The journey into rehab doesn't start with a packed bag or a phone call. It starts with a quiet, courageous moment of honesty—the moment you admit that something has to change. It's about recognizing that substance use isn't just a part of your life anymore; it's negatively impacting all of it. From there, it’s about overcoming the internal barriers and making that first crucial call to a confidential helpline.
Deciding When It’s Time for Professional Help
Choosing to get help is, without a doubt, the hardest part of the entire process. It’s a step that goes way beyond a simple checklist. It’s about taking a hard look at how substance use is affecting your life, your relationships, and your future. Realizing you need support isn't a sign of weakness—it's a profound act of strength.
This decision usually doesn't happen overnight. It’s often the result of a series of quiet alarms going off. Maybe your performance at work is slipping, or important relationships feel constantly strained. Perhaps you find yourself hiding how much you're really using from the people you love. These aren't just isolated incidents; they're symptoms of a pattern, showing that control is slipping through your fingers.
Recognizing the Real-World Signs
The signs that you need professional help are rarely the dramatic, made-for-TV moments people imagine. More often, it's a slow, steady erosion of your daily life and well-being. Getting brutally honest with yourself is the only way to see these signs for what they are.
Do any of these scenarios hit a little too close to home?
- Relationship Strain: Are you arguing more with family or friends, especially about your substance use or the behavior that comes with it? Do you feel a growing distance from people who used to be your support system?
- Career or School Troubles: Have you been missing deadlines, calling in sick too often, or just noticing a general decline in the quality of your work? For a lot of people, facing real professional consequences is the first undeniable sign that things are out of hand.
- Neglected Responsibilities: Are bills piling up unpaid? Is the house a mess? Has even basic personal hygiene taken a backseat? When the core tasks of managing your life start to fall apart, it’s a major red flag.
- Loss of Interest: Remember the hobbies and activities that used to bring you joy? If you've stopped doing them, it’s often because addiction has a way of narrowing your entire world until the substance is the only thing left in focus.
If these situations feel familiar, it’s a strong signal that the problem has grown beyond your ability to manage it on your own. This isn't a moral failing; it's the clinical nature of addiction.
Overcoming Denial and Stigma
Denial is a powerful force. It’s that voice in your head whispering, "I can stop anytime I want" or "It’s really not that bad." It takes incredible courage to push past that voice and face the truth, especially when the stigma around addiction adds a heavy layer of shame and fear.
Admitting you need help is the first, most powerful step you can take. It’s not about giving up; it’s about choosing to fight for your life on your own terms.
The fear of being judged can feel paralyzing, but you are far from alone in this. The need for effective addiction treatment is growing, which means there are more accessible and varied options available for everyone. In fact, the global addiction treatment market is projected to hit about USD 16.22 billion by 2034, a number that reflects the rising need for quality rehab services.
This growth is good news for anyone seeking help—it means more resources, better support systems, and more specialized care are available than ever before. You can explore more data on the expanding addiction treatment market to see just how much this field is evolving.
How to Find the Right Rehab Program for You
You’ve made the decision to get help, and that’s a huge first step. But what comes next can feel like trying to find a single path in a forest of options. With so many different kinds of rehabs out there—inpatient, outpatient, various therapies—it’s easy to get overwhelmed.
The secret is to find a program that fits your life, not to try and force yourself into a program that doesn't. The right choice depends on your specific situation: the severity of your addiction, whether you’re also dealing with anxiety or depression, and your daily commitments to work or family. What works for someone else might not be the right fit for you.
Different Flavors of Rehab: What Are Your Options?
Not all rehab programs are built the same. Getting a handle on the main differences is the best way to make a choice you feel confident about. It's like picking the right tool for a job—you need one that's designed for what you're facing.
The options can seem endless, but they generally fall into a few key categories:
- Inpatient or Residential Rehab: This is the most immersive option. You live at the facility 24/7, which creates a safe, structured environment completely removed from daily triggers. It's often the best choice for those with severe addiction, co-occurring mental health conditions, or an unstable living situation back home.
- Outpatient Rehab: If you have a solid support system and need to keep up with work or family life, outpatient programs offer a lot of flexibility. You live at home and go to the center for therapy sessions several times a week.
- Partial Hospitalization Programs (PHP): Think of this as a middle ground. It's a step down from inpatient care, where you spend several hours a day at the facility (usually five to seven days a week) but go home in the evenings.
