Showing Interventions for Conduct Disorder
For families facing the challenges of conduct disorder (CD), understanding available interventions for conduct disorder is a critical step toward healing. CD is not just “bad behavior”; it’s a mental health condition defined by a persistent pattern of violating others’ rights or major societal rules through aggression, destruction, deceit, or rule-breaking.
Early intervention is vital, as untreated CD can lead to severe long-term issues. Up to 40% of diagnosed children are at higher risk of developing antisocial personality disorder in adulthood.
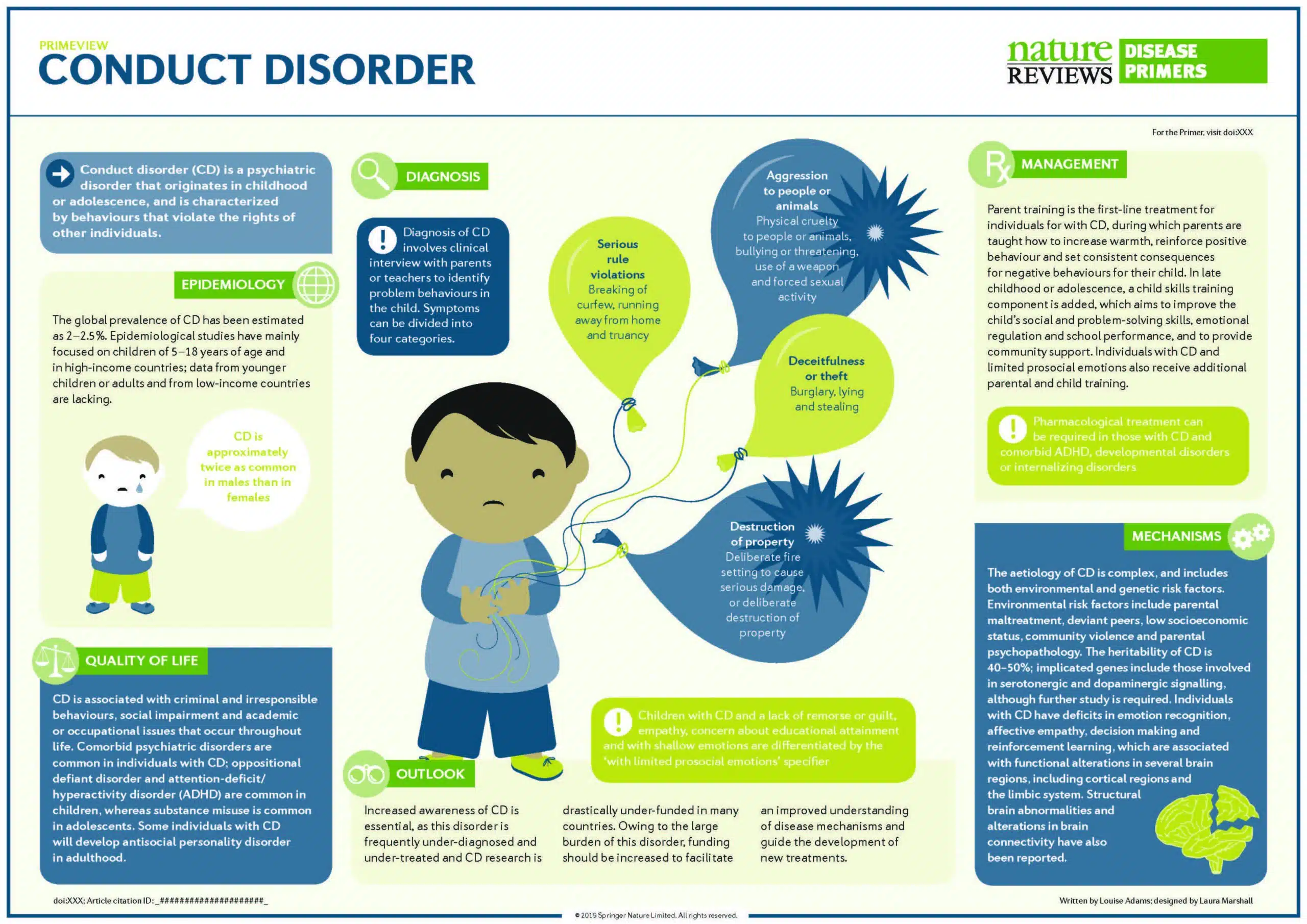
Primary interventions include:
- Psychosocial Interventions: Evidence-based therapies like Multisystemic Therapy (MST) and Functional Family Therapy (FFT).
