Understanding Your Personal Relapse Risk Factors
Thinking about how to prevent relapse isn’t a one-size-fits-all deal. Your path to recovery is unique, and so are the challenges that might pop up along the way. To build a solid plan for staying sober, you first have to get real about what your specific risks look like. This isn’t about scaring yourself; it’s about empowering yourself with knowledge.
A huge piece of the puzzle is the substance you’re recovering from. The daily fight in alcohol recovery looks very different from the challenges of opioid recovery. Each substance affects the brain in its own way, leading to different types of cravings and withdrawal symptoms. This means relapse rates can vary quite a bit. For example, some studies show that up to 80% of people treated for alcohol use disorder may relapse within the first year. For opioids, which are notoriously powerful, that number can be as high as 91%.
Knowing these stats isn’t meant to discourage you, but to help you respect the specific battle you’re in. You can discover more insights about relapse risks on HazeldenBettyFord.org to get a clearer picture.
To put this into perspective, let’s look at how the risks can differ. The following table breaks down relapse rates and common risk factors for several substances.
Relapse Risk Factors by Substance Type
Comparison of relapse rates and specific risk factors for different substances
| Substance | First Year Relapse Rate | Primary Risk Factors | Critical Prevention Window |
|---|---|---|---|
| Alcohol | 40-80% | Social situations (parties, bars), stress, celebratory events, boredom. | The first 90 days are often the most challenging due to social normalization and accessibility. |
| Opioids | Up to 91% | Pain (physical or emotional), encountering old dealers or users, prescription refills for unrelated issues. | The first 6-12 months are extremely high-risk due to intense post-acute withdrawal. |
| Stimulants | ~61% | Cues related to “high-achieving” environments, fatigue, depression, places associated with past use. | High-stress periods and the first 3-6 months after stopping use are critical. |
| Cannabis | ~50% | Social circles where use is common, stress, boredom, belief that it’s “not a big deal.” | The first 30-90 days, as psychological dependence and routine are broken. |
This data shows that while the threat of relapse is real for everyone, the why and when can be very different. Understanding your specific substance’s profile is the first step in creating a targeted prevention strategy.
Identifying Your High-Risk Situations
Beyond the substance, your personal life creates a unique set of “triggers”—the people, places, feelings, or scenarios that can ignite a craving. Figuring these out isn’t about hiding from the world, but about learning how to face it with new skills.
Some common triggers fall into these buckets:
- Environmental Triggers: This could be anything from driving past your old go-to liquor store to hearing a specific song you used to listen to while high. For one person, a work happy hour is a clear danger zone. For another, it might be the loneliness of an empty house on a weekend.
- Emotional Triggers: Stress is a big one for almost everyone. A bad day at work, a fight with your spouse, or money troubles can make the thought of escaping with a substance seem very appealing. But don’t forget other powerful emotions like boredom, anger, loneliness, or even extreme happiness, which can make you feel like you “deserve” to celebrate with your old habit.
- Social Pressure: Sometimes it’s obvious, like an old friend offering you a drug. Other times it’s more subtle, like feeling like the odd one out at a wedding where everyone is drinking. This is where learning to set firm boundaries becomes a non-negotiable recovery skill.
Underlying Factors: Genetics and Mental Health
It’s also important to look at the deeper issues that can make you vulnerable to addiction. Your family history might play a part. Genetics can make some people more biologically prone to developing a substance use disorder. If addiction is common in your family, you might need to be extra careful on your own journey.
Even more significant is the link between addiction and mental health. Conditions like depression, anxiety, or PTSD are major risk factors. Many people start using substances to self-medicate the symptoms of an undiagnosed mental health challenge. True, lasting relapse prevention has to address both the addiction and any co-occurring disorders at the same time. Trying to treat one without the other is like bailing water out of a sinking boat without plugging the hole.
Mastering The Three-Pillar Prevention System
Thinking about how to prevent relapse can feel like a huge weight, but it gets a lot lighter when you break it down. Imagine building a structure with three strong pillars holding you up. You’re not just relying on one thing; you’re creating a support system that’s sturdy enough to handle whatever life throws at you. Clinical guidelines actually show that combining therapy, medication, and ongoing support creates a personalized safety net that dramatically lowers the chances of relapse. You can read the full research about relapse prevention strategies to see the data for yourself.