- Intensive Outpatient Programs (IOP): This is a bit less time-intensive than a PHP. Treatment usually involves a few hours a day, a few times a week, which really helps you practice applying recovery skills to your real life while still getting consistent support.
With the global drug addiction treatment market projected to grow past USD 31.20 billion by 2032, there's a clear and growing focus on providing effective, evidence-based care. In fact, therapy and counseling make up more than half of that market. This just goes to show how central quality therapeutic support is to achieving lasting recovery.
Comparing Rehab Program Types
To help you see the differences side-by-side, here’s a quick breakdown of the main program types. Think about your personal needs, responsibilities, and the level of support you think will give you the best shot at success.
| Program Type | Best For | Structure | Typical Duration |
|---|---|---|---|
| Inpatient/Residential | Severe addiction, dual diagnosis, unstable home environment. | 24/7 care, living on-site in a structured environment. | 30 to 90 days, or longer. |
| Partial Hospitalization (PHP) | Stepping down from inpatient or needing intensive care without 24/7 supervision. | 5-7 days/week, 6-8 hours/day at the facility. Return home at night. | 2 to 4 weeks. |
| Intensive Outpatient (IOP) | Moderate addiction, strong support system, need to maintain work/school. | 3-5 days/week, 3-4 hours/day at the facility. | 4 to 8 weeks. |
| Standard Outpatient | Mild addiction, stepping down from IOP, or as aftercare support. | 1-2 days/week, 1-2 hours/day for therapy and group sessions. | Ongoing, as needed. |
Ultimately, this table is just a guide. The best program for you will align with your clinical needs and personal circumstances.
Questions You Absolutely Must Ask an Admissions Team
When you start calling rehab centers, don't be passive. Treat it like an interview—because you are interviewing them to see if they're worthy of your trust, time, and money. A good admissions team will be transparent and patient. If you feel rushed, pressured, or like they're dodging your questions, that’s a major red flag.
Here are the essential questions you should have on your list:
- What accreditations and licenses do you hold? You want to see state licensing and accreditation from respected organizations like The Joint Commission or CARF.
- What’s your staff-to-patient ratio? A lower number here usually means more personal attention.
- What specific types of therapy do you use? Ask if they use evidence-based methods like Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), or trauma-informed care.
- Do you treat co-occurring disorders? This is non-negotiable if you’re also dealing with anxiety, depression, or PTSD. You need an integrated program.
- Can you walk me through a typical day? This gives you a real feel for the daily structure and rhythm of the program.
- How do you involve family in the treatment process? Family support can be a game-changer, so see what their approach is.
- What does your aftercare planning look like? Recovery is a long-term game. A solid plan for what happens after you leave is crucial for preventing relapse.
For a more comprehensive look at this process, feel free to check out our guide on how to choose the right rehab.
Finding the right rehab isn’t about finding the "best" facility—it's about finding the best facility for you. Your unique history, needs, and goals should be the driving force behind your decision.
Choosing where to go for treatment is a big deal. By taking the time now to do your homework, ask the tough questions, and trust your intuition, you’re setting yourself up for success in an environment where you can truly begin to heal.
Navigating Insurance and Paying for Treatment
The price tag on rehab can feel overwhelming, but it should never be the reason you or a loved one don't get help. It’s a real concern, but you have far more options than you might realize. Figuring out your insurance and exploring other ways to pay can turn what feels like a roadblock into just another step on the path.
The good news is that laws like the Affordable Care Act (ACA) require most insurance plans to cover mental health and substance use treatment the same way they cover a broken arm or diabetes. This has opened the door to recovery for millions. That said, every insurance policy is a little different, and the terminology can be a real headache.
Cracking the Code of Your Insurance Policy
Before you can use your benefits, you have to understand what they are. The best place to start is by calling the member services number on the back of your insurance card. When you call, have your policy information handy and be ready to take some good notes.
To get a clear picture of what's covered, here are the key questions you need to ask:
- Does my plan cover substance abuse treatment? Be specific. Ask about medical detox, inpatient residential stays, and outpatient programs.
- What is my deductible? This is the amount you’ll have to pay out-of-pocket before your insurance kicks in.
