Understanding When Crisis Requires Immediate, Comprehensive Care
Inpatient behavioral health treatment provides 24-hour medical care in a secure hospital setting for individuals in a severe mental health crisis. This level of care is for people who pose a danger to themselves or others, experience acute psychiatric symptoms like psychosis or suicidal ideation, or have not improved with less intensive outpatient services.
Key Facts About Inpatient Behavioral Health:
- What it is: Round-the-clock psychiatric care in a hospital or specialized facility.
- Who it’s for: Adults, adolescents, or older adults in acute mental health crisis.
- Typical length: One week for adults; two weeks for children, adolescents, and older adults.
- Primary goal: Crisis stabilization and safety through intensive medical and therapeutic intervention.
- Common conditions treated: Severe depression, bipolar disorder, schizophrenia, suicidal thoughts, psychotic episodes, and co-occurring disorders.
When a loved one is in crisis—unable to care for themselves, hearing voices, or expressing suicidal thoughts—it’s natural to feel overwhelmed. Inpatient behavioral health care is a critical medical intervention for these moments, much like hospitalization for a physical emergency. It provides a safe, structured environment for expert evaluation, symptom stabilization, and a bridge to ongoing recovery.
This guide explains when inpatient care is necessary, what to expect during a stay, and how to steer aftercare and insurance. At Addiction Helpline America, we connect families to behavioral health resources, guiding them through the process of accessing inpatient treatment. Our mission is to provide clear, compassionate information to help you make informed decisions.
Inpatient behavioral health terms to remember:
- Mental health inpatient
- Inpatient treatment for depression and anxiety near me
- residential depression rehab
Understanding Inpatient Behavioral Health: A Foundation for Recovery
Inpatient behavioral health treatment is a specialized level of care where an individual receives round-the-clock medical attention in a secure, structured environment for mental health stabilization. It is an active, medically supervised program designed to bring acute symptoms under control, ensure safety, and create a clear path toward recovery.
The primary goal is crisis intervention and stabilization. Similar to how a hospital treats a broken leg, inpatient behavioral health addresses severe mental health crises. The treatment team works to calm acute symptoms—like suicidal thoughts or psychosis—in a safe space where healing can begin. This level of care includes 24-hour medical supervision from psychiatrists, nurses, and therapists, which is not possible in outpatient settings.
While sometimes used interchangeably, “inpatient” and “residential” treatment are different.
| Feature | Inpatient Behavioral Health Treatment | Residential Treatment |
|---|---|---|
| Duration | Short-term, a few days to two weeks, for rapid stabilization. | Longer-term, 30 days to several months, for sustained recovery. |
| Focus | Acute care, stabilization, and diagnosis for urgent mental health issues. | Addresses underlying issues and develops long-term coping strategies. |
| Origin | Stems from an urgent psychiatric crisis and danger to self/others. | Often follows inpatient care or is chosen for intensive, non-crisis treatment. |
For a deeper look, our guide on inpatient vs outpatient rehab breaks down the levels of care.
Conditions Treated in Inpatient Settings
Inpatient behavioral health facilities treat serious mental health conditions when symptoms become too severe to manage safely at home.
- Severe Depression: For those with complete hopelessness, inability to function, and thoughts of suicide or self-harm.
- Bipolar Disorder: To stabilize extreme mood swings, psychosis, or reckless behaviors during severe manic or depressive episodes.
- Schizophrenia and Psychotic Disorders: During acute episodes with overwhelming hallucinations, delusions, or disorganized thoughts that prevent self-care.
- Severe Anxiety Disorders: When conditions like Panic Disorder or OCD become so debilitating they lead to suicidal thoughts or a complete inability to function.
- Post-Traumatic Stress Disorder (PTSD): When severe flashbacks, dissociation, or hypervigilance make a person unsafe.
- Eating Disorders: For life-threatening medical complications from Anorexia, Bulimia, or Binge Eating Disorder, addressing both physical and psychological issues.
