing others talk about their struggles can diminish feelings of isolation and shame, reinforcing the idea that recovery is possible.
Sharing your experience in group therapy is like joining a hiking club. You’re all climbing different mountains, but you understand the challenges and celebrate the victories together. That shared journey provides motivation and strength.
Individual Counseling: Addressing Personal Challenges
Individual counseling offers a private setting to explore personal trauma, family issues, and other triggers that contribute to opioid addiction. This personalized approach allows therapists to tailor treatment to each person’s specific needs.
Imagine having a dedicated tour guide on a complex journey. They know the terrain, understand your needs, and can help you navigate the challenges along the way. That’s the role of a therapist in individual counseling.
Innovative Approaches: Contingency Management and Family Therapy
Beyond these core therapies, other effective methods exist. Contingency management uses positive reinforcement to encourage healthy behaviors. Someone might receive vouchers or other rewards for staying drug-free. This approach taps into the brain’s reward system, making positive change more appealing.
Family therapy is crucial for repairing relationships strained by addiction. It helps families understand the nature of addiction, improve communication, and create stronger support systems for ongoing recovery. Because family dynamics often play a significant role in both the development of addiction and the recovery process, addressing these complex relationships is key to creating a supportive and stable environment for long-term success.
These therapeutic approaches, alone or in combination, are essential components of effective opioid addiction treatment. They empower individuals to heal from the inside out, build resilience, and create a future free from addiction’s grip.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Breakthrough Innovations Changing Recovery Outcomes
The world of opioid addiction treatment is constantly changing, offering fresh hope for those who haven’t found success with traditional approaches or need more support. These aren’t just small steps forward; they’re big shifts in how we think about recovery, opening doors to care that’s more personalized, accessible, and effective.
Extended-Release Formulations: Simplifying Medication Management
One key innovation is extended-release medications used in medication-assisted treatment (MAT). Instead of daily doses, these formulations allow for less frequent dosing, sometimes even weekly. Think of it like a time-release fertilizer, steadily nourishing a plant over time.
This eliminates daily clinic visits, making treatment more manageable for people with busy lives or those in rural areas with limited healthcare access. This convenience can greatly improve adherence to treatment plans, a vital ingredient in successful recovery.
Trauma-Informed Therapies: Addressing the Root Causes
Another important shift is the rise of trauma-informed care. This approach recognizes the significant role past trauma, such as abuse or neglect, often plays in addiction. Trauma-informed therapies provide a safe, supportive space to address these underlying wounds.
It’s like carefully tending to the roots of a plant, ensuring a strong foundation for growth. This focus on healing past trauma can be incredibly powerful in breaking the cycle of addiction and supporting long-term recovery.
Technology’s Expanding Role: 24/7 Support
Technology is also making a big difference. Mobile apps and remote monitoring tools offer round-the-clock support, connecting people with resources and encouragement whenever they need it. Imagine having a supportive friend always available to offer guidance.
These tools can track progress, manage cravings, and provide access to virtual counseling. They also offer crucial support for those in rural communities or facing transportation challenges. This increased accessibility broadens the reach of treatment and empowers individuals in their recovery journey. Some apps even offer mindfulness exercises, relapse prevention strategies, and connections to peer support networks.
Personalized Medicine: Tailoring Treatment to the Individual
Personalized medicine is also transforming the field. Genetic testing can now help predict which medications will be most effective for each person. This allows for a more targeted approach, boosting the chances of success. It’s similar to choosing the right fertilizer for a specific plant—what works for one might not work for another.
This personalized approach acknowledges that every recovery journey is unique and requires a tailored treatment plan. Encouragingly, in the United States, drug overdose deaths have recently declined. Provisional data shows a nearly 24% drop in overdose deaths from October 2023 to September 2024 compared to the previous year. This decrease is attributed to public health investments and better data systems for identifying emerging drug threats. Learn more about this positive trend here. You may also be interested in learning more about Rehab Centers for Opioid Addiction.
These innovations hold immense promise for the future of opioid addiction treatment, making recovery more attainable and sustainable for countless individuals. They mark a shift toward more compassionate, effective, and evidence-based care.
Your Next Steps: Creating Your Personal Recovery Plan
Now that we’ve explored the different ways people recover from opioid addiction, let’s talk about how to create a plan that works for you. Think of it like planning a road trip – you wouldn’t just hop in the car and start driving, would you? Recovery also needs careful planning and preparation.
Evaluating Your Options and Asking the Right Questions
First, take an honest look at your situation. Consider the severity of your addiction, your support network (friends, family), your job and family commitments, and any other mental health challenges you might be facing. This self-assessment is like laying the foundation of a house – it needs to be strong to support everything else.
Next, research different treatment providers. Ask important questions, like you’re interviewing someone for a job:
- What types of opioid addiction treatment do they offer?
- Do they use Medication-Assisted Treatment (MAT)?
- What kinds of therapy are available?
- How do they help people prevent relapse?
- What are their success rates?
You’re looking for the best “contractor” to help you rebuild your life.
Preparing for the Journey: Practical and Mental Steps
Getting ready for treatment involves both practical and mental preparation. Think of it like packing for that road trip:
- Insurance Coverage: Figure out what your insurance will pay for and what costs you might have to cover.
- Financial Assistance: Explore programs that can help with costs if needed.
- Legal and Logistical Matters: Arrange for things like time off work, childcare, or other responsibilities.
Mental preparation is just as important:
- Acknowledge Your Addiction: Accepting you have a problem takes courage and is the first step.
- Set Realistic Goals: Recovery is a marathon, not a sprint. Focus on small, manageable steps.
- Build a Support System: Surround yourself with people who support your recovery.
These preparations will make your “trip” smoother.
Navigating Insurance and Finding Financial Support
The screenshot above shows the Substance Abuse and Mental Health Services Administration (SAMHSA) website’s treatment locator tool. This helpful tool can help you find treatment centers near you. It lets you search for centers that offer specific types of opioid addiction treatment. The best part? Finding a treatment center is easy, just based on where you live and what you need.
Don’t let money worries stop you from getting help. Many centers accept insurance, and there are lots of resources to help cover costs. SAMHSA’s website has tons of information on insurance coverage and financial aid.
Accessing Emergency Help: When You Need It Most
If you or someone you know is overdosing on opioids, call 911 immediately. Naloxone, a medication that can reverse an opioid overdose, can be a lifesaver. Learn how to use naloxone and where to get it in your area. Never hesitate to get help in a crisis – it can make all the difference.
Embracing the Journey to Recovery
Remember, recovery is possible. With the right treatment and support, you can overcome opioid addiction and build a healthier, happier life. Every step, no matter how small, is a win. Embrace the journey, and remember you’re not alone.
If you or someone you love is struggling with opioid addiction, contact Addiction Helpline America at https://addictionhelplineamerica.com. We’re here 24/7 to offer confidential support, guidance, and resources to help you navigate recovery. Our trained representatives can connect you with the help you need. Don’t wait – take that first step toward a healthier future today.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.