- What are my copayments and coinsurance? A copay is a flat fee for a service. Coinsurance is the percentage of the cost you’re on the hook for after you've met your deductible.
- Do I need pre-authorization for treatment? This is a big one. Many plans require the rehab facility to get approval before you check in for them to cover the stay.
- Is there a limit on the number of days or sessions covered? Knowing this upfront helps you and the treatment team create a realistic plan.
Don't hang up until you understand the answers. If you hear a term you don't know, ask them to explain it in simple language. For a deeper dive, you can explore our detailed guide on whether your insurance will cover drug rehab.
What to Do If You Don't Have Insurance
If you don’t have insurance, please don’t lose hope. It might feel like a dead end, but the path to rehab is still wide open. There are resources out there designed specifically for this situation.
Governments and health organizations get it—access to treatment is a critical public health issue. The World Health Organization (WHO) consistently highlights the need for countries to beef up their substance abuse prevention and treatment services. In the U.S. alone, the 2024 National Drug Control Budget requested $21.8 billion to expand access to care, which shows a serious national commitment to making recovery possible for everyone.
Your financial situation does not define your worthiness of recovery. There are systems in place designed to help you access life-saving care, regardless of your ability to pay.
Exploring Alternative Funding for Rehab
When insurance isn't in the picture, it's time to get a little resourceful. Many people successfully fund their treatment by combining a few different methods.
Here are the most common avenues to explore:
- State-Funded Programs: Every state gets federal money to provide addiction treatment to residents who can’t afford it. The best way to start is by contacting your state’s substance abuse agency to find out if you're eligible and which facilities participate.
- Sliding Scale Fees: Many non-profit and even some private rehab centers offer a "sliding scale." This simply means they adjust the cost of treatment based on your income to make it much more affordable.
- Financing and Payment Plans: Some facilities have their own in-house financing, allowing you to pay for your treatment in manageable monthly installments after you’ve completed the program. Think of it as an investment in your future.
- Grants and Scholarships: Organizations like the Substance Abuse and Mental Health Services Administration (SAMHSA) provide grants to help people cover the cost of rehab. It takes some research, but these opportunities can dramatically reduce the financial burden.
Finding the right financial solution takes some legwork, but it's a crucial part of the process. By exploring all these options, you can piece together a plan that makes getting into rehab a reality.
What to Expect During the Admissions Process
You’ve made the courageous decision to get help. That’s huge. Now comes the admissions process, which can feel like a whole new mountain to climb. But I want to reframe that for you—think of it less as a test and more as a conversation. It's the first step where you and a team of professionals start building your recovery plan together. The goal is simple: make sure you land in a place that's safe, effective, and right for you.
Everything kicks off with a confidential phone call. You’ll be talking to an admissions coordinator, and I can tell you from experience, these are some of the most compassionate and non-judgmental people you’ll ever meet. Their job is to listen, answer your questions, and start piecing together the information needed to get you on the right path.
The Initial Assessment and Why Honesty Matters
During that first call, the coordinator will walk you through a pre-assessment. They’ll ask about your substance use history, your current home life, and your general physical and mental health. This isn't meant to be invasive; it’s the essential groundwork for matching you with the proper level of care.
You can expect questions along these lines:
- What substances have you been using, and for how long?
- Can you describe the frequency and amount of use?
- Do you have any other health conditions, like diabetes or high blood pressure?
- What prescription medications are you currently taking?
- Have you ever been diagnosed with anxiety, depression, or another mental health condition?
Let me be direct: being completely honest here is absolutely critical. I've seen situations where people held back details, and it led to serious medical complications during detox. The clinical team uses this information to build a plan that keeps you safe.
The admissions process isn't a test you can fail. It's the first step in a partnership designed to build a foundation for your recovery. Your honesty provides the blueprint for your care plan.
