
Why Knowing How to Act in an Overdose Emergency Can Save a Life
Immediate help for drug overdose can be the difference between life and death. When someone overdoses on opioids, their breathing slows or stops, and brain cells begin dying within minutes. Here’s what you need to do right now if you suspect an overdose:
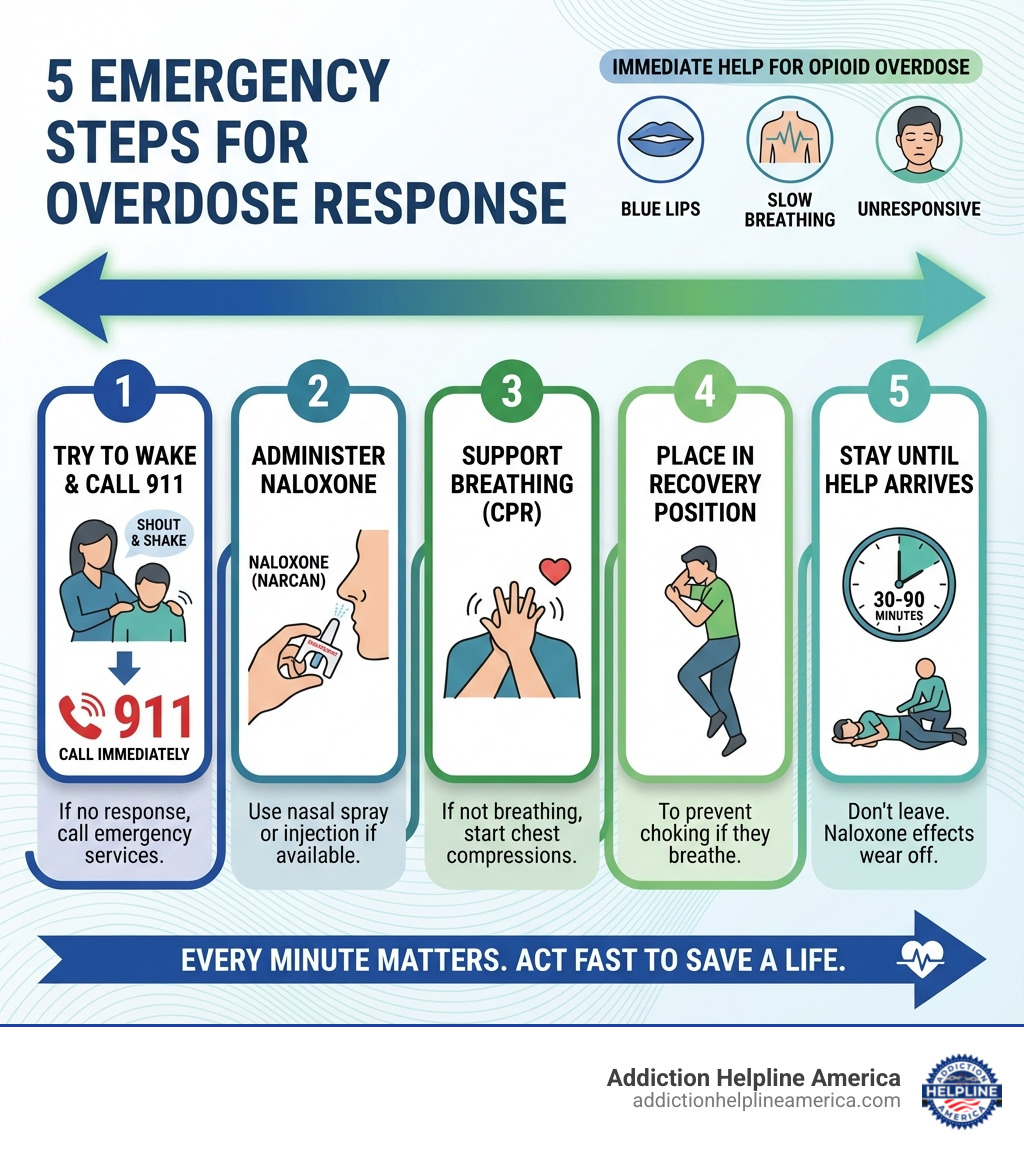
The 5 Critical Steps:
- Try to wake them – Shout their name and shake their shoulders. If no response, call 911 immediately.