- Parent Management Training (PMT): Teaches parents effective behavior management strategies.
- Pharmacotherapy: Medication used for co-occurring conditions like ADHD, not for CD directly.
- Community-Based Treatment: Includes therapeutic schools and structured community programs.
These interventions address CD’s multifaceted nature by involving children, families, schools, and communities. The goal is to treat the underlying condition, not just label the behavior.
Addiction Helpline America provides compassionate guidance for families impacted by complex behavioral challenges. We help connect those in need with vital resources and effective interventions for conduct disorder.
Quick interventions for conduct disorder terms:
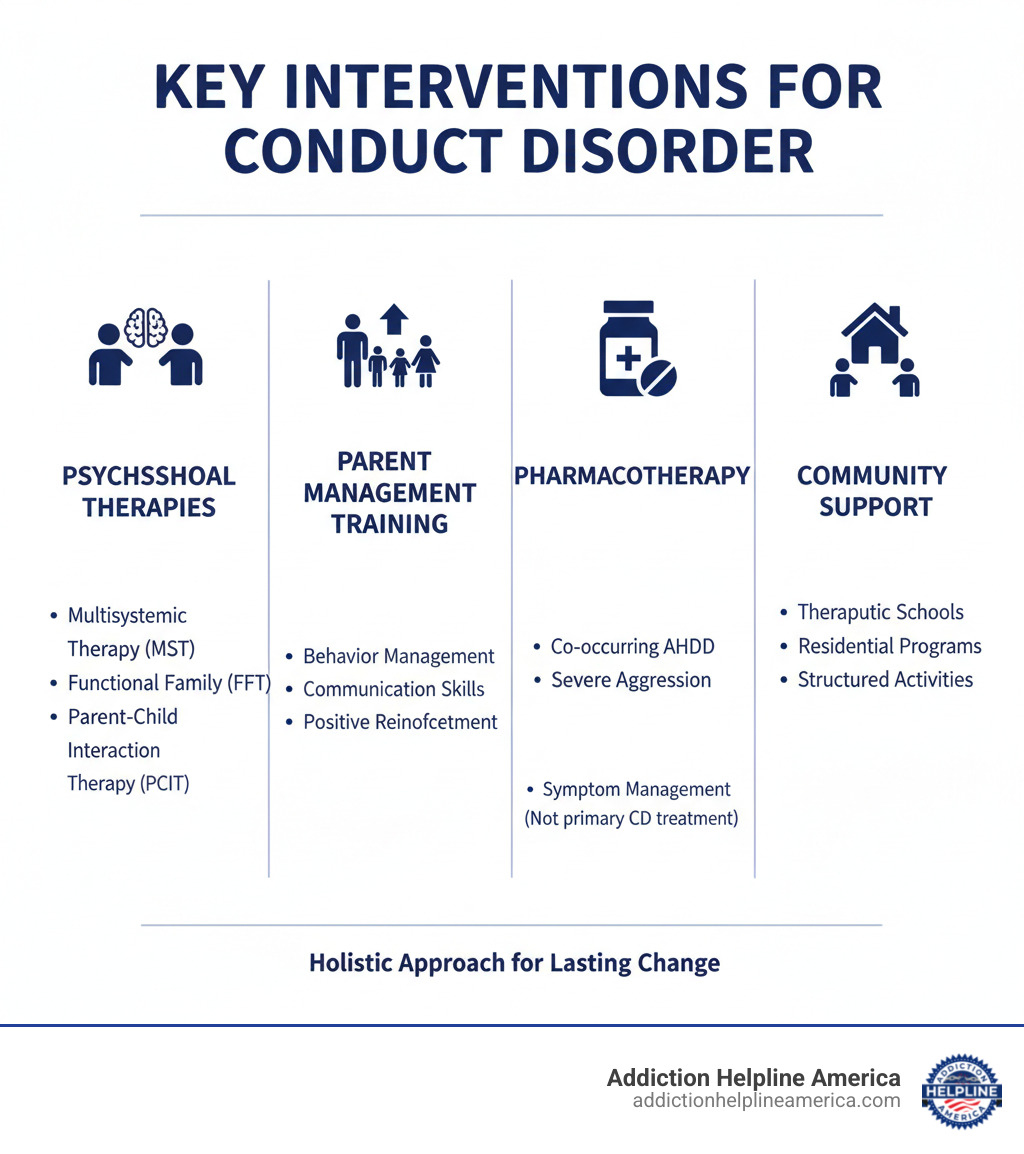
Decoding Conduct Disorder: Symptoms, Causes, and Diagnosis
When a child’s disruptive behaviors go beyond typical defiance, they may point to conduct disorder (CD). This mental health condition involves a persistent, repetitive pattern of violating the rights of others or major age-appropriate rules, causing significant problems at home, school, and in social settings.