- Suicidal Ideation or Behavior: Any active thoughts, plans, or attempts at self-harm require immediate inpatient care for safety.
- Co-occurring Substance Use Disorders: Integrated treatment is needed when addiction and a mental health condition exist together. Learn more from our resource on dual diagnosis programs.
The Core Components of Inpatient Behavioral Health Treatment
“Active treatment” is an intensive, physician-supervised program where every element works toward recovery.
- Diagnostic Services: A thorough psychiatric evaluation upon admission to create an accurate diagnosis and treatment plan.
- Medication Management: Psychiatrists closely monitor medications, adjust dosages, and manage side effects daily.
- Individual Therapy: One-on-one sessions with a therapist to process the crisis and develop coping strategies.
- Group Therapy: Daily sessions with peers to share experiences, learn new skills, and reduce feelings of isolation.
- Family Therapy: Sessions involving loved ones (with permission) to improve communication and build a strong support system for after discharge.
- Therapeutic Activities: Art, music, or recreational therapies that offer alternative ways to express emotions and reduce stress.
- Milieu Therapy: The therapeutic environment itself—including the structured routine and supportive interactions—is designed to promote healing.
At Addiction Helpline America, we help families steer this landscape. We connect you with appropriate inpatient behavioral health facilities and help you understand what to expect.
Recognizing the Need: When Is Inpatient Care the Right Choice?
Deciding to seek inpatient behavioral health care is an overwhelming process, often made during a moment of crisis. It’s natural to question if it’s truly necessary. However, there are clear signs when the risk is too great and outpatient support is not enough.
Inpatient behavioral health care is the right choice when someone is in an acute mental health crisis that poses a danger to themselves or others, or when less intensive treatments have failed. It’s about recognizing the need for intensive, 24/7 support to get through a critical period safely.
Signs and Symptoms Warranting Hospitalization
The following red flags indicate that immediate, intensive care is needed:
- Danger to self or others: This is the most critical indicator. Any clear intent or behavior that puts the person or others at immediate risk requires hospitalization.
- Suicidal thoughts or behaviors: Active suicidal ideation, specific plans, or recent attempts demand 24-hour professional observation in a secure setting.
- Self-harm: Behaviors like cutting or burning indicate severe emotional pain and a need for immediate, intensive support.
- Assaultive or violent behavior: Threats or acts of violence require a structured, secure environment to protect everyone involved.
- Severe self-neglect: An inability to perform basic self-care, such as eating, maintaining hygiene, or taking essential medications.
- Psychotic episodes: Hallucinations (seeing or hearing things that aren’t there) or delusions (false beliefs) that impair judgment and safety.
Admission Criteria and Legal Considerations
Admission to an inpatient behavioral health unit is reserved for situations where it is medically necessary.
- Medical Necessity: A physician must determine that the patient requires 24-hour medical supervision and cannot be treated safely in a less restrictive setting.
- Voluntary Admission: This is the preferred method, where a person recognizes their need for help and provides informed consent for treatment.
- Involuntary Commitment: When a person is too unwell to recognize their need for help and poses a danger, state laws allow for involuntary hospitalization to ensure safety. A common tool is a 72-hour emergency hold, which permits immediate hospitalization for evaluation.
- Patient Rights: Even during involuntary commitment, patients retain rights to humane treatment and communication with attorneys and loved ones.
For more information on psychiatric facilities and patient rights, visit our resources page.
When to Go to the Emergency Room
Go to the ER immediately in these situations:
- Immediate danger of self-harm or harming someone else.
- Severe, unmanageable symptoms like acute psychosis or extreme agitation.
- A co-occurring medical emergency, such as an overdose or severe self-inflicted injury.
- A crisis hotline (like 988) advises you to go to the ER.
If you cannot safely transport the person, call 911. Emergency responders are trained to handle mental health crises. The ER can provide immediate stabilization and assess if inpatient behavioral health hospitalization is required. Acting decisively in a crisis can save a life.
