Understanding Your Path to Recovery: The IOP Solution
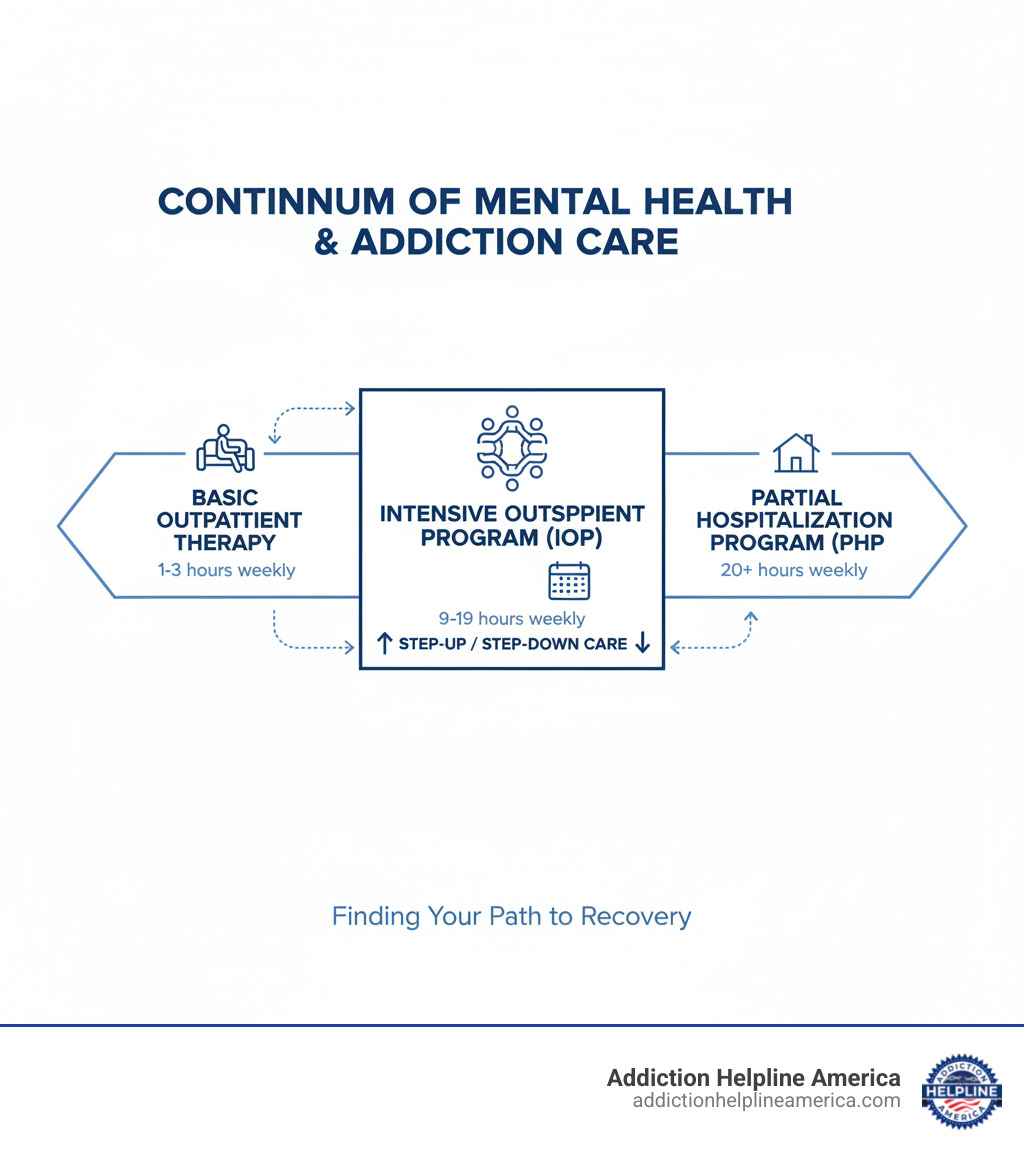
An intensive outpatient program is a structured treatment option that bridges the gap between basic outpatient therapy and residential care, offering 9-19 hours of weekly programming while allowing you to maintain your daily responsibilities at home.
Quick Answer: What is an Intensive Outpatient Program?
- Structure: 3-5 days per week, 3-4 hours per session
- Duration: Typically 4-12 weeks, sometimes longer based on individual needs
- Treatment: Combines individual therapy, group sessions, and family involvement
- Flexibility: Live at home while receiving intensive support
- Ideal for: Those needing more than weekly therapy but not 24-hour care
When you’re struggling with addiction or mental health challenges, finding the right level of care can feel overwhelming. You might wonder if weekly therapy sessions are enough, or if residential treatment is your only option for intensive support.