Behavioral Categories
Experts group CD behaviors into four main categories. A diagnosis requires a consistent pattern over at least 12 months, causing significant impairment.
- Aggression to people and animals: Bullying, threatening, starting physical fights, using weapons, or being physically cruel.
- Destruction of property: Deliberately setting fires or otherwise destroying others’ property.
- Deceitfulness or theft: Breaking into homes or cars, lying to get things or avoid obligations, or shoplifting.
- Serious rule violations: Staying out late despite parental rules, running away from home, or frequent truancy from school.
Potential Causes
Conduct disorder rarely has a single cause; it’s usually a mix of factors.
- Genetic vulnerability: A child may inherit a temperament prone to impulsivity. A family history of mood disorders, ADHD, or substance use disorder increases risk.
- Environmental factors: Growing up in a home with abuse, neglect, or significant conflict can contribute. Living in high-crime neighborhoods or having inconsistent discipline are also risk factors.
- Brain differences: Some studies suggest individuals with CD may have differences in the frontal lobe, which controls impulse management and decision-making.
For a deeper look at the science, you can explore Scientific research on the diagnosis of Conduct Disorder.
Differentiating Conduct Disorder from Oppositional Defiant Disorder (ODD)
Conduct disorder is often confused with oppositional defiant disorder (ODD), but CD is more severe. ODD involves a pattern of angry/irritable moods and defiant behavior toward authority figures, but it does not typically involve violating the basic rights of others. CD, however, is defined by such violations.
| Feature | Oppositional Defiant Disorder (ODD) | Conduct Disorder (CD) |
|---|---|---|
| Core Characteristics | Pattern of angry/irritable mood, argumentative/defiant behavior, vindictiveness. | Persistent pattern of violating basic rights of others or major societal norms/rules. |
| Severity | Less severe; primarily directed at authority figures, verbal aggression. | More severe; involves physical aggression, destruction, deceit, and serious rule-breaking. |
| Violation of Rights | Does not involve violating the basic rights of others. | Involves violating the basic rights of others (e.g., bullying, theft, physical cruelty). |
| Legal Implications | Less likely to lead to legal trouble, though conflicts with authority are common. | High likelihood of involvement with the juvenile justice system and criminal behavior. |
| Empathy/Remorse | May show remorse, but primarily focused on resisting authority. | Often characterized by a lack of empathy, guilt, or remorse for their actions. |
| Developmental Pathway | Can be a precursor to CD; approximately 30% of children with ODD may develop CD. | Often develops after ODD, but can also have an independent onset. |
The key difference is that ODD is about defiance toward authority, while CD involves more serious antisocial acts that harm others.
The Impact of Age of Onset
When CD behaviors first appear affects the prognosis and guides interventions for conduct disorder.
Childhood-onset (before age 10) is considered more severe. These children may show more physical aggression and are at higher risk for developing antisocial personality disorder as adults. This type requires more intensive, long-term family therapy.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Adolescent-onset (after age 10) tends to involve less physical aggression and has a somewhat better outlook. Treatment may focus more on peer relationships and problem-solving skills, with continued family support. Understanding the onset helps tailor the most effective interventions for conduct disorder.