- Give naloxone – Administer nasal spray (Narcan) or injection if available. It reverses opioid effects within 2-3 minutes.
- Start CPR – If they’re not breathing, begin chest compressions at 100-120 per minute.
- Recovery position – Turn them on their side to prevent choking if they start breathing.
- Stay with them – Don’t leave until emergency help arrives. Naloxone effects are temporary.
You won’t get in trouble for calling 911. Good Samaritan laws in most states protect you from drug possession charges when seeking help during an overdose.
Nearly 50,000 people died from opioid overdoses in 2019, and bystanders were present in more than one in three cases. That means you have the power to save a life. Most overdose deaths happen at home, and in nearly 40% of cases, someone else was there. Acting fast matters because every minute without oxygen causes more brain damage.
A drug overdose happens when someone takes a toxic amount of opioids like heroin, fentanyl, or prescription painkillers. The drugs overwhelm the brain’s ability to control breathing, leading to respiratory failure. But here’s the hopeful truth: overdose is reversible when you act quickly.
You don’t need medical training to help. Naloxone is safe, easy to use, and available without a prescription in all 50 states. Many community programs offer it for free. And if you don’t have naloxone, calling 911 and performing CPR can still save someone’s life.
At Addiction Helpline America, we’ve guided countless families through overdose emergencies and connected them with life-saving resources for immediate help for drug overdose and long-term recovery support. Our free, confidential helpline at 844-561-0606 is available 24/7 to provide urgent guidance and connect you with treatment options.
Recognizing the Signs of an Opioid Overdose
Recognizing the signs of an opioid overdose is the crucial first step in providing immediate help for drug overdose. Opioids, whether prescription painkillers, heroin, or fentanyl, can depress the central nervous system, leading to life-threatening respiratory failure. Acting quickly based on these signs can save a life.
What are the immediate signs and symptoms of an opioid overdose?
The signs and symptoms of an opioid overdose are distinct and require immediate attention. They often indicate that the brain is not receiving enough oxygen, which can lead to severe brain damage or death within minutes. Look for these critical indicators:
- Slow or stopped breathing: Breathing may be very shallow, erratic, or have stopped completely. The person might also be gasping for air. This is a primary danger, as opioids interrupt the brain signals that control breathing.
- Gurgling or deep snoring sounds: These sounds, sometimes called the “death rattle,” indicate that the airway is partially blocked, often by vomit or the tongue falling back.
- Limp body: The person’s muscles will be relaxed, and their limbs may be weak or entirely limp.
- Pale, cold, or clammy skin: Their skin may feel cool to the touch and appear pale or grayish.
- Blue or purple lips and fingernails: This is a clear sign of cyanosis, meaning a severe lack of oxygen in the blood. This discoloration can also appear around the eyes or on other extremities.
- Pinpoint pupils: The black center of the eyes may be extremely small, constricted, and unresponsive to light.
- Unconsciousness: The person cannot be woken up, even with loud shouting or painful stimuli. They are unresponsive to their name or physical stimulation.
If you observe any of these signs, assume it is an overdose and prepare to provide immediate help for drug overdose.
How to tell the difference between being high and an overdose
It can be challenging to differentiate between someone who is simply “high” on opioids and someone experiencing a life-threatening overdose. However, if you are unsure, always treat it as an overdose. It’s better to overreact than to risk a life.
Here’s a comparison to help you distinguish:
| Feature | Being “High” | Experiencing an Overdose |
|---|---|---|
| Responsiveness | Drowsy but responsive to verbal commands, light shaking, or sternum rub. May nod off but can be roused. | Unresponsive to shouting, shaking, or sternum rub. Cannot be woken up. |
| Breathing | Slow and shallow, but regular. | Extremely slow, shallow, or stopped breathing. May have long pauses between breaths, or make gurgling/snoring sounds. |
| Skin Color | Normal or slightly flushed. | Pale, grayish, or bluish, especially on the lips, fingernails, and around the eyes. Skin may be cold and clammy. |
| Pupils | Constricted, but may still react slightly to light. | Pinpoint pupils (very small) that do not react to light. |
| Body Tone | Relaxed, but some muscle tone remains. | Limp body, flaccid limbs. |
| Awareness | Aware of surroundings, though possibly disoriented. | Unconscious, unaware of surroundings. |
The key distinction is responsiveness and the severity of breathing depression. If someone cannot be roused and their breathing is severely compromised, they are likely overdosing and need immediate help for drug overdose.
