
The simplest answer for how to get addiction help is also the most human: it starts with admitting there’s a problem, finding someone you trust to talk to, and then looking into what professional help is out there. This whole journey kicks off with a single, brave decision to choose a healthier life for yourself.
Taking the First Step: Recognizing You Need Help
Admitting you or someone you care about needs help is, without a doubt, the hardest part of the entire process. It’s a moment packed with a messy mix of emotions—fear, shame, but also, surprisingly, a huge sense of relief. Taking this first step isn’t a sign of weakness. It’s an act of incredible strength.
The red flags that substance use has crossed a line can be sneaky at first. They often show up as small, easy-to-justify changes in your everyday life.
- Strained Relationships: Are arguments about your substance use becoming more frequent? Are you pulling away from friends and family to avoid their questions?
- Trouble at Work or School: Maybe performance has slipped, deadlines are being missed, or you’re calling out sick more often because of hangovers or just not caring anymore.
- Declining Health: You might be ignoring physical or mental health problems, blaming them on stress instead of the substance itself.
- Loss of Interest: Hobbies and activities that used to bring you joy now feel like a chore compared to using.
Seeing these patterns for what they are is a critical moment of clarity. For many, this isn’t a single “rock bottom” event but a slow burn—a dawning realization that life has become unmanageable.
Getting Past Denial and Fear
Denial is a powerful reflex. It’s that voice in your head whispering, “It’s not that bad,” or “I can quit whenever I want.” Fear is usually what’s fueling it—fear of being judged, fear of the unknown, and a deep fear of what life will look like without the substance you rely on.
“Acknowledging the problem is the first, and often hardest, part of recovery. It’s where you stop running from the issue and start moving toward a solution. This shift in perspective reframes seeking help from a moment of defeat to an act of empowerment.”
If you’re reading this, you are far from alone. The scale of substance use is massive; according to the UNODC World Drug Report 2025, roughly 316 million people used drugs in 2023. Yet, a huge treatment gap exists, often because of the very stigma and fear you might be feeling right now.
When you’ve decided to seek help, the first few actions can feel daunting. The table below breaks down the immediate, concrete steps you can take to build a solid foundation for your recovery.
Initial Steps to Getting Addiction Help
| Action Step | Why It’s Important | Who Can Help |
|---|---|---|
| Acknowledge the Truth | Saying it out loud—even just to yourself—breaks the power of denial and makes the problem real. | Yourself, a private journal. |
| Confide in Someone Safe | Sharing your struggle with one trusted person relieves isolation and creates an ally. | A spouse, a close friend, a family member you trust not to judge. |
| Contact a Professional | This is your first step toward a real, structured plan. They provide objective guidance. | A family doctor, a therapist, or a confidential addiction helpline. |
These steps are about taking that internal realization and turning it into external action. Each small move builds on the last, guiding you from a place of uncertainty toward a clear path of healing. Taking these first steps to recovery is a process you can start right now, creating the momentum you need for the journey ahead.
Understanding Your Addiction Treatment Options
Once you’ve made the decision to get help, the next question is, “What kind of help do I need?” It’s a big one. The world of addiction treatment isn’t a single path; it’s a whole spectrum of care designed to meet you exactly where you are. Finding the right fit for your personal situation, your needs, and your life is the key to getting started on solid ground.
The path from recognizing a problