Why Understanding Meloxicam Discontinuation Matters
Safely learning how to stop meloxicam requires medical guidance, but many don’t realize the risks of discontinuing this common pain medication without a plan.
Quick Answer: Safe Meloxicam Discontinuation Steps
- Consult your doctor first – Never stop without medical advice
- Follow a tapering plan – Gradual reduction may be needed for long-term users
- Monitor for returning symptoms – Pain and inflammation will likely return
- Prepare alternatives – Have other pain management strategies ready
- Watch for complications – Report any unusual symptoms immediately
Unlike opioids, meloxicam doesn’t cause traditional withdrawal. However, stopping this NSAID (non-steroidal anti-inflammatory drug) can lead to the return of underlying pain and inflammation, known as “rebound symptoms.”
Meloxicam has an elimination half-life of 15 to 24 hours, taking up to 80 hours to completely exit your system. During this time, the pain and swelling it controlled will gradually return.
Why stopping suddenly can be problematic:
- Return of chronic pain conditions like arthritis
- Increased inflammation and stiffness
- Potential cardiovascular risks in some patients
- Gastrointestinal rebound effects
At Addiction Helpline America, we’ve helped many with prescription medication concerns, including guidance on how to stop meloxicam safely when misuse is a factor. Our team knows even non-addictive drugs can create dependency issues that need professional support.
Understanding Meloxicam and Its Purpose
To understand how to stop meloxicam, it’s helpful to know what this medication does and why your doctor prescribed it.
Meloxicam is a prescription NSAID (non-steroidal anti-inflammatory drug). You might recognize it by its brand names Mobic or Vivlodex. It acts as your body’s inflammation fighter, working to control pain and swelling.
Meloxicam works by targeting cyclooxygenase-2 (COX-2) enzymes. These enzymes produce prostaglandins, compounds that cause pain and inflammation. By blocking COX-2, meloxicam shuts down this process.
This makes meloxicam effective for chronic conditions involving ongoing inflammation. Doctors most commonly prescribe it for osteoarthritis, rheumatoid arthritis, and sometimes juvenile rheumatoid arthritis.
According to the CDC, over 58 million US adults have arthritis. That’s nearly one in four adults dealing with joint pain and inflammation that can significantly impact daily life. What is an inflammation? Understanding this process helps explain why stopping meloxicam requires careful planning.
People want to stop meloxicam for various reasons. Sometimes the underlying condition improves. Other times, people experience side effects like stomach upset, or have concerns about long-term kidney function. Your doctor might also recommend stopping due to blood pressure changes or other health considerations.
Whatever your reason for considering stopping, the decision affects your body’s pain management. Learning how to stop meloxicam safely is crucial because your body needs time to adjust to its absence.
The Risks of Stopping Meloxicam Without Medical Guidance
When considering how to stop meloxicam, understand that stopping suddenly without medical guidance can create challenges, even though it’s not addictive like opioids.
Stopping meloxicam is like putting away an umbrella in a rainstorm; the pain and inflammation it protected you from will likely return, sometimes with a vengeance.
The main concern is rebound effects, not traditional withdrawal. When the drug’s anti-inflammatory protection is gone, your underlying condition can return, sometimes stronger.
Rebound pain is often the first symptom. The arthritis pain and stiffness can return more than before. This is a real physiological response.
Rebound inflammation follows closely. You might wake up with joints that feel more swollen, stiffer, or tender. The redness and warmth in affected areas can also increase as your body’s inflammatory response restarts.
But the risks go beyond your original symptoms. If you’ve been taking meloxicam long-term or at high doses, stopping suddenly can affect other body parts.
Your gastrointestinal system may react unpredictably. Abruptly stopping NSAIDs like meloxicam can disrupt your digestive system, potentially worsening ulcers or increasing bleeding risk.
Your kidneys also need time to readjust. Long-term use can impact kidney function, so sudden discontinuation requires careful monitoring, especially if you have existing kidney issues.
Blood pressure changes are another consideration. Since NSAIDs can affect blood pressure, stopping meloxicam might cause fluctuations that need medical attention, especially if you have hypertension.
Potential cardiovascular risks are also a concern. Research shows an increased risk of cardiovascular events with NSAID use, so changes to your regimen must be managed carefully to minimize heart-related complications.
These effects differ from the severe withdrawal symptoms of addictive substances like opioids or alcohol. Meloxicam doesn’t create that kind of physical dependence.