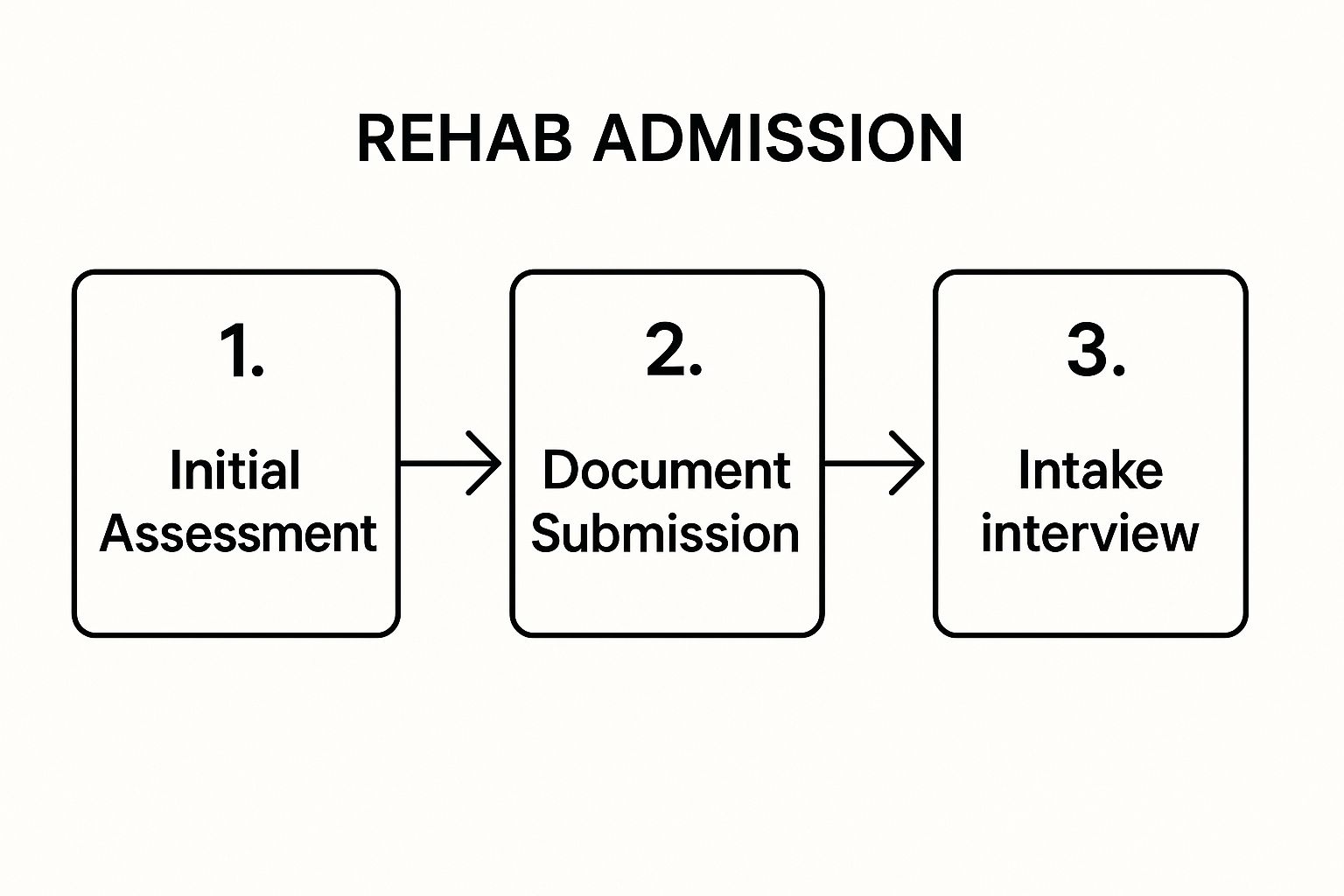
The whole process is designed to be thorough yet supportive, guiding you from that initial phone call right up to the moment you walk through the doors.
As you can see, it’s a logical flow. You start by sharing information, move on to handling the paperwork, and finish with your in-person intake.
To help you keep track of everything, here’s a simple checklist that breaks down the major milestones you can expect.
Admissions Process Checklist
| Stage | Key Action | What to Prepare |
|---|---|---|
| Initial Call | Speak with an admissions coordinator for a pre-assessment. | A quiet, private space to talk openly. |
| Insurance Verification | The admissions team confirms your benefits with your provider. | Your insurance card and policy information. |
| Clinical Review | The facility’s medical team reviews your information. | A list of your current medications and doctors. |
| Travel & Logistics | Coordinate your arrival date and travel arrangements. | Your travel itinerary and personal calendar. |
| Arrival & Intake | Complete final paperwork and meet the clinical team. | Photo ID, insurance card, and essential items. |
Following these steps will help ensure a smooth and organized transition into treatment.