The truth is, there’s a middle ground that works for many people. IOPs have grown dramatically – from serving 1.2 million people in 2010 to 1.4 million by 2019, with nearly 16,000 facilities now offering these programs across the United States.
Research consistently shows that IOPs can be just as effective as inpatient treatment for many individuals with substance use disorders. This means you can get the intensive care you need without leaving your family, job, or support system behind.
At Addiction Helpline America, we’ve helped countless individuals and families steer their recovery journey through various treatment options, including intensive outpatient programs that provide the perfect balance of structure and flexibility. Our experience has shown us that IOPs often serve as a crucial stepping stone in the recovery process, offering hope when other approaches haven’t worked.
Understanding the IOP Model: Structure and Components
An intensive outpatient program is a structured, non-residential treatment program for mental health or substance use issues that don’t require 24/7 supervision. It blends intensive therapeutic support with the flexibility to maintain your daily life, acting as a bridge between weekly therapy and full-time residential care.
IOPs serve as both a “step-down” from inpatient care and a “step-up” when weekly therapy isn’t enough. The core services include group therapy, individual counseling, family involvement, and educational components that work together to build long-term coping skills.
First developed in the 1980s for professionals who couldn’t take time off for residential treatment, IOPs became more accessible in the 1990s. Their growth has been significant, with nearly 16,000 facilities serving 1.4 million people by 2019, showing how these programs have evolved to meet diverse community needs.
Typical Structure of an Intensive Outpatient Program
The word “intensive” reflects a serious time commitment beyond a typical weekly therapy session. Here’s a general overview:
- Time Commitment: Most programs require 9 to 19 hours per week. Adults typically commit to at least 9 hours, while adolescent programs may start at 6 hours.
- Schedule: Attendance is usually 3 to 5 days per week, with each session lasting 3 to 4 hours. Many programs offer evening or weekend options to accommodate work or school.
- Program Length: Most IOPs run 4 to 12 weeks, though some may extend longer for complex needs.
- Individual Therapy: One-on-one sessions provide a private space to work through personal challenges and develop customized coping strategies.
- Group Therapy: This is the backbone of most IOPs, offering a supportive environment to share experiences, learn from peers, and practice new skills.
- Family Involvement: Quality IOPs often include family therapy or educational workshops to help loved ones understand how to support the recovery process.
Key Components and Activities
IOPs offer a variety of therapeutic activities to provide real-world tools for lasting recovery.
- Psychoeducational Groups: Interactive discussions provide valuable information about mental health conditions, addiction, relapse prevention, and healthy lifestyles.
- Skills Development: You’ll learn practical strategies for emotional regulation, distress tolerance, interpersonal effectiveness, and mindfulness, often drawn from Dialectical Behavior Therapy (DBT) and Cognitive Behavioral Therapy (CBT).
- Relapse Prevention: For substance use issues, this is a major focus. You’ll identify triggers, develop coping mechanisms, and create a detailed prevention plan.
- Medication Support: Psychiatric services are available to evaluate, prescribe, and monitor medications when needed.
- Case Management: A case manager coordinates services, connects you with community resources, and helps develop a solid aftercare plan.
- Complementary Therapies: Many programs incorporate trauma-informed yoga, art therapy, or mindful movement to offer different pathways for healing. Some may also offer advanced treatments like ketamine when clinically appropriate.
IOP and Levels of Care: Finding the Right Fit
Understanding where an intensive outpatient program fits within the spectrum of care is key to finding the right support. Treatment options range from weekly therapy to 24/7 hospital care, with IOPs providing a middle ground of intensive support without requiring you to leave your life behind.
Healthcare professionals use criteria from the American Society for Addiction Medicine (ASAM) to determine the appropriate level of care based on symptom severity, co-occurring health issues, and readiness for treatment. IOPs are highly flexible, serving as a step-down from inpatient care or a step-up from weekly therapy.
You may be a good fit for an intensive outpatient program if you have moderate to severe symptoms but also a stable and supportive home environment. The ideal candidate is motivated to participate in recovery and can manage daily responsibilities without constant medical supervision.
Making the right choice isn’t something you have to do alone. At Addiction Helpline America, we help you understand your options and connect you with the right level of care.