Meloxicam “Withdrawal” Symptoms vs. Rebound Effects
Meloxicam doesn’t cause true withdrawal. It isn’t psychoactive, meaning it does not readily cross the blood–brain barrier or alter brain chemistry to create dependence.
What’s often called “withdrawal” is actually the return of underlying symptoms the medication was managing.
The physical discomfort comes from your original condition returning: arthritis pain, joint stiffness, and swelling. Some people also report fatigue, headaches, or an upset stomach as their body readjusts.
Psychological adjustments are also possible, but they’re typically responses to returning pain. It’s natural to feel irritable, worried, or mildly depressed when chronic pain returns, as it affects your mood.
Meloxicam has a half-life of 15 to 24 hours, so most of the drug is gone within a few days, though traces can be detected for up to 3-5 days.
The timeline for rebound effects varies. For short-term, low-dose users, symptoms may return within days and peak for about a week. For long-term, high-dose users, effects could last several weeks as the body readjusts.
Understanding these effects helps you prepare and work with your provider to manage the transition safely.
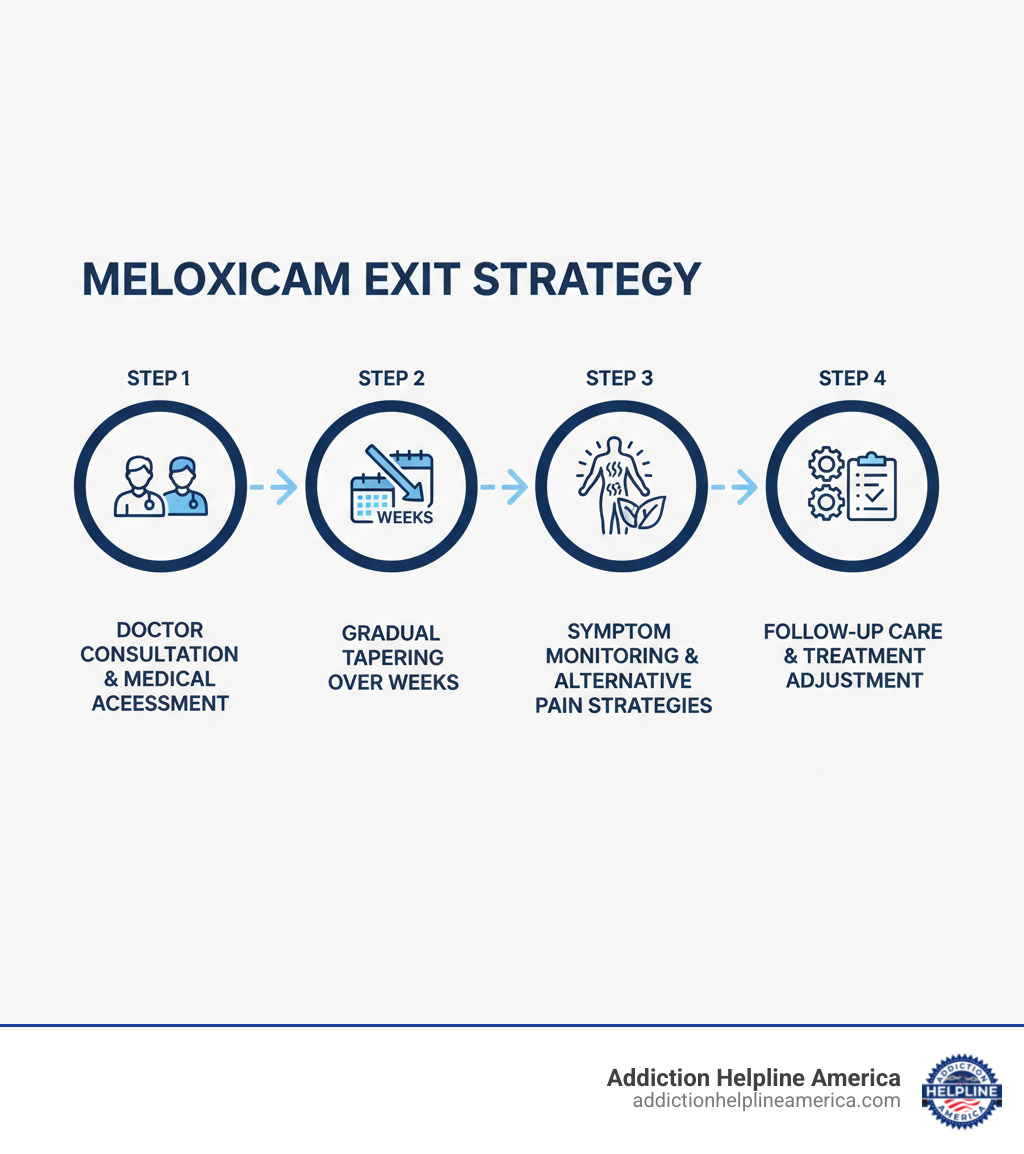
How to Stop Meloxicam Safely: A Step-by-Step Guide
When it comes to how to stop meloxicam, the golden rule is to never do it alone. Your healthcare provider must be your partner, providing medical supervision and personalized guidance for a smooth transition.