A Day in the Life: What to Expect During an Inpatient Stay
An inpatient behavioral health facility is a safe, structured, and goal-oriented environment designed for healing. The predictable daily routine helps patients feel secure during a chaotic time.
A typical day is filled with therapeutic activities. After breakfast and morning medications, the day includes:
- Group therapy sessions focusing on skills from Cognitive Behavioral Therapy (CBT) or Dialectical Behavior Therapy (DBT).
- Individual therapy for confidential, one-on-one counseling.
- Family therapy sessions to help repair relationships and prepare loved ones for supporting recovery.
- Therapeutic activities like art, music, or recreation to help express difficult emotions.
- Quiet time for personal reflection and journaling.
Staff members are always present and available to offer support. The secure environment removes outside stressors, allowing patients to focus entirely on getting better. Active participation is key—the more you engage, the more you will benefit from the experience.
The Multidisciplinary Treatment Team
Inpatient care uses a team approach, with different specialists collaborating on your recovery.
- Psychiatrist: The medical doctor who leads the team, makes diagnoses, and manages medication.
- Psychiatric Nurses: Provide 24/7 care, administer medications, and monitor symptoms.
- Clinical Therapist/Counselor: Conducts individual and group therapy sessions.
- Social Worker: Focuses on discharge planning, connecting you to community resources, and facilitating family therapy.
- Occupational Therapist: Helps you regain daily living skills, from self-care to time management.
- Case Manager: Coordinates all aspects of your care, including communication with your insurance company.
This collaborative approach ensures all aspects of your well-being are addressed.
Typical Length of Stay and Influencing Factors
The average inpatient behavioral health stay for adults is about one week. Children, adolescents, and older adults may stay longer, often around two weeks.
The actual length of stay depends on several factors:
- Patient Progress: The primary factor is stabilizing acute symptoms to the point where you can safely transition to a lower level of care.
- Symptom Severity: More severe crises naturally require more time for stabilization.
- Co-occurring Conditions: Addressing both a mental health disorder and a substance use issue may extend the stay.
- Discharge Planning: A solid aftercare plan must be in place before you can be discharged safely.
Inpatient care focuses on acute stabilization. For longer-term rehabilitation, your team might recommend a 30-day inpatient program.
Supporting a Loved One in Inpatient Behavioral Health
Your support is vital. Here’s how you can help:
- Get Involved: Participate in family therapy and educational programs offered by the facility.
- Follow Policies: Respect the facility’s visiting hours and rules, which are designed to protect all patients’ recovery.
- Communicate with the Team: With your loved one’s consent (via a signed HIPAA form), you can speak with the care team. You can always provide them with helpful information, even without consent.
- Provide Emotional Support: Be positive and hopeful. Avoid discussing stressful topics from home.
- Take Care of Yourself: Supporting someone in crisis is draining. Seek your own support through therapy or support groups to remain a strong resource for your loved one.