This isn’t about checking boxes on a generic plan. It’s about knowing what tools are out there and piecing together a strategy that feels right for you.
Pillar 1: Therapy And Skills Development
This is where you do the real inner work. It’s not just about talking through your problems; it’s about learning new ways to navigate life without turning to substances. In therapy, you’ll dig into your personal triggers—the specific people, places, or even feelings that spark cravings. From there, you’ll develop real-world strategies to face them without giving in. This is how you build a toolbox of healthy coping mechanisms that you can actually use when you feel stressed, lonely, or frustrated.
For example, instead of shutting down when you feel overwhelmed, a therapist can help you practice calling a friend or using a grounding exercise to bring you back to the present moment. There are many different paths here, from Cognitive Behavioral Therapy (CBT) to group counseling. If you’re curious about what might work for you, you can learn more about different types of addiction therapy in our guide.
Pillar 2: Medication-Assisted Treatment (MAT)
For many people, especially those recovering from opioid or alcohol addiction, medication can be a critical piece of the puzzle. Medication-Assisted Treatment (MAT) involves using specific, FDA-approved medications to help keep cravings and withdrawal symptoms at bay. Think of it like a splint for a broken leg—it doesn’t instantly heal the bone, but it gives it the stability and support it needs to heal correctly.
MAT can quiet the intense physical cravings, which gives you the headspace to truly engage with therapy and build new skills. It’s a common misconception that this is just trading one drug for another. In reality, it’s a medical treatment designed to support your recovery and is a key part of how to prevent relapse for countless individuals.
Pillar 3: Ongoing Monitoring And Support
Recovery isn’t a finish line you cross; it’s a path you walk every day. This third pillar is all about staying connected and accountable to keep you moving forward. This might look like:
- Having regular calls with a sponsor or mentor you trust.
- Attending support groups like AA or NA.
- Keeping scheduled appointments with your doctor or therapist.
This constant loop of support helps you spot warning signs early, celebrate your wins (big and small), and tweak your prevention plan before a minor slip-up turns into a major problem. When these three pillars work together, they create a strong and flexible defense against relapse.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Navigating The Critical First Six Months
Let’s be real: the first six months of recovery can feel like an eternity. This is when you step out of a structured environment and have to apply everything you’ve learned to the messy, unpredictable real world. It often feels like you’re learning to walk all over again, and the statistics highlight just how challenging this period is.
For instance, research shows that for people recovering from alcohol use disorder, about two-thirds may experience a relapse within the first six months after treatment. This isn’t meant to scare you; it’s to emphasize why this window is so critical. Understanding this high-risk period is a core part of figuring out how to prevent relapse. You can find more details about the challenges of early recovery and see why a solid, proactive plan makes all the difference.
This initial phase is tough because your brain is physically and chemically healing, and you’re essentially rewiring years of ingrained habits. You’re vulnerable, yes, but this is also your greatest opportunity to build a foundation that will support you for years to come.
Structuring Your Days For Stability
When your inner world feels chaotic, a predictable routine can be a lifesaver. Having a consistent daily structure reduces decision-making stress and creates a much-needed sense of normalcy and safety. It doesn’t need to be a rigid, minute-by-minute schedule, but simple anchors—like waking up at the same time, having regular meals, or scheduling a daily walk—can ground you.
This is especially helpful for tackling a powerful trigger: boredom. An afternoon with nothing to do can quickly become a dangerous mental space. Fill that time with intention. Choose activities that support your recovery, whether it’s listening to a recovery podcast, calling a friend, or even just tackling that closet you’ve been meaning to organize.
Building these new, healthy responses takes time and practice. This infographic breaks down the cycle of developing strong coping skills.
