Understanding the Opioid Crisis and Finding Effective Help
Opioid addiction solutions include three main approaches that work best when combined:
- Medication-Assisted Treatment (MAT): FDA-approved medications like methadone, buprenorphine, and naltrexone that reduce cravings and prevent withdrawal.
- Counseling and Behavioral Therapy: Individual and group therapy to address underlying causes and build coping skills.
- Recovery Support Services: Peer support, housing assistance, and wraparound services for long-term stability.
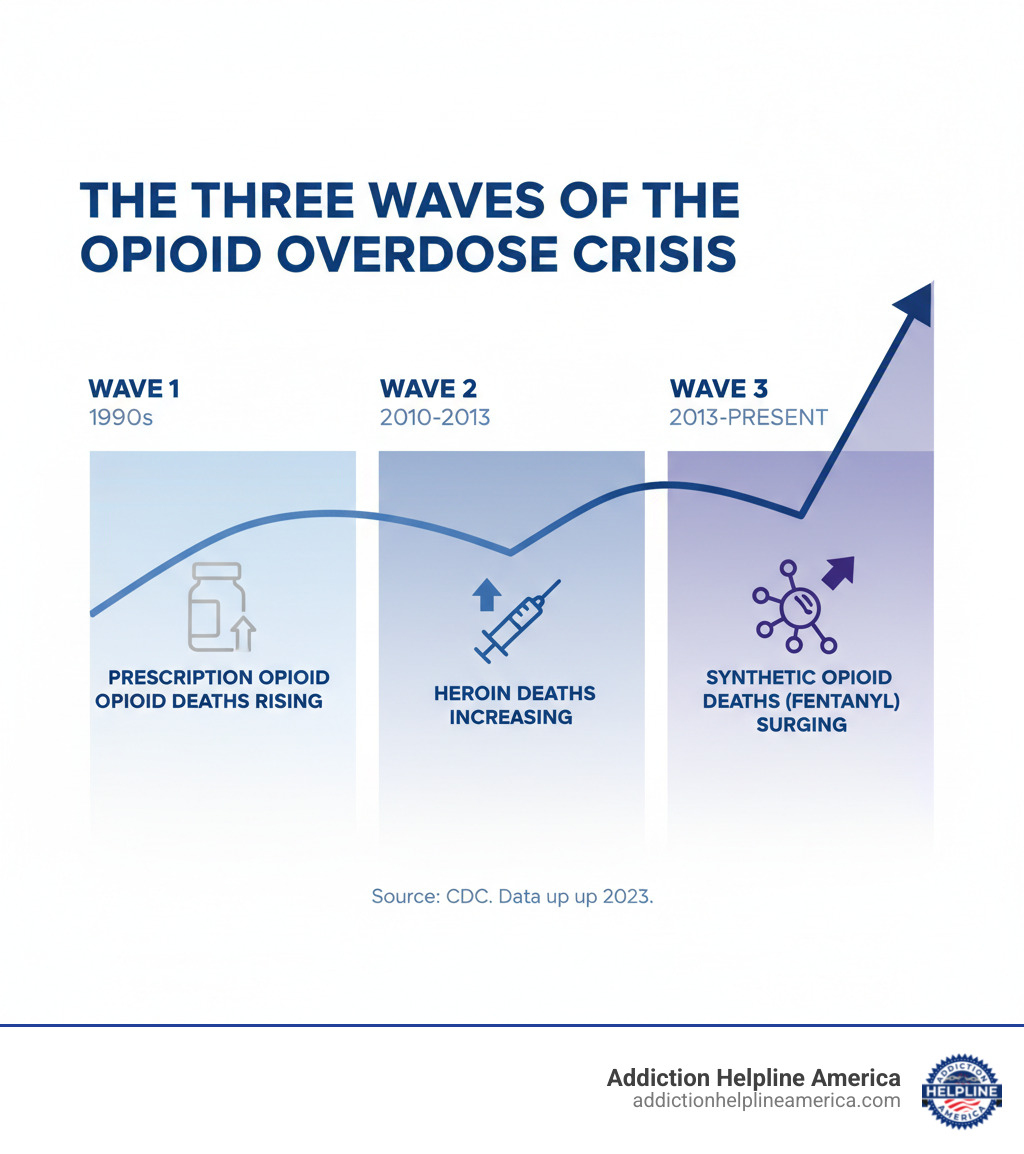
The opioid crisis is a devastating public health emergency. In 2021 alone, over 107,000 people died from drug overdoses, with opioids being the primary driver. The crisis has evolved through three waves: first prescription opioids, then heroin, and now synthetic opioids like illicitly manufactured fentanyl, which is 50 to 100 times more potent than morphine.