The Journey Forward: Discharge, Aftercare, and Sustaining Progress
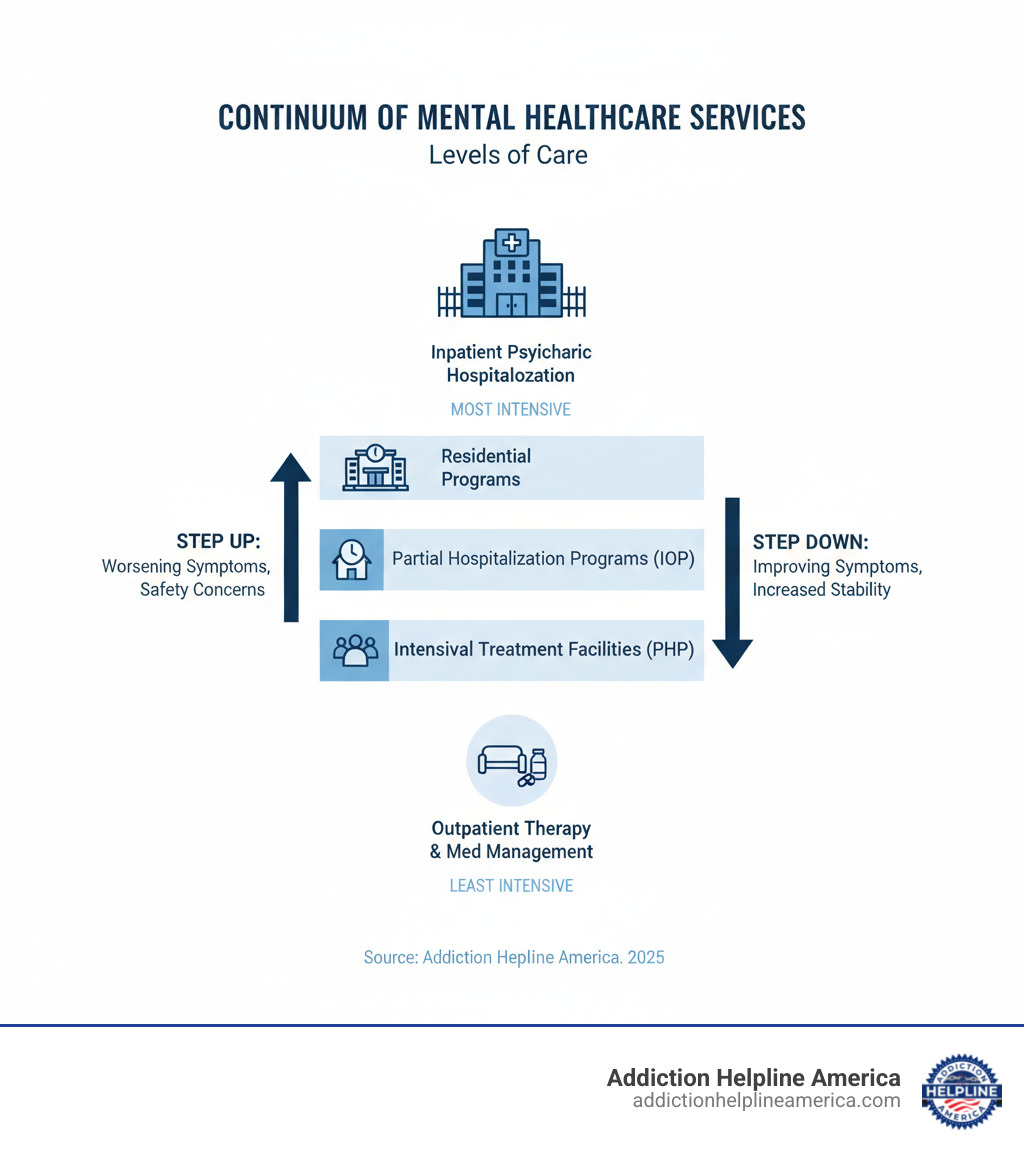
Leaving an inpatient behavioral health facility is the beginning of the next phase of your recovery. Discharge planning starts on day one, reflecting a “continuum of care” philosophy. The goal is to ensure you have all the support you need to succeed after you leave.
Discharge Criteria
Doctors know you’re ready to leave when you meet specific criteria:
- Clinical Stabilization: The most severe symptoms that led to hospitalization have significantly improved, and you are no longer in acute crisis.
- No Longer a Threat: The immediate safety concerns for yourself or others have been resolved.
- Ability to Function: You can manage basic self-care and have demonstrated the ability to use new coping skills.
- Secured Aftercare Plan: A concrete plan for continued treatment is in place. This is a requirement for discharge, ensuring a safe transition.
The Critical Role of Aftercare
What happens after the hospital is just as important as your stay. A strong aftercare plan is the scaffolding that supports long-term recovery. Key components include:
- Step-Down Programs: Partial Hospitalization Programs (PHPs) or Intensive Outpatient Programs (IOPs) provide structured therapy several days a week while you live at home.