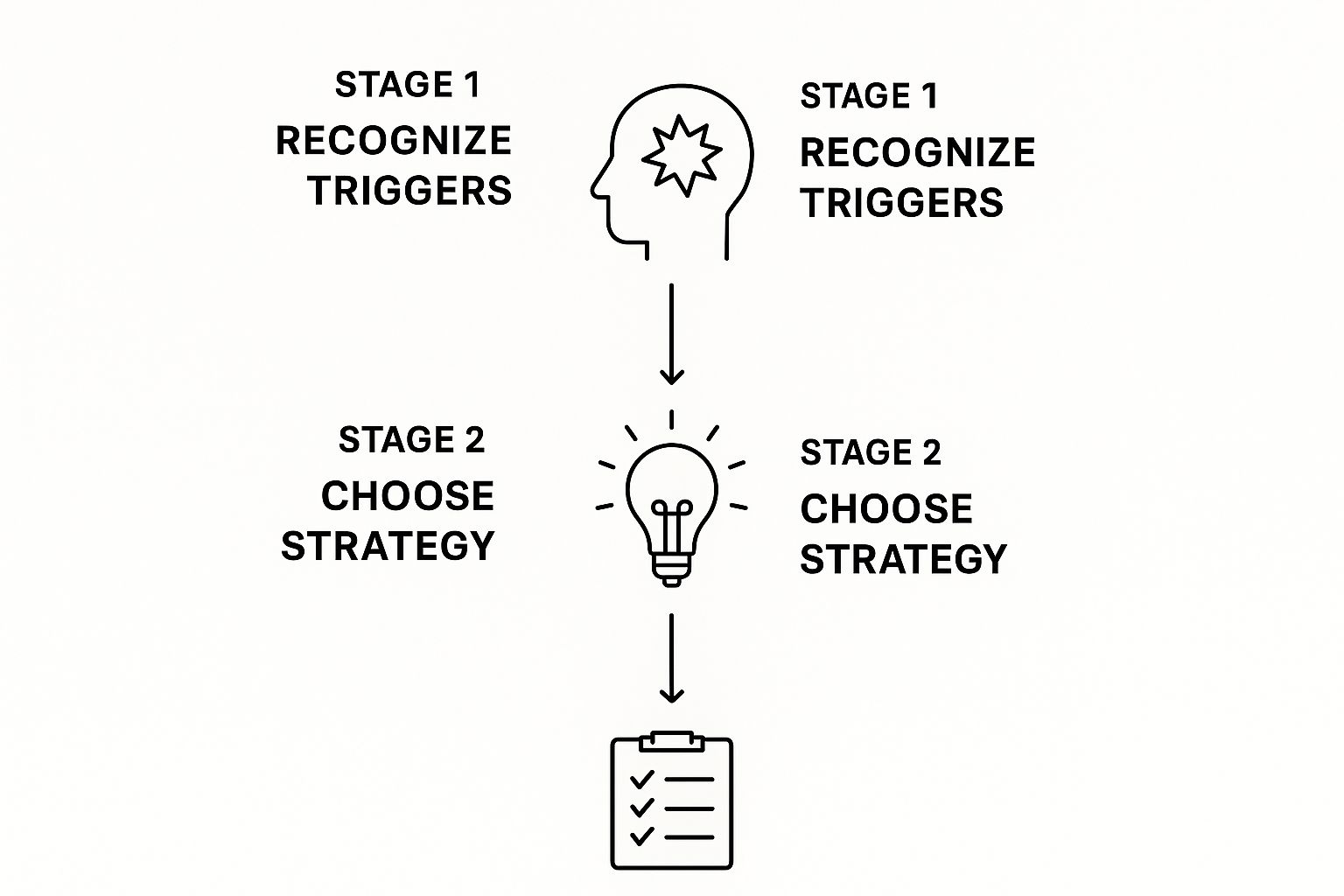
As the image illustrates, building resilience is a continuous process: you learn to recognize your triggers, consciously choose a healthier way to react, and then take a moment to reflect on what worked for next time.