How IOP Differs from Other Treatment Options
Understanding how an intensive outpatient program compares to other options highlights why it might be the perfect fit. Each level of care serves different needs, and finding the right match is crucial for recovery.
| Feature | Traditional Outpatient Therapy | Intensive Outpatient Program (IOP) | Partial Hospitalization Program (PHP) | Inpatient/Residential Care |
|---|---|---|---|---|
| Hours/Week | 1-3 hours | 9-19 hours | 20+ hours (often 25-35 hours) | 24/7 care |
| Living Situation | Lives at home | Lives at home | Lives at home | Lives at facility |
| Support Level | Minimal, individual sessions | Structured, frequent group/individual | Highly structured, daily sessions | Constant supervision, highest support |
| Ideal Candidate | Mild symptoms, stable, good coping | Moderate symptoms, stable home, needs more structure than outpatient, can manage daily life | Acute symptoms, needs daily structure to avoid inpatient, but safe at home overnight | Severe symptoms, needs detox, unsafe at home, requires 24/7 monitoring |
IOPs offer intensive care without intensive disruption. You get structured support and a therapeutic community while sleeping in your own bed and maintaining daily responsibilities.
Research confirms this approach. A comprehensive study found that intensive outpatient programs are often as effective as inpatient treatment for most people with alcohol or drug use disorders. This means you can get excellent care while maintaining important connections and routines. Evidence on IOP effectiveness shows how these programs consistently deliver real results. The key difference is flexibility, offering a middle ground where healing happens alongside living.
Who Benefits from an Intensive Outpatient Program and What Does It Treat?
An intensive outpatient program can be an ideal solution if you need serious support but want to maintain your daily life. It’s designed for individuals who need more than weekly therapy but don’t require 24/7 care.
The ideal candidate for an IOP typically has a stable living situation and a support system of family or friends. A key factor is being motivated for change and willing to participate in group settings. IOPs are appropriate for those who do not require medical detox and are not an immediate danger to themselves or others; in those cases, a higher level of care is necessary first.
IOPs provide a therapeutic environment that is intensive enough to create meaningful change while being flexible enough to accommodate work, school, or family responsibilities.
Common Conditions and Disorders
Intensive outpatient programs are versatile and effective for a wide range of challenges.
- Substance Use Challenges: IOPs are highly effective for alcohol, prescription medication, or other drug concerns, especially for those with mild to moderate issues who have completed any necessary detox.
- Mental Health Needs: They provide structured support for managing conditions like depression, anxiety, and bipolar disorder.
- Eating Disorders: Specialized IOPs offer structured meal support, body image work, and therapy to address underlying emotional factors.
- PTSD and Trauma: Trauma-informed IOPs provide a safe environment and specialized approaches for healing from traumatic experiences.
- Personality Disorders: Research shows IOPs can be effective for complex conditions like Borderline Personality Disorder, with one study highlighting the benefits of intensive group work and skills training. You can read more here: A study on IOP for BPD.
Specialized IOPs for Unique Needs
The intensive outpatient program model is adaptable to meet specific needs, ensuring you receive care designed for your situation.
- Dual Diagnosis Support: These IOPs treat co-occurring mental health and substance use conditions simultaneously, which leads to better long-term outcomes. You can work on your depression and your drinking together.
- Adolescent-Focused Programs: These programs address the unique challenges of teenagers, such as peer pressure, family dynamics, and academic stress, with age-appropriate methods and slightly different time commitments (often starting at 6 hours per week).
- Support for Professionals: Many IOPs continue to serve professionals with demanding careers, allowing them to maintain job responsibilities while receiving intensive help.
- Gender-Responsive Care: These programs create safe, same-gender spaces where men and women can address sensitive issues without additional social pressures.
At Addiction Helpline America, we know the right fit matters. We’re here to help you find a specialized IOP that understands your unique needs.
The Road to Recovery: Therapeutic Approaches and Family Involvement
Successful intensive outpatient programs are built on evidence-based practices and individualized care plans. Treatment is custom to your specific needs and goals, focusing on building coping skills that provide the tools to thrive long after the program ends.
Common Therapeutic Modalities Used in IOPs
IOPs use a variety of proven therapeutic approaches:
- Cognitive Behavioral Therapy (CBT): Helps you identify and change negative thought patterns and behaviors. The IOP setting allows you to practice these new skills in your daily life immediately.
- Dialectical Behavior Therapy (DBT): Teaches essential skills for managing intense emotions, including mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness.
- Motivational Interviewing: A collaborative approach that helps you find your own motivation for change, meeting you where you are in your recovery journey.
- Group Therapy: The core of many IOPs, providing a safe space to share experiences, learn from peers, and practice new communication skills on topics like relapse prevention and problem-solving.
- 12-Step Facilitation: Many IOPs introduce the principles of 12-Step programs like AA or NA, bridging formal treatment with community-based support.