The Web of Comorbidity: How Co-Occurring Conditions Impact Treatment
Conduct disorder is frequently intertwined with other mental health conditions, a factor that significantly impacts treatment. A child with CD may struggle with one or more other disorders at the same time, creating a complex clinical picture.

Common Comorbidities
Several conditions commonly co-occur with conduct disorder:
- Attention-Deficit/Hyperactivity Disorder (ADHD): The impulsivity from ADHD can worsen CD symptoms, making it harder for children to control aggressive behaviors.
- Mood Disorders: Depression and bipolar disorder can contribute to the irritability and emotional outbursts seen in CD.
- Anxiety Disorders: High anxiety can manifest as irritability or aggression, especially if a child lacks healthy coping skills.
- Substance Use Disorders: Early substance use is strongly linked to CD and increases the risk of future personality disorders and violent crime.
- Post-Traumatic Stress Disorder (PTSD): Trauma is a major risk factor for CD, and PTSD symptoms like angry outbursts can overlap with or worsen CD behaviors.
Impact on Treatment
Co-occurring conditions deeply influence interventions for conduct disorder. A key best practice is to identify and treat these other conditions, particularly ADHD, as a first step. Behavioral therapies for CD are often more effective after symptoms of comorbid disorders are managed.
This complexity requires a personalized and integrated treatment plan. For example, a child might need medication for ADHD, therapy for anxiety, and specific behavioral interventions for CD. Addressing all connected issues is vital for lasting success.
For those facing the dual challenge of addiction and mental health issues like CD, we offer support. We understand this complex link and can help you find resources. For more information, visit our page on Addiction and Mental Health.
First-Line Psychosocial Interventions for Conduct Disorder
Psychosocial interventions are the leading first-line treatment for conduct disorder. These methods focus on the psychological, social, and environmental factors influencing a child’s behavior to create lasting change. Experts, including those at the National Institute for Health and Care Excellence (NICE), recommend a family-focused approach using evidence-based therapies. You can explore these guidelines at NICE guidelines on interventions for conduct disorders.
Successful programs often involve the family and community, such as Multisystemic Therapy (MST), Functional Family Therapy (FFT), The Incredible Years, and Parent-Child Interaction Therapy (PCIT). The core idea is that helping a child with CD is a team effort.
The Central Role of Parent Management Training (PMT)
Among the most effective interventions for conduct disorder, Parent Management Training (PMT) empowers parents with practical skills to create a positive and structured home environment.
PMT typically involves:
- Improving Parenting Skills: Learning to identify target behaviors and promote positive ones.
- Positive Reinforcement: Using praise and rewards to motivate better choices.
- Consistent Discipline: Setting clear rules and using fair, predictable consequences.
- Reducing Harsh Punishment: Moving away from punitive measures that can worsen defiance.
- Improving Parent-Child Relationships: Strengthening the family bond through positive communication and shared activities.
By giving parents these tools, PMT helps build a stable and loving environment where children can learn to manage their actions more effectively.
Individual and Group Therapy Approaches
Individual and group therapies are also crucial, focusing directly on helping the child build inner skills.
- Cognitive Behavioral Therapy (CBT): Helps young people recognize and change negative thought patterns that lead to aggressive behavior.
- Anger Management Training: Teaches children to spot anger triggers and use calming strategies.
- Problem-Solving Skills Training: Equips children with a step-by-step method for handling difficult situations without acting impulsively.
- Social Skills Development: Helps children learn to listen, show empathy, cooperate, and steer social interactions.
- Peer Group Therapy: Offers adolescents a safe space to practice new social skills and get feedback from peers.
These therapies empower the child with the mental and emotional tools needed for lasting behavioral change, working hand-in-hand with family-based interventions.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Building a Comprehensive Treatment Plan
An effective treatment plan for conduct disorder is a multifaceted puzzle, bringing together different pieces of a child’s world: their individual needs, family, school, and community.