Behind these statistics are families searching for help. The good news is that Opioid Use Disorder is a treatable medical condition. Research shows that combining medication with counseling offers the most effective path to recovery, yet millions who need this care never receive it.
This guide provides a comprehensive overview of proven opioid addiction solutions, from emergency response to long-term recovery. Understanding your options is the critical first step.
At Addiction Helpline America, we connect individuals and families with evidence-based opioid addiction solutions through our nationwide network of treatment providers. Our team offers free, confidential guidance to help you find the right program for your unique situation.
Opioid addiction solutions terms to remember:
- Prescription Drugs Treatment
- Top Alcohol & Drug Rehab Centers in Los Angeles, California
- are there any free drug rehab centers
Understanding Opioid Use Disorder (OUD) and the Current Crisis
Opioids are powerful drugs that include prescription pain relievers (like oxycodone), heroin, and synthetic opioids like fentanyl. They work by binding to receptors in the brain, reducing pain and creating feelings of euphoria, which makes them highly addictive. Understanding how opioid use disorder develops is key to finding effective opioid addiction solutions.
What is Opioid Use Disorder (OUD) and How Does It Differ from Physical Dependence?
OUD is a chronic, relapsing brain disease, not a moral failing. It’s important to distinguish it from physical dependence. Physical dependence occurs when the body adapts to a drug, causing withdrawal symptoms if it’s stopped suddenly. A patient taking prescribed morphine for pain will develop physical dependence, but this isn’t the same as addiction.
Addiction, or OUD, involves compulsive use despite harmful consequences. A person with OUD may use more than intended, struggle to quit, and experience intense cravings. They continue using even as it damages their health, relationships, and ability to function. The disorder also involves tolerance (needing more of the drug for the same effect) and using just to avoid withdrawal sickness.
What Are the Primary Causes and Risk Factors Associated with Developing Opioid Addiction?
No single factor causes OUD. It’s a complex mix of genetics, environment, and psychology. A family history of substance use disorder increases vulnerability. Environmental factors like poverty, peer pressure, or chronic stress also play a role. Psychologically, people with depression, anxiety, or PTSD are at higher risk, as they may use opioids to self-medicate emotional pain. For some, the path begins with a legitimate prescription, and experiencing intense euphoria from the medication can be a warning sign of higher addiction potential.
What Are the Signs and Symptoms of Opioid Addiction and Intoxication?
Recognizing the signs can save a life. Someone intoxicated on opioids may be extremely drowsy (“nodding off”), have pinpoint pupils, and exhibit slow or shallow breathing. Other signs include confusion, slurred speech, and nausea.
Behavioral symptoms of addiction include:
- Using more opioids than intended or for longer periods.
- Spending excessive time obtaining, using, or recovering from opioids.
- Failing to meet work, school, or home responsibilities.
- Continuing use despite negative consequences to health or relationships.
- Isolating from friends and family.
- Neglecting personal hygiene or experiencing significant weight loss.
What Are the Different Types of Opioids, Including Prescription and Illicit Forms, and Their Respective Risks?
Opioids include legal medications and illegal street drugs. Prescription opioids like oxycodone (OxyContin, Percocet), hydrocodone (Vicodin), and morphine are prescribed for pain but carry a risk of dependence and addiction. Illicit opioids include heroin, which is highly addictive and carries a high overdose risk.