The 5 Steps for Providing Immediate Help for Drug Overdose
When every second counts, knowing these five steps can empower you to provide immediate help for drug overdose and potentially save a life.

Step 1: Try to Wake Them and Call 911 Immediately
Your first priority is to assess the situation and get emergency services on the way.
- Shout their name and gently shake their shoulders: Try to elicit a response. If they don’t respond, try a more painful stimulus like a sternum rub (rubbing your knuckles firmly up and down their breastbone).
- If unresponsive, call 911 or your local emergency number immediately: Time is critical. Do not hesitate.
- Provide your exact location: Be clear about the address, cross streets, or any landmarks. If you are in a remote area, look for emergency markers if available.
- State you suspect an overdose: Clearly tell the operator that you believe the person is experiencing a drug overdose.
- Mention if the person is not breathing or is breathing erratically: This information helps emergency responders prepare.
Step 2: Administer Naloxone (Narcan) if Available
Naloxone is a true lifesaver that can rapidly reverse the effects of an opioid overdose. It is an opioid antagonist, meaning it binds to the same brain receptors as opioids, blocking their effects and allowing the person to breathe normally again.
- It can reverse opioid effects: Naloxone can restore normal breathing within 2 to 3 minutes.
- Administer nasal spray or injection if you have it: If you have a naloxone kit, use it immediately. Follow the instructions provided with your specific kit. For nasal spray, lay the person flat on their back, tilt their head back, insert the device into one nostril, and push the plunger firmly. For more detailed instructions, refer to our guide on How to use naloxone nasal spray.
- It is safe to use even if opioids are not present: Naloxone will not harm someone who isn’t overdosing on opioids, making it safe to administer if you are unsure of the cause but suspect an overdose.
Step 3: Support Their Breathing with CPR
If the person is not breathing or only gasping, providing oxygen is vital, especially if naloxone is not immediately available or while waiting for it to take effect.
- Check for breathing: Look, listen, and feel for breaths.
- If not breathing or only gasping, begin CPR: If you are trained in CPR, begin chest compressions immediately. Place the heel of one hand in the center of their chest, place your other hand on top, and push hard and fast, aiming for 100-120 compressions per minute, about 2 inches deep.
- Rescue breaths if trained and comfortable: If you are trained and comfortable giving rescue breaths, administer two breaths after every 30 compressions.
- Hands-only CPR is better than no CPR: If you haven’t been trained or are uncomfortable with mouth-to-mouth, performing continuous chest compressions (hands-only CPR) is still incredibly effective and can provide critical oxygen to the brain. To learn more about the critical role of CPR in an overdose emergency, see The role of CPR in overdose response.
Step 4: Place Them in the Recovery Position
Once the person starts breathing on their own, or if you need to leave them momentarily to call for help, placing them in the recovery position is essential to prevent choking.
- How to roll the person onto their side: Gently roll the person onto their side. Ensure their head is supported and tilted back to keep the airway open. Their top leg should be bent at the knee to stabilize them.
- Keeps airway clear: This position prevents the tongue from blocking the airway.
- Prevents choking on vomit: If the person vomits, the recovery position helps prevent aspiration into the lungs, which can be fatal.
- Monitor breathing: Continue to monitor their breathing closely while they are in this position.
Step 5: Stay With Them Until Help Arrives
Your presence and continued monitoring are crucial even after administering naloxone or starting CPR.
- Naloxone effects are temporary (30-90 minutes): Opioids can last longer in the body than naloxone. This means the person can re-overdose once the naloxone wears off.
- Overdose can return: It’s vital to stay and watch for any return of overdose symptoms. More naloxone might be needed.
- Monitor the person’s condition: Keep checking their breathing, responsiveness, and skin color.
- Provide reassurance: Talk to them calmly, even if they appear unresponsive. Let them know help is coming.
- Cooperate with emergency responders: When paramedics arrive, provide them with all the information you have about what happened, what was taken (if known), and what actions you took.
- The common effects of drug addiction can be complex, and immediate help is just one part of a larger journey toward recovery.