A Multifaceted and Supportive Approach
A helpful plan integrates several key components:
- Individual and Family Therapy: One-on-one therapy helps a child build skills like anger management, while family therapy, especially Parent Management Training (PMT), creates a safe and structured home environment.
- School-Based Support: Close collaboration with teachers is key. This may involve an Individualized Education Program (IEP) or in-class behavior plans to ensure consistency between home and school.
- Community Involvement: Structured activities like sports, clubs, or mentoring programs offer safe spaces and teach teamwork. For more severe cases, therapeutic schools or residential treatment centers provide a higher level of support.
The Role of Pharmacotherapy
Medication, or pharmacotherapy, is not a cure for CD but can be a helpful part of a broader strategy. There are no FDA-approved medications specifically for conduct disorder. Instead, medication is used to treat co-occurring conditions that often accompany CD:
- Stimulants can be effective for co-occurring ADHD, helping to reduce impulsivity.
- Antidepressants may be used for co-occurring mood or anxiety disorders to help stabilize mood.
- In rare cases of severe aggression, atypical antipsychotics might be considered short-term. For guidance on related mental health issues, see our page on finding a Therapist for Depression and Anxiety.
Any decision about medication should be made by a qualified professional as part of a comprehensive plan that prioritizes psychosocial therapies.
Challenges and Long-Term Outcomes
Treating conduct disorder can be challenging. A child’s distrust of adults or lack of cooperation can make therapy difficult, requiring patience and persistence from professionals.
However, the consequences of forgoing interventions for conduct disorder are serious. If left untreated, a young person faces a higher risk of:
- Antisocial Personality Disorder (ASPD) in adulthood (up to 40% of cases).
- Substance abuse and addiction.
- Criminal behavior and involvement with the justice system.
- Other mental health problems like depression and anxiety.
- Social and occupational difficulties, including trouble maintaining relationships and employment.
These risks highlight why early and comprehensive intervention is so critical for guiding young people toward a brighter future.
Frequently Asked Questions about Conduct Disorder Interventions
Families often have questions about conduct disorder. Here are answers to some common inquiries.
What is the difference between conduct disorder and normal teenage rebellion?
While teenage rebellion is a normal, temporary phase of testing boundaries, conduct disorder (CD) is a serious mental health condition. The key differences are severity and impact. CD involves a persistent and severe pattern of behavior that violates the rights of others (e.g., aggression, theft, cruelty) and causes significant impairment in a child’s social and academic life. Rebellion is less intense and does not typically involve such serious harm or dysfunction.
Can conduct disorder be “cured”?
The term “cure” can be misleading for mental health conditions. However, with early and comprehensive interventions for conduct disorder, many individuals learn to manage their behaviors, develop prosocial skills, and lead successful adult lives. The goal of treatment is to equip them with the tools to function effectively and build healthy relationships, preventing the severe long-term consequences of untreated CD.
Is medication always necessary for treating conduct disorder?
No. Medication is not a first-line or standalone treatment for CD itself. The primary and most effective interventions for conduct disorder are psychosocial therapies like Parent Management Training (PMT) and Cognitive Behavioral Therapy (CBT).
Medication is typically used as a supportive tool to:
- Treat co-occurring conditions like ADHD or depression, which can make CD symptoms worse.
- Manage severe aggression that has not responded to other therapies.
Any decision to use medication is made carefully by a professional as part of a comprehensive treatment plan.
Conclusion: Finding a Path Forward
A diagnosis of conduct disorder can feel daunting, but there is a clear message of hope: effective interventions for conduct disorder offer a path forward. As we’ve explored, early, comprehensive support that involves the family, school, and community is crucial for positive change.
The journey may have challenges, such as a child’s distrust or lack of cooperation. However, consistent treatment offers significant hope for improvement. Children can learn to manage their behavior, build social and emotional skills, and avoid the serious long-term risks of untreated CD, like antisocial personality disorder or substance abuse.
Addiction Helpline America is here to stand by your family. We offer confidential guidance and can connect you with trusted resources and treatment centers nationwide. You don’t have to steer these challenges alone. Let us help you Find the right types of treatment programs for your needs custom to your family’s situation.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.