To help you map out this journey, this table outlines some common milestones you can expect during your first six months. It offers a look at the challenges, what to focus on, and how to recognize your progress.
| Month | Common Challenges | Prevention Focus | Success Indicators |
|---|---|---|---|
| Month 1 | Intense cravings, post-acute withdrawal symptoms (PAWS), emotional volatility. | Establishing a solid routine, attending meetings daily, identifying triggers. | You’ve gone 30 days sober, built a small support contact list, and created a daily schedule. |
| Month 2 | The “pink cloud” fading, reality setting in, overconfidence. | Developing a crisis plan, practicing honesty with sponsors/therapists, setting small goals. | You can identify a craving and use a coping skill without prompting. |
| Month 3 | Boredom, frustration with slow progress, relationship issues surfacing. | Exploring new hobbies, practicing mindfulness, beginning to mend relationships. | You’re finding joy in new, sober activities and having more stable moods. |
| Month 4 | Feeling “cured” and tempted to test limits, complacency. | Deepening your work in therapy or a 12-step program, celebrating milestones. | You actively seek out support when you feel complacent or are facing a trigger. |
| Month 5 | Dealing with old friends or situations, managing stress without old crutches. | Setting firm boundaries, practicing stress-reduction techniques like meditation. | You can say “no” to an unsafe situation and manage a stressful day without relapsing. |
| Month 6 | Planning for the long term, facing bigger life decisions sober. | Creating long-term goals (career, education), serving others in recovery. | You feel confident in your ability to handle life’s ups and downs and are making future plans. |
This table isn’t a rigid checklist but a guide to help you feel prepared. Seeing your progress month by month can be a powerful motivator to keep moving forward.
Your Personal Crisis Plan
There will be moments when a craving hits you with the force of a tidal wave. In that moment of panic, you don’t want to be scrambling to figure out what to do. That’s why you need an emergency response plan written down and ready to go. This isn’t just a mental note; it’s a concrete list of actions you can take without having to think.
Here’s what your immediate response plan could look like:
- Make the call: Have at least two trusted people on speed dial who understand your situation and have agreed to be your emergency contacts.
- Move your body: If a trigger hits at home, get up and leave. Go for a brisk walk around the block. If you’re in a risky place like a grocery store aisle, turn around and walk out. A change of scenery can break the mental loop.
- Shock your senses: Distract your brain with a strong physical sensation. Splash ice-cold water on your face, bite into a slice of lemon, or hold an ice cube in your hand. The intense feeling can jolt you out of a craving.
Having this plan ready means you don’t have to rely on willpower when you’re feeling overwhelmed. You just have to follow your own instructions. This proactive strategy is how you turn one of the most fragile periods of recovery into the beginning of lasting change.
Building Your Personal Support Network That Actually Works

Recovery isn’t something you can muscle through on your own. While all the hard work ultimately comes from within, the people you surround yourself with can be either a lifeline or a liability. Creating the right kind of support network is a key strategy in how to prevent relapse, and it starts with being honest—first with yourself, and then with others. This isn’t just about having people around; it’s about making sure the right people are in your corner, actively rooting for your sobriety.
Identifying True Support vs. Well-Meaning Enablers
A truly supportive friend gets it. They respect your boundaries and won’t make things weird when you order a seltzer at a bar or suggest “just one” won’t hurt. An enabler, often with the best intentions, might feel sorry for you and suggest you bend the rules, not understanding they’re nudging you toward a cliff. The crucial difference is that a supporter protects your recovery, while an enabler, knowingly or not, protects your old habits.
Your inner circle might need some editing, and that can be a tough pill to swallow. It could mean creating distance with old friends who aren’t on board with your new life. The idea isn’t to burn every bridge but to be intentional about who you give a front-row seat to your recovery journey. For those who want more structured advice, our team has created a guide where you can learn more about how to build a support network that really fits your needs.
Sometimes, you need immediate, professional backup. National resources are out there 24/7, and they are incredibly valuable. Here’s a look at the SAMHSA National Helpline page, a great example of accessible support.

This shows that confidential, free help is always just a phone call away. They can provide information and connect you with treatment options whenever you need them.
Communicating Your Needs and Rebuilding Trust
Clear communication is your greatest asset. Your friends and family aren’t mind readers; you have to tell them what support looks like for you. This could mean:
- Setting clear boundaries: “I really want to see you, but I can’t be at family gatherings where there’s a lot of drinking right now. Could we grab coffee one-on-one instead?”