Understanding Naloxone and Legal Protections
Understanding naloxone and the legal protections available can significantly reduce hesitation in providing immediate help for drug overdose. We want to empower everyone to act without fear.
What is naloxone and how can you get it?
Naloxone (often known by the brand name Narcan®) is an opioid antagonist, a medication specifically designed to rapidly reverse an opioid overdose. It works by blocking the effects of opioids on the brain, quickly restoring normal breathing and consciousness.
- Opioid antagonist: Naloxone competes with opioids for the same receptors in the brain, essentially kicking the opioids off and reversing their effects.
- How it works: When administered, it rapidly binds to opioid receptors, counteracting respiratory depression, which is the most dangerous effect of an opioid overdose.
- Nasal spray vs. injection: Naloxone is commonly available as a nasal spray (pre-filled device, one spray per nostril) or as an injectable solution (given into a muscle or under the skin). Both forms are safe and easy to use, even without medical training.
- Available in many pharmacies and through community programs: Naloxone is available over-the-counter in all 50 states, meaning you don’t need a prescription. You can ask your pharmacist for it. Many local health departments and community-based programs also provide naloxone kits for free or at a reduced cost. For more information on where to obtain this life-saving medication, please visit our page on How to get naloxone kits.
- Co-prescription with opioids: If you or a loved one are prescribed high-dose opioids, talk to your doctor about getting naloxone co-prescribed. It’s an important safety measure, especially if you are at an increased risk for overdose.
- Find help for opioid addiction: If you or someone you know is struggling with opioid use, comprehensive help is available. We can connect you with resources for opioid addiction treatment.
What are Good Samaritan Laws for Overdose Response?
Fear of legal repercussions can sometimes prevent people from calling for help during an overdose. However, Good Samaritan laws are designed to remove this barrier and encourage individuals to seek immediate help for drug overdose.
- Legal protection for calling 911: Most states have Good Samaritan laws that provide some legal protection for people who call 911 or their local emergency number during an overdose.
- Protects the caller and the person overdosing: These laws typically protect both the person experiencing the overdose and the person who calls for help from charges related to drug possession or paraphernalia.
- Protection from simple possession charges: The primary goal is to ensure people are not afraid to seek emergency medical assistance due to fear of arrest for minor drug offenses.
- Does not cover trafficking or outstanding warrants: These laws generally do not protect against more serious offenses like drug trafficking, manufacturing, or outstanding warrants. The focus is on saving a life during an emergency.
- Learn more about Good Samaritan laws: We encourage you to familiarize yourself with the specific Good Samaritan laws in your state. You can find more comprehensive information on our page about Good Samaritan laws for overdose.
Overdose Prevention and Finding Long-Term Support
While providing immediate help for drug overdose is critical, preventing overdoses from happening in the first place and finding long-term support are equally important. We believe in a hopeful path to recovery, addressing both the immediate crisis and the underlying challenges. Our Mental Health Complete Guide offers further support.
How to Reduce the Risk of an Overdose
Understanding and mitigating risk factors can significantly reduce the likelihood of an opioid overdose.
- Risk factors:
- Mixing drugs: Combining opioids with other central nervous system depressants like alcohol or benzodiazepines (e.g., Xanax, Valium) significantly increases the risk of respiratory depression and overdose.
- Reduced tolerance: After a period of abstinence (e.g., leaving rehab or a detox facility), a person’s tolerance to opioids decreases. Using the same amount they used before can lead to a fatal overdose.
- Using alone: If an overdose occurs while using alone, there’s no one to provide immediate help for drug overdose or call for emergency services.
- Unknown potency: Illicitly manufactured opioids, especially those containing fentanyl or carfentanil, can be incredibly potent and deadly in tiny amounts. Their strength is often unknown.
- Prevention tips:
- Never use alone: Always use with a buddy or in a supervised setting. If you must use alone, consider calling a national overdose prevention line or using an app designed to alert others if you become unresponsive.
- Start with a small dose: Especially if you’re trying a new batch or if your tolerance has decreased. “Start low, go slow.”
- Test your drugs: If available in your area, use drug checking services to understand the composition and potency of substances.
- Carry naloxone: Always have naloxone on hand, and make sure those around you know where it is and how to use it.