Your doctor is your navigator. They know your health history and can help create a custom discontinuation plan for your needs. The goal is to minimize discomfort and manage returning symptoms. Let’s walk through each essential step.
Step 1: Consult Your Healthcare Provider
This step is essential for safe discontinuation. Before reducing your dose, have a thorough conversation with your doctor.
Your provider knows your medical history, including how long you’ve been taking meloxicam, your dosage, and your body’s response. They can foresee complications, especially if you have other health conditions or take other medications.
Be honest about your reasons for wanting to stop, whether it’s side effects, long-term risks, or condition improvement. This helps your doctor assess if stopping is appropriate.
Your doctor will likely evaluate your current health status first. This may include kidney function tests, blood pressure monitoring, or an assessment of your underlying condition to ensure it’s safe to stop.
Most importantly, this appointment is where you’ll work together to create your personalized plan. Your doctor might recommend stopping immediately, suggest a gradual reduction, or advise waiting. They’ll also discuss alternative pain management strategies.
Step 2: Following a Tapering Schedule (If Necessary)
Individual circumstances matter. While many can stop meloxicam without tapering, others benefit from this gradual approach.
Tapering means slowly reducing your medication dose over time, giving your body a chance to adjust.
Your doctor may recommend tapering for long-term or high-dose use. Long-term users often benefit most as their bodies are accustomed to the drug’s effects. It may also be advised for people with certain health conditions.
The main benefit of tapering is preventing intense rebound pain and inflammation by giving your body time to readjust. The CDC emphasizes that some medications should be tapered under medical supervision for safety and comfort.
Stopping cold turkey isn’t usually dangerous with meloxicam. It doesn’t typically cause serious medical complications when stopped abruptly. However, you might experience a more intense return of your original pain and inflammation, which can be challenging for those with chronic arthritis.
The decision between tapering and stopping immediately should always be made with your doctor’s guidance.
Step 3: How to Stop Meloxicam and Manage Returning Symptoms
With a plan, the work begins. This phase involves actively monitoring how your body responds and having strategies to manage returning symptoms.
Pay close attention to your body. Track pain, stiffness, and swelling. A journal can be helpful for follow-up appointments with your doctor.
Contact your provider if you notice severe pain, new digestive issues, or other concerning symptoms.
As your body adjusts, non-pharmacological approaches can provide significant relief. Heat therapy (warm baths, heating pads) can ease stiff joints. Cold therapy with ice packs can reduce swelling and numb acute pain.
Gentle exercise is vital. Activities like stretching, walking, or swimming help maintain joint flexibility. Listen to your body and avoid pushing through severe pain.
Quality rest is also important. Your body needs sleep to heal and adapt. Good rest helps you cope with discomfort.
Successfully learning how to stop meloxicam means finding new ways to support your body. The right strategies and medical support make the transition manageable.
Life After Meloxicam: Alternative Pain Management Strategies
Successfully stopping meloxicam opens the door to new pain management approaches. The journey continues as you explore new strategies that may work better for you.
This transition is an opportunity to build a comprehensive pain management toolkit, using multiple approaches to stay comfortable and active.
Non-Pharmacological and Lifestyle Alternatives
Many people find significant relief through non-medication approaches. These natural strategies can improve your overall quality of life.
- Physical therapy can be a game-changer for arthritis pain. A therapist can teach you exercises to strengthen muscles, improve flexibility, and reduce strain on joints.
- Acupuncture is a practice where thin needles are placed at specific points to reduce pain signals. Many find it relaxing and effective.