- Asking for specific help: “If I look overwhelmed, could you ask me if I want to take a walk? That would be more helpful than just telling me to ‘relax’.”
If addiction damaged your relationships, rebuilding that trust takes time and consistent effort. It’s about showing, not just telling, everyone that you are committed to this new path. Every promise you keep and every difficult moment you navigate sober is another brick in the foundation of that rebuilt trust.
Creating Daily Habits That Protect Your Recovery

A lasting recovery isn’t built on a few big, heroic decisions. It’s forged in the small, consistent choices you make every single day. These daily habits become the structure that supports your sobriety, a reliable framework that holds firm even when your motivation is low or life gets chaotic. When you focus on these small actions, the question of how to prevent relapse changes. It becomes less about desperately surviving a crisis and more about building a life where crises have less power over you.
The idea here isn’t to follow a strict, boot-camp-style regimen. It’s about discovering simple, repeatable routines that ground your day and give you a sense of stability and purpose.
Designing Your Morning and Evening Rituals
The way you begin and end your day can set the tone for everything that happens in between. A chaotic, reactive morning can leave you feeling off-kilter for hours, while a restless night can completely sap your resilience. Instead of letting the day just happen to you, you can take control with a few intentional rituals.
A solid morning routine could look something like this:
- Five minutes of quiet: Before you grab your phone, just take five minutes. You could meditate, do some deep breathing exercises, or even just sit with a cup of coffee and look out the window. This simple act creates a calm starting point for your day.
- A quick journal entry: Jot down one thing you’re grateful for and one thing you want to accomplish today. This shifts your mindset toward gratitude and gives you a clear intention.
- A bit of movement: A short walk around the block, a few simple stretches, or some push-ups can get your blood flowing and give you an immediate mood boost.
An evening ritual is just as important for winding down and processing the day, which helps with getting restorative sleep. This might be as simple as putting your phone away an hour before bed, reading a chapter of a book, or listening to some calming music. These aren’t just items on a to-do list; they are genuine acts of self-care that directly protect your recovery.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Turning Boredom and Stress into Strengths
Two of the most common relapse triggers are boredom and stress. In the past, feeling bored or stressed was likely a cue to use a substance. Now, you can see these feelings as an invitation to engage with your life in a new way. When you feel that old, familiar ache of boredom, have a list of activities ready to go. This could be anything from watching a tutorial to learn a new skill on YouTube, calling a supportive friend, or tackling that small organization project you’ve been putting off.
When stress shows up, your brain’s old wiring will probably start screaming for that quick, familiar escape. Your new job is to have a healthier tool ready and waiting. Instead of reaching for a substance, reach for your running shoes and go for a jog. Reach for your journal and get all those stressful thoughts out on paper. Or, reach for your phone and call your sponsor or a trusted friend.
Every time you consciously choose a healthy coping mechanism over an old, destructive one, you are physically rewiring the neural pathways in your brain. You weaken the old habit and strengthen the new one. This deliberate choice, made again and again, is how you fundamentally change your response to life’s inevitable challenges.
Handling Setbacks Without Losing All Your Progress
Let’s be real: at some point on your recovery journey, you’re going to hit a bump in the road. Thinking it’ll be a perfectly smooth ride is setting yourself up for a bigger fall. The most important thing to grasp is that not every mistake is a total disaster. There’s a world of difference between a minor slip—a one-time mistake you instantly regret—and a full-blown relapse, where you fall back into old, destructive patterns.
Knowing the difference is critical for figuring out how to prevent relapse when you’ve had a minor setback. Think of a slip as a warning light on your dashboard, not a sign that the engine has blown. It’s telling you to pull over and check what’s going on, not to abandon the car on the side of the road.
The moment you realize you’ve slipped, the feeling of shame can be crushing. This is a crucial turning point. If you let that shame win, you risk falling into something called the Abstinence Violation Effect. This is the dangerous mindset where you tell yourself, “Well, I’ve already blown my sobriety, so I might as well just keep going.” This is a trap. Your first move needs to be immediate damage control.