- Outpatient Therapy: Regular sessions with a therapist (individual or group) serve as an ongoing anchor for your recovery.
- Support Groups: Peer-led groups from organizations like NAMI or MHA connect you with others who have similar experiences.
- Medication Follow-ups: Regular appointments with your psychiatrist are crucial for ensuring your medications remain effective.
- Community Resources: Your plan may also include connections to vocational training, housing assistance, or other practical supports.
Aftercare is where you integrate the progress made in the hospital into your daily life. At Addiction Helpline America, we can help you steer these next steps. For more information, visit our find help and support resources page.
Navigating Access to Care: Insurance, Costs, and Finding Help
Worrying about how to pay for inpatient behavioral health treatment can be a major barrier to getting help. Fortunately, there are many options available.
How Insurance and Payment Work
- Verifying Coverage: Call your insurance company to ask about your specific benefits for inpatient behavioral health, including your deductible, co-pay, and out-of-pocket maximum.
- Pre-authorization: Most insurance plans require the hospital to get approval before or shortly after admission to confirm the stay is medically necessary. The facility typically handles this process.
- Medicare and Medicaid: Medicare provides benefits for inpatient psychiatric hospitalization but has specific criteria and limits. Medicaid coverage varies by state but is a vital resource for many families.
- Payment Plans: If you are uninsured or underinsured, many facilities offer financial assistance or individualized payment plans. Always ask about your options.
Resources for Finding Treatment and Support
You don’t have to find the right facility alone.
- Addiction Helpline America: We connect individuals and families to mental health and addiction treatment centers nationwide. Our service is free, confidential, and personalized to help you find the right program. Reach us anytime at Addiction Helpline America.
- National Crisis Hotlines: For immediate crisis support, dial or text 988 to reach the Suicide & Crisis Lifeline 24/7.
- Local Community Mental Health Centers: These centers can provide assessments, referrals, and help you steer local resources.
- National Organizations:
We are here to help you understand your options and connect you to the right care.
Frequently Asked Questions about Inpatient Behavioral Health
What is the main goal of a short-term inpatient stay?
The primary goal is crisis stabilization. It provides intensive, 24/7 care in a secure environment to manage acute symptoms, ensure safety, and create a plan for continued treatment at a lower level of care. It’s about controlling immediate danger so ongoing recovery can begin.
Can I refuse medication during an inpatient stay?
Patient rights vary by state and admission status (voluntary vs. involuntary). If you are admitted voluntarily, you generally have the right to be involved in your treatment plan and discuss medication. However, in emergencies or under an involuntary commitment where a person is a danger to themselves or others, medication may be administered for safety, as determined by a physician.
What should I bring for an inpatient stay?
Facilities provide a specific list, but you should typically bring a few days’ worth of comfortable clothing (without drawstrings), basic toiletries in non-glass containers, and a list of your current medications. For safety, items like cell phones, laptops, sharp objects, and alcohol-based products are usually not permitted. Always check with the facility beforehand for their specific list.
Conclusion
When you or a loved one faces a severe mental health crisis, the path forward can seem unclear. Inpatient behavioral health treatment exists for these moments. It is not a sign of failure but a necessary and life-saving medical intervention.
This level of care provides immediate safety, 24-hour medical supervision, intensive therapy, and a structured plan for long-term recovery. It offers hope by creating a secure space where healing can begin.
Recovery is not just possible; it’s happening every day. An inpatient stay is often the turning point that stops a downward spiral and starts the journey toward wellness.
At Addiction Helpline America, we understand the fear and confusion of a mental health crisis. We are here to provide free, confidential, and personalized guidance to help you steer your options and find the right care. You do not have to face this alone.
Whether you are seeking help for yourself or a loved one, we can connect you with the right treatment facility for your situation. Explore different types of treatment programs to learn more, or contact us directly for support.
Remember: seeking help is an act of courage. Lasting recovery is within reach.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.