The greatest threat today is illicitly manufactured fentanyl (IMF). It’s often pressed into counterfeit pills that look like real prescription drugs (e.g., oxycodone, Xanax) or mixed into other drugs like heroin and cocaine, often without the user’s knowledge. This creates a deadly game of Russian roulette, as a user may unknowingly consume a lethal dose.
How Does Fentanyl Pose a Unique Risk in the Current Opioid Crisis?
Fentanyl is 50 to 100 times more potent than morphine, meaning a tiny amount can be fatal. The latest overdose data from CDC WONDER shows synthetic opioids like fentanyl are driving most overdose deaths. Because it can’t be seen, smelled, or tasted, people often consume it unknowingly.
The crisis is further complicated by Xylazine (“tranq-dope”), a veterinary sedative mixed with fentanyl. Naloxone (Narcan) does not reverse xylazine’s effects, making overdoses harder to treat and more deadly. This polysubstance use, often involving stimulants like methamphetamine, marks a dangerous new phase of the changing opioid crisis and underscores the need for comprehensive opioid addiction solutions.
How to Respond to an Opioid Overdose Emergency
When someone overdoses on opioids, every second counts. Knowing how to respond is one of the most urgent opioid addiction solutions.
Recognizing Overdose Signs
An opioid overdose slows down the body’s vital functions. According to the CDC, several signs of an overdose require immediate action:
- The person is unconscious or cannot be woken up.
- Breathing is very slow, shallow, irregular, or has stopped.
- Skin, lips, or fingernails turn blue or gray.
- Pupils are extremely small (“pinpoint pupils”).
- Choking or gurgling sounds are heard.
- The body is limp.
If you see these signs, assume it’s an overdose and act immediately. Do not wait for the person to “sleep it off.”
Immediate Steps
Follow these steps to save a life:
- Call 911 immediately. Tell the dispatcher your location and that someone is unresponsive and may have overdosed. Most states have Good Samaritan laws to protect you from drug-related charges when you call for help.
- Administer naloxone (Narcan) if available. This medication can rapidly reverse an opioid overdose. It is safe and will not harm someone if opioids are not present. The nasal spray is easy to use: insert the nozzle into one nostril and press the plunger.
- Support their breathing. If you are trained, provide rescue breaths (one breath every five seconds) until the person can breathe on their own.
- Place them in the recovery position. Roll the person onto their side to prevent them from choking if they vomit.
- Stay with them until help arrives. Naloxone wears off in 30-90 minutes, and the person could overdose again. Be prepared to give another dose if symptoms return.
The Role of Naloxone (Narcan)
Naloxone is a life-saving medication that blocks opioid receptors in the brain, restoring normal breathing in minutes. It is now available over-the-counter at most pharmacies. Many health departments also distribute free Take Home Naloxone kits. Carrying naloxone and knowing What to Do if You Think Someone is Overdosing is a critical skill for everyone.
At Addiction Helpline America, we believe education on overdose response is a vital part of the solution, saving lives and supporting recovery.
A Deep Dive into Opioid Addiction Solutions
Effective recovery from opioid addiction requires a comprehensive, individualized approach, much like treating other chronic diseases. The most effective opioid addiction solutions combine medical treatment, counseling, and ongoing support.
Withdrawal Management (Detoxification)
Detox is often the first step, involving the safe, medically supervised management of withdrawal symptoms. While opioid withdrawal is uncomfortable (chills, muscle aches, nausea, severe cravings), it is rarely life-threatening. Medications can make the process more bearable.
Why Detox Alone Is Not Enough:
Detox is only a first step. Research on withdrawal management risks shows that without follow-up treatment, relapse is common. After detox, a person’s tolerance to opioids is gone, dramatically increasing the risk of a fatal overdose if they use again. Detox cleanses the body but doesn’t treat the underlying brain disease of addiction.
Medication-Assisted Treatment (MAT): The Gold Standard for Opioid Addiction Solutions
MAT combines FDA-approved medications with counseling and is the gold standard for treating OUD. It is proven to save lives and is not simply replacing one addiction with another. MAT works by stabilizing brain chemistry, reducing cravings, and preventing withdrawal, which allows a person to focus on therapy and rebuilding their life. Medications for Opioid Use Disorder Save Lives by dramatically reducing overdose risk.