Taking Immediate Action
The goal here is simple: stop the slip from snowballing into a full-blown relapse. This isn’t a time for deep reflection; it’s a time for a pre-planned, rapid response. You need to know what to do before it happens.
- Reach out right away. Call your sponsor, therapist, or a trusted friend from your support network. Voicing what happened immediately breaks the power of secrecy and shame.
- Get to a safe environment. If you’re in a high-risk situation, leave. Go home, find a meeting, or head to a friend’s house—anywhere you know you will be safe from further temptation.
- Analyze what went wrong (with help). Once you’re in a clearer headspace, talk through the sequence of events with someone you trust. What was the trigger? Were there warning signs you might have overlooked?
Rebuilding and Moving Forward
A setback can feel like a massive failure, but it’s actually a priceless learning experience. It has just highlighted a weak spot in your recovery armor that you can now reinforce. After you’ve managed the immediate crisis, it’s time to focus on rebuilding your motivation. Remind yourself of all the progress you’ve made. One mistake doesn’t wipe out weeks or months of hard work.
From here, you adjust your game plan. Maybe this means you need more frequent check-ins with your therapist for a bit. Perhaps you need to set a firmer boundary with a particular person, or create a more solid plan for dealing with a trigger like stress or boredom. The key is to view this not as a final judgment on your recovery, but as a necessary course correction.
Our team has put together a resource that can help with this; you might want to look into learning more about aftercare and relapse prevention strategies to strengthen your plan. This proactive mindset transforms a moment of weakness into a source of future strength, making sure one bad day doesn’t throw your entire journey off track.
Your Personalized Recovery Action Plan
It’s time to take everything you’ve learned about your recovery and turn it into a practical roadmap you can actually use. A generic plan just won’t cut it because your journey is entirely your own. The idea is to build a living document—a personalized action plan that can grow and change right along with you. This isn’t about setting strict, unbreakable rules; it’s about creating a flexible guide for how to prevent relapse by being ready for real-world situations.
Think of it as a custom user manual for your sobriety. It needs to spell out what works for you and what your game plan is when things get hard. A solid plan is your safety net, there to catch you before a small slip becomes something much more serious.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Building Your Actionable Checklist
Your plan needs to be simple and easy to pull up, especially when you’re in a tough spot. Let’s break down the must-have pieces. You can start by jotting these down in a notebook or even in a note on your phone.
- Your Top 3 Triggers: Be honest and specific. List the three biggest things—whether they are people, places, or feelings—that are most likely to spark a craving.
- Your 3 Emergency Contacts: Write down the names and numbers of three people you can call anytime, day or night. Make sure these are people who get it and support your recovery.
- Your 2 Go-To Coping Skills: What are two positive actions you can take the second a craving hits? For example, “Take a 15-minute walk around the block,” or “Put on my recovery playlist and do some deep breathing.”
- Your “Why” Statement: This is a single, powerful sentence to remind you why you started this journey. Maybe it’s, “I want to be fully present for my family,” or “I am building a life I can be proud of.”
Setting Realistic Milestones
Instead of getting bogged down by a huge, vague goal like “stay sober forever,” break it down into smaller, achievable milestones. This approach helps you build momentum and gives you wins to celebrate along the way, which is great for your confidence.
| Milestone | Realistic Goal | Reward |
|---|---|---|
| First 30 Days | Attend every single one of my scheduled meetings and therapy sessions. | Treat myself to a new book or album I’ve been wanting. |
| 90 Days | Go to a high-risk social event (like a party or family dinner) and successfully stay sober. | Plan a fun weekend trip to a new city or a beautiful park. |
| 6 Months | Offer to mentor or support someone who is newer to recovery than I am. | Sign up and pay for a class to learn a new skill or hobby. |
This plan is your personal promise to yourself. It’s a real tool that shifts your recovery from just reacting to crises to proactively creating a life you truly want to live.
Your journey is yours alone, but you don’t have to walk it by yourself. If you’re feeling overwhelmed or just need to talk to someone right now, the Addiction Helpline America is available 24/7. Our trained team offers free, confidential support and can help you find the resources you need to stay on your path. Call us anytime at (844) 561-0606 or visit us at https://addictionhelplineamerica.com.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.