- Return unused or expired prescriptions: Dispose of old opioid prescriptions safely at pharmacies or designated drop-off sites to prevent misuse.
For those on the path to recovery, understanding the detox process is vital. Learn more about How long does it take to detox from heroin?.
Where to Find Additional Resources and Support
Beyond immediate crisis response, a robust network of resources and support systems is essential for long-term recovery and overdose prevention.
- Addiction Helpline America (844-561-0606): Our free and confidential helpline connects individuals nationwide to addiction and mental health treatment centers. We provide personalized guidance to find the right recovery program from our vast network, including facilities in Alabama, Alaska, Arizona, Arkansas, California, Colorado, Connecticut, Delaware, Florida, Georgia, Hawaii, Idaho, Illinois, Indiana, Iowa, Kansas, Kentucky, Louisiana, Maine, Maryland, Massachusetts, Michigan, Minnesota, Mississippi, Missouri, Montana, Nebraska, Nevada, New Hampshire, New Jersey, New Mexico, New York, North Carolina, North Dakota, Ohio, Oklahoma, Oregon, Pennsylvania, Rhode Island, South Carolina, South Dakota, Tennessee, Texas, Utah, Vermont, Virginia, Washington, West Virginia, Wisconsin, and Wyoming.
- Local health departments: These agencies often provide information on local naloxone distribution programs, harm reduction services, and substance use treatment options.
- Community harm reduction programs: These programs offer vital services such as naloxone kits, safe injection supplies, and education on safer drug use practices.
- Types of Addiction Therapy: Understanding the different therapeutic approaches available can help individuals find the most effective treatment for their needs. Explore Types of Addiction Therapy.
- Support groups: Organizations like Narcotics Anonymous (NA) offer peer support and a path to recovery through shared experiences.
- SAMHSA National Helpline: The Substance Abuse and Mental Health Services Administration (SAMHSA) operates a national helpline at 1-800-662-HELP (4357) for individuals and families facing mental and/or substance use disorders.
Frequently Asked Questions about Immediate Help for Drug Overdose
What are the consequences if an overdose is not treated immediately?
The consequences of an untreated opioid overdose are severe and often irreversible. When breathing slows or stops, the body, especially the brain, is deprived of oxygen.
- Brain damage from lack of oxygen: Within minutes, brain cells begin to die, leading to permanent neurological damage.
- Coma: Prolonged lack of oxygen can result in a coma.
- Permanent disability: Survivors may experience long-term cognitive impairments, motor skill issues, or other disabilities.
- Death: If the overdose is not reversed quickly, it will lead to death. This underscores the critical importance of providing immediate help for drug overdose.
What should I do if naloxone is not available?
If naloxone is not available, do not despair, and do not delay calling 911. Your actions can still make a life-saving difference.
- Do not delay calling 911: This is the most crucial step. Emergency medical professionals have advanced tools and medications, including naloxone.
- Focus on rescue breathing and CPR to supply oxygen to the brain until help arrives: If the person is not breathing, immediately begin chest compressions (hands-only CPR) or full CPR if you are trained. Providing oxygen to the brain and vital organs can buy critical time until paramedics arrive.
Can you get in trouble for helping someone who overdosed?
In most states, the answer is generally no, thanks to Good Samaritan laws.
- Most states have Good Samaritan laws to protect you from drug possession charges when you call for help: These laws are specifically designed to remove the fear of legal repercussions for those who seek emergency medical assistance during an overdose. They typically protect both the caller and the person experiencing the overdose from charges for simple drug possession.
- The goal is to save a life, and these laws encourage that: Legislators understand that the priority in an overdose situation is to save a life, not to prosecute minor drug offenses. By providing legal immunity, these laws empower individuals to act quickly and call for help without hesitation.
Conclusion
You now have the knowledge and steps to provide immediate help for drug overdose. You have the power to save a life. Overdose is reversible, and your quick actions can prevent tragedy and open the door to a new beginning.
Recovery is possible, and a life free from the grip of addiction is within reach. If you or a loved one is struggling with substance use, please know that help is available. Addiction Helpline America offers a free, confidential helpline to connect you with treatment options custom to your needs.
Call 844-561-0606 now or visit our Substance Abuse Helpline Complete Guide to start the path to recovery.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.