- Massage therapy is another hands-on approach. It can relieve tight muscles, improve blood flow, and help release natural pain-relievers.
- Yoga and meditation combine movement with mental relaxation. Gentle yoga is available for those with joint pain, and the mindfulness aspect is also valuable.
- An anti-inflammatory diet—rich in fruits, vegetables, fatty fish, and whole grains, while low in processed foods—can help reduce inflammation.
- Weight management is crucial for joint pain. Losing even a small amount of weight can significantly reduce pressure on joints like knees and hips.
- Regular exercise, like swimming or walking, helps keep joints flexible and strengthens supporting muscles.
Medication Alternatives to Discuss with Your Doctor
Sometimes, medication is still needed. Your doctor can help you explore alternatives to meloxicam that better suit your needs.
- Acetaminophen is an option for pain without significant inflammation. It’s gentler on the stomach and has fewer cardiovascular risks than NSAIDs.
- If inflammation persists, your doctor might suggest other NSAIDs like ibuprofen or naproxen. People respond differently to various NSAIDs. You can learn about Other NSAIDs.
- Topical pain relievers (creams, gels, patches) offer targeted relief with fewer systemic side effects.
- For stubborn inflammation, corticosteroid injections can provide targeted, long-lasting relief.
The key is working with your healthcare team to create a personalized plan. Your doctor can help you find the right combination of treatments to keep you comfortable and active.
Meloxicam, Dependence, and When to Seek Professional Help
When discussing how to stop meloxicam, questions about addiction and dependence are natural. At Addiction Helpline America, we address these concerns daily. While meloxicam differs from opioids, understanding the full picture is key to your safety.
Is Meloxicam Addictive?
Meloxicam is generally not considered addictive. It doesn’t hijack the brain’s reward system like other substances.
The science backs this up. Meloxicam is not psychoactive and does not readily cross the blood–brain barrier, which is what addictive substances do.
However, your body can develop dependence. After long-term use for chronic pain, your body adapts. When you stop, the underlying pain returns, sometimes intensely.
Physical dependence on meloxicam manifests as rebound pain and inflammation. This is your body readjusting, not craving the drug.
Psychological dependence is also real. The fear of facing chronic pain without medication can be overwhelming, leading to anxiety or compulsive use—taking it even when it’s no longer needed or causes side effects.
How to Stop Meloxicam When Misuse is a Concern
Meloxicam abuse is uncommon but possible. Signs of misuse include taking more than prescribed, using it too frequently, or combining it with alcohol or opioids.
If you recognize these patterns, you’re not alone. Chronic pain can lead to desperate measures. The key is recognizing when use becomes problematic.
When misuse is a factor, learning how to stop meloxicam is more complex. You may be dealing with multiple substances, mental health concerns, or a substance use disorder requiring professional help.
Comprehensive treatment is crucial here. At Addiction Helpline America, we know prescription misuse can stem from legitimate medical needs. We connect you with centers that address both the physical and underlying issues.
When to seek professional treatment may not be obvious. If you struggle with dosing, combine meloxicam with other substances, or feel panicked about stopping, it’s time to reach out. Misuse can signal broader challenges with pain management.
Seeking help is a sign of strength. If you or a loved one struggles with prescription medications, professional support can help you find a safe path forward.
Conclusion
Learning how to stop meloxicam safely isn’t a solo journey. You need a plan, like a map for a road trip.
The good news is meloxicam doesn’t cause intense withdrawal like addictive drugs. However, stopping isn’t always easy. Your body is used to the help, and symptoms will likely return when it’s removed.
The most important step is talking to your doctor. They know your history and can create a personalized plan, which may involve tapering your dose or stopping immediately.
Effective pain management continues after stopping meloxicam. This is a chance to find new ways to feel better, such as gentle exercise, heat therapy, dietary changes, or physical therapy.
Even though meloxicam isn’t typically addictive, struggles with prescription medication are real. What starts as pain management can become a difficult pattern to break.
At Addiction Helpline America, we’ve helped many people who felt alone in their struggles. If you or a loved one are struggling with prescription drug misuse, confidential help is available. We understand each situation is unique and can help you find support without judgment.
You don’t have to do this alone. We offer free, confidential, personalized guidance to connect you with suitable treatment programs. Taking the first step is smart. Find personalized addiction and mental health treatment today and move forward with confidence.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.