- Trauma-Informed Care: Specialized approaches like EMDR (Eye Movement Desensitization and Reprocessing) are often integrated to help process traumatic memories safely. You can learn more in the comprehensive SAMHSA guide on clinical issues in IOP.
The Crucial Role of Family Involvement
Recovery is not a solo journey. Effective intensive outpatient programs recognize that involving family significantly improves the chances of lasting success.
- Family Therapy and Education: Guided sessions and workshops help families understand the impact of addiction or mental health issues on the entire family system. They learn about the recovery process and how to provide support without enabling.
- Rebuilding Trust and Communication: IOPs provide a structured environment for families to have honest conversations, work through conflicts, and learn healthier communication skills. This process is vital for rebuilding trust.
- Creating a Supportive Home: Since you live at home during an IOP, family involvement is key to creating a home environment that nurtures recovery. When your family understands your goals, they can become your strongest allies.
Call Our 24/7 Free & Confidential Helpline for Addiction Support
Starting an intensive outpatient program begins with a comprehensive assessment to create a personalized treatment plan. This roadmap outlines the therapeutic approaches, group topics, and individual support you’ll receive. During the program, you’ll learn and practice new coping skills in real-world situations.
Completing the program isn’t the end; it’s a transition. You’ll graduate with a strong aftercare plan to help turn short-term progress into lasting change.
How to Find and Choose the Right Intensive Outpatient Program
Finding the right intensive outpatient program is a critical step.
- Seek Referrals: Your primary care doctor, therapist, or psychiatrist can provide trusted recommendations.
- Use Online Resources: The Substance Abuse and Mental Health Services Administration (SAMHSA) has a treatment locator at findtreatment.samhsa.gov/locator. Organizations like the National Alliance on Mental Illness (NAMI) also offer resources.
- Ask Key Questions: When contacting programs, inquire about their duration, time commitment, treatment philosophy (CBT, DBT, etc.), staff qualifications, and accreditation.
- Clarify Costs: Get clear details on costs and insurance coverage upfront to avoid surprises.
The right program will feel like a supportive place where you can grow while maintaining important parts of your life.
Costs, Insurance, and Life After Treatment
Intensive outpatient programs are typically more affordable than residential treatment because they don’t include room and board.
- Insurance Coverage: Most insurance plans, including Medicare, Medicaid, and Tricare, are required to cover mental health and substance use treatment. Always call your provider to confirm your specific benefits, deductibles, and co-pays.
- Other Payment Options: If you lack insurance, many programs offer sliding-scale fees based on income or can connect you with state-funded options.
- Life After Treatment: Transitioning back to daily life is smoother with an IOP because you’ve been practicing skills at home all along. Before you finish, your team will create a solid aftercare plan, which may include ongoing individual therapy, support groups, or community resources. Many programs also have alumni networks for continued peer support.
Completing an IOP builds a strong foundation. Ongoing therapy or support groups often become a normal part of life, helping you maintain progress. At Addiction Helpline America, we can help you steer this journey and find the right program.
Conclusion
The intensive outpatient program represents a remarkable balance in modern mental health and addiction treatment. Throughout this guide, we’ve explored how IOPs offer something truly special – the intensive, structured support you need to heal, combined with the flexibility to keep living your life at home.
This unique approach has proven itself time and again. The flexibility to maintain your job, stay connected with family, and practice new skills in real-world situations makes recovery feel more achievable and sustainable. At the same time, the structured environment with 9-19 hours of weekly programming ensures you’re getting the intensive support necessary for meaningful change.
What makes IOPs particularly effective is their evidence-based foundation. From Cognitive Behavioral Therapy to Dialectical Behavior Therapy, from group sessions to family involvement, every component is designed to build lasting coping skills. The research backs this up – studies show that intensive outpatient programs can be just as effective as inpatient treatment for many people dealing with substance use and mental health challenges.
Whether you’re transitioning down from residential care, stepping up from weekly therapy, or starting your recovery journey fresh, an IOP can provide that crucial middle ground. It’s intensive enough to create real change, yet flexible enough to fit into your life as it is today.
Taking the first step toward treatment is never easy, but it’s also one of the bravest things you can do. Every person’s path to recovery looks different, and finding the right fit matters tremendously. That’s where we come in.
At Addiction Helpline America, we understand that choosing a treatment program can feel overwhelming. We’re here to provide free, confidential guidance to help you steer your options and find an intensive outpatient program that matches your unique needs and circumstances.
Recovery is possible, and you don’t have to figure it out alone. Find the right treatment program for you and take that important next step toward the healthier, more balanced life you deserve.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.