The three main medications are:
- Methadone: A full opioid agonist that eliminates withdrawal and cravings. It is dispensed daily at specialized clinics and is highly effective for severe OUD.
- Buprenorphine (e.g., Suboxone): A partial opioid agonist that also reduces cravings and withdrawal but has a lower overdose risk due to a “ceiling effect.” It can be prescribed in an office setting.
- Naltrexone (e.g., Vivitrol): An opioid antagonist that blocks the effects of opioids. It is non-addictive but requires a person to be fully opioid-free for 7-10 days before starting.
| Feature | Methadone | Buprenorphine (e.g., Suboxone) | Naltrexone (e.g., Vivitrol) |
|---|---|---|---|
| Type | Full Opioid Agonist | Partial Opioid Agonist | Opioid Antagonist |
| How it Works | Eliminates withdrawal, reduces cravings, prevents euphoria (at stable dose) | Reduces cravings and withdrawal, has a “ceiling effect” for safety | Blocks opioid effects (no high), non-addictive, no physical dependence |
| Administration | Daily liquid, dispensed at specialized clinics | Daily sublingual film/tablet, monthly injection | Daily oral pill, monthly injection |
| Physical Dependence | Yes (if stopped abruptly, withdrawal occurs) | Yes (if stopped abruptly, withdrawal occurs) | No |
| Overdose Risk | Higher if misused or combined with depressants | Lower due to ceiling effect, safer than methadone if misused | None (blocks effects, does not cause overdose) |
| Starting Treatment | Can start immediately, even with active opioid use | Must be in mild-to-moderate withdrawal to avoid precipitated withdrawal | Must be opioid-free for 7-10 days to avoid precipitated withdrawal |
| Benefits | Highly effective for severe OUD, long history of success | Can be prescribed by certified doctors in office settings, lower overdose risk | No risk of dependence, good for individuals committed to abstinence |
| Downsides | Daily clinic visits, strict regulations | Can be diverted, requires special training for prescribers (historically) | Less effective for severe cravings, requires full detox beforehand |
For more information, explore our Addiction Helpline America MAT Resources.
The Critical Role of Counseling and Behavioral Therapies
Medication stabilizes the brain, but therapy teaches new ways to live. Counseling helps address the root causes of addiction and builds coping skills for long-term recovery.
- Cognitive Behavioral Therapy (CBT) helps identify and change negative thought patterns and behaviors related to drug use.
- Individual and Group Therapy provide safe spaces to process trauma, learn from peers, and reduce the isolation of addiction.
- Family Therapy helps repair relationships and teaches family members how to support recovery effectively. We offer Resources for Families of Addicts to aid this process.
These therapies build essential skills in stress management and emotional regulation. For more details, see our Behavioral Therapy Resources.
Tailoring Opioid Addiction Solutions for Unique Needs
Effective treatment must be custom to the individual.
- Co-occurring Mental Health Disorders: Depression, anxiety, and PTSD are common with OUD. Integrated treatment that addresses both addiction and mental health simultaneously is most effective. Finding the Best Mental Health Treatment Near Me is a critical step.
- Chronic Pain Management: For those who developed OUD from pain prescriptions, treatment must balance pain management and recovery. This involves exploring non-opioid alternatives like physical therapy and CBT for pain. Our Comprehensive Pain Treatment Resources can help.
- OUD in Pregnancy: Untreated OUD can harm both parent and baby. MAT with methadone or buprenorphine is the safe, recommended standard of care during pregnancy, improving outcomes for both. We provide specialized OUD in Pregnancy Support.
Prevention, Support, and Long-Term Recovery
Comprehensive opioid addiction solutions extend beyond treatment to include prevention and long-term support systems for sustained recovery.
Primary Prevention Strategies
Preventing addiction before it starts is key. This includes:
- Safer Prescribing Practices: Healthcare providers are adopting stricter guidelines for prescribing opioids and discussing risks with patients.
- Non-Opioid Pain Alternatives: Physical therapy, acupuncture, and cognitive behavioral therapy for pain are effective alternatives that avoid addiction risk.