Verification and Documentation
Once the initial assessment is done, the admissions team takes over the logistical heavy lifting. This is where they handle insurance verification and help you gather all the necessary documents. The staff will contact your insurance provider directly to figure out exactly what your benefits cover—from detox to inpatient and outpatient services.
They'll give you a clear picture of any out-of-pocket costs, like deductibles or copays, so you're not hit with any surprises down the road. Honestly, this is a massive weight off most people's shoulders, as the team navigates all the confusing insurance jargon for you.
You'll also need to get a few key documents ready:
- A government-issued photo ID (a driver's license or passport works great)
- Your health insurance card
- A list of all prescription medications you're currently taking
Having this small pile of paperwork ready makes your arrival day much smoother. To get an even clearer idea of what comes next, you can learn more about what to expect in rehab and feel more prepared for your first 24 hours.
Your Arrival and Intake
When you arrive on your admission day, staff will be there to welcome you and guide you through the final steps. It usually starts with an in-person intake interview with a counselor, which is a bit more in-depth than the first phone call.
You’ll also sit down with a nurse or doctor for a physical health screening. This is where they finalize your medical care plan and any detox protocols. After that, you'll get a tour of the facility, be shown to your room, and have some time to settle in before you meet your primary therapist and the other residents. It’s a structured and welcoming approach designed to help you feel safe and supported from the moment you arrive.
Preparing Yourself for a Successful Stay in Rehab
Getting ready for rehab is about more than just tossing some clothes in a bag. The groundwork you lay before you even walk through the door can genuinely shape your entire experience and pave the way for a lasting recovery. Think of it as clearing the deck so you can focus 100% on yourself and your healing.
This is your time to handle all the logistical headaches and outside noise. That means navigating those tough conversations with your boss and family, knowing your legal rights, and, most importantly, getting into a solid headspace. Tying up these loose ends creates a kind of protective bubble, letting you immerse yourself in the work ahead without distractions pulling you back.
Handling Work and Family Conversations
The thought of telling your employer you need time off for treatment can be terrifying. It's natural to worry about being judged or even losing your job. The good news is, there are protections in place for exactly this situation.
The Family and Medical Leave Act (FMLA) is a big one. This federal law gives eligible employees the right to take up to 12 weeks of unpaid, job-protected leave for serious medical reasons—and yes, treatment for a substance use disorder absolutely qualifies.
You don't have to spill all the personal details to your employer. Your privacy is protected. Simply explaining that you need to take medical leave on the advice of a healthcare provider is enough.
When you talk to HR, keep it professional and frame it as a medical necessity. You could say something like, "I need to take a medical leave of absence starting on [start date]. I can provide the required documentation from my doctor." This approach gets you the time you need while keeping your personal health information confidential.
What to Pack and What to Leave Behind
When it comes to packing, less is definitely more. Your focus should be on bringing things that will support your recovery, not distract from it. Every facility will give you a specific list, but some general rules always apply.
What to Bring:
- Comfy Clothes: Plan for about a week's worth of casual, modest clothing. Think sweatpants, t-shirts, hoodies—anything you feel comfortable in. If they have a gym or pool, pack workout clothes and a swimsuit.
- Personal Hygiene Items: All your toiletries (shampoo, soap, toothpaste, etc.) should be new, unopened, and alcohol-free.
- Key Documents: Don't forget your driver's license or ID, your insurance card, and maybe a small bit of cash for a vending machine.
- Contact List: A written list of phone numbers for family, friends, or any legal or medical contacts you might need.
- A Journal and Pen: Writing can be an incredibly powerful outlet. It's a space to process everything you're thinking and feeling as you go through treatment.
What to Leave at Home:
- Electronics: Laptops, tablets, and often even cell phones are usually a no-go. The idea is to disconnect from the outside world and focus on your inner one.
- Revealing Clothing: Avoid anything overly tight, short, or clothes with logos related to alcohol or drugs.
- Outside Food and Drinks: Your meals and snacks are all part of the program, so you won't need to bring your own.
- Valuables: To avoid any risk of loss or theft, it's best to leave expensive jewelry, large sums of money, or irreplaceable sentimental items safely at home.
For a more comprehensive rundown, check out our detailed guide on how to prepare for rehab to make sure you have all your bases covered.
Getting Mentally and Emotionally Ready
Honestly, your mindset walking in is one of the biggest predictors of success. It's completely normal to feel a storm of emotions—anxiety, fear, even a little hope. The key is to acknowledge those feelings without letting them take over.
Try to set realistic expectations. Recovery isn't a straight line from sick to cured; it's a journey with twists, turns, and bumps. You're going to a place to learn and heal, not to get a 30-day "fix." Embrace the entire process, even the parts that are hard. That's where the real growth happens.
Here’s a practical tip I've seen work wonders: write a letter to your future self. Before you go, sit down and pour it all out. Write down why you're doing this, what your biggest fears are, and what you hope life will look like on the other side. Give it to your therapist to hold onto, and ask for it back on a day when you're struggling. It's a powerful reminder of the commitment you made to yourself.
Common Questions About Getting Into Rehab
When you start looking into rehab, a million questions probably pop into your head. That’s completely normal. You're likely feeling a mix of hope, fear, and a whole lot of uncertainty. Let's walk through some of the most common concerns I hear from people and get you some straight answers.
Will I Lose My Job If I Go to Rehab?
This is easily one of the biggest fears holding people back. The good news is, you likely have more protection than you realize.
The Family and Medical Leave Act (FMLA) is a federal law that can be a lifesaver here. For employees who qualify, it provides up to 12 weeks of unpaid, job-protected leave for serious medical conditions. And yes, seeking treatment for a substance use disorder absolutely counts.
When you talk to your employer, you don't have to spill every detail. The conversation can be discreet and professional. You're not required to disclose your specific diagnosis; simply explaining that you need to take a medical leave advised by a doctor is often enough. Your HR department is the best place to start—they can walk you through the paperwork without compromising your privacy.
What Is Rehab Actually Like Day-to-Day?
It's natural to wonder what you'll do all day. While every rehab has its own vibe, they all share one key element: structure. This isn't about control; it's about replacing the chaos of addiction with a predictable, healing rhythm.
Here’s a glimpse of what a typical day might involve:
- Mornings usually kick off with breakfast and a group therapy session. You might also have educational classes on topics like understanding addiction, building coping skills, or practicing mindfulness.
- Afternoons are often dedicated to more personalized care. This is when you'll likely have your one-on-one therapy sessions, specialized groups (like trauma or grief counseling), and holistic activities like yoga, art, or time at the gym.
- Evenings tend to wind down with dinner, followed by a 12-step meeting or a group reflection on the day. You'll also get some personal time to journal, read, or just relax before lights out.
The whole point of this structured environment is to create a safe space. It allows you to focus 100% on getting better, free from the triggers and stresses of your daily life.
This routine isn't just about passing the time. It’s about building the healthy habits and discipline that will become the foundation of your recovery.
Can I See My Family or Have My Phone?
Yes, but there are usually some ground rules. Everyone in the field knows that family support is crucial for recovery. At the same time, the first few days are all about you—settling in and focusing without distraction.
Most treatment centers have what’s called a "blackout" or "acclimation" period. This typically lasts for a few days to a week. During this time, contact with the outside world is limited to give you a chance to get your bearings.
After that initial phase, you'll be able to have scheduled visits and make phone calls during designated times. Many facilities also offer family therapy sessions, which can be incredibly powerful for healing broken trust and building a solid support network for when you get home.
How Much Is This Going to Cost Me?
Let's be real: cost is a huge concern. The price of rehab can vary dramatically depending on the program, location, and level of care you need. But please, don't let the fear of cost stop you from reaching out.
As we discussed earlier, your health insurance will likely cover a big chunk of the bill. Beyond that, there are so many other ways to manage the expense.
Getting a handle on the financials is a critical step. For a much deeper dive into the numbers and payment strategies, you'll find a lot of helpful information by reading more about how much rehab costs and how to find an affordable option.
From state-funded programs and scholarships to facilities with sliding scale fees, resources exist to make sure cost isn't a barrier. This is an investment in your life—and it's the most important one you'll ever make.
At Addiction Helpline America, we're here 24/7 to help you sort through these questions and figure out your next step. Our team will listen without judgment and guide you toward the right options. Call us anytime at https://addictionhelplineamerica.com.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Call Now for 24/7 Free Confidential Addiction Support
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.