- Community Prevention: Education programs in schools and communities teach about opioid dangers, safe medication storage, and proper disposal of unused prescriptions.
The Role of Family and Friends
Support from loved ones is a powerful factor in recovery. Family and friends can help by:
- Educating themselves about OUD as a medical condition to approach the situation with empathy.
- Encouraging treatment by expressing concern and offering to help find resources.
- Creating a supportive environment while setting healthy boundaries to protect their own well-being.
- Seeking their own support through groups like Al-Anon or Nar-Anon. Our Resources for Families of Addicts can also provide guidance.
Long-Term Recovery
Recovery is a lifelong journey, not a one-time event. Sustained success often involves:
- Peer Support: Connecting with specialists who have lived experience with recovery provides invaluable mentorship and hope.
- Sober Living Environments: These structured homes bridge the gap between intensive treatment and independent living. Learn more about Sober Living.
- Ongoing Support: Continued therapy and participation in support groups like Narcotics Anonymous reinforce coping skills and provide accountability.
- Life Skills Development: Rebuilding a life includes finding employment, managing finances, and repairing relationships.
Latest Research Initiatives
The field of addiction treatment is constantly evolving. The NIH HEAL (Helping to End Addiction Long-term®) Initiative is a major research effort developing new, non-addictive pain treatments and improving access to care, offering hope for even more effective solutions in the future.
Frequently Asked Questions about Opioid Addiction
Is treatment for opioid addiction effective?
Yes, treatment is effective. Opioid Use Disorder is a chronic disease, like diabetes, that requires ongoing management rather than a one-time cure. Relapse can be part of the process and does not mean treatment has failed.
Success is measured not just by reduced substance use, but also by improved quality of life, including better physical and mental health, stable housing, and repaired relationships. Most importantly, evidence-based treatment—especially Medication-Assisted Treatment (MAT)—dramatically reduces the risk of fatal overdose. The key is a customized approach that combines medication, counseling, and support. For more details, see our page on Addiction Treatment Success Rates.
How long does rehab for opioid addiction take?
There is no one-size-fits-all answer. The duration of treatment for opioid addiction solutions is highly individualized and depends on the severity of the OUD, co-occurring mental health conditions, and other personal factors.
While programs are often offered in 30, 60, or 90-day increments (with longer stays generally leading to better outcomes), treatment should be viewed as a continuum of care. This may involve stepping down from an inpatient program to outpatient care, and then to ongoing therapy and support groups. Recovery is a long-term journey, and the length of formal rehab is just one part of it. To learn more about program lengths, visit our page How Long is Rehab?.
Do medications for OUD just replace one addiction with another?
No. This is a common and dangerous myth. When used as prescribed, medications like methadone and buprenorphine do not create a new addiction. They are therapeutic tools that manage the disease of addiction.
At proper doses, these medications do not produce a “high.” Instead, they work by stabilizing brain chemistry, eliminating withdrawal symptoms, and reducing cravings. This alleviates the physical compulsion to use illicit opioids, allowing the individual to feel normal and fully engage in counseling and other aspects of recovery. As SAMHSA confirms, these medications help patients manage their addiction so they can recover. For more information, you can visit the SAMHSA website.
Conclusion: Your Path to Recovery Starts Today
We’ve covered the scope of the opioid crisis and, more importantly, the proven opioid addiction solutions that offer real hope. From emergency overdose response with naloxone to the gold standard of Medication-Assisted Treatment and counseling, we’ve seen that a comprehensive, individualized approach works.
Recovery is absolutely possible. It requires courage, but you do not have to face this journey alone. Taking the first step is often the hardest, but support is available right now, whether you are seeking help for yourself or a loved one.
At Addiction Helpline America, we provide free, confidential guidance to help you find a treatment program that fits your unique needs. Our nationwide network of trusted providers offers the full spectrum of care, including medically supervised detox, MAT, dual diagnosis care, and long-term support. We are here to listen and connect you with quality care in your area.
Your path to a healthier, more hopeful future starts with a single conversation. Let us help you take that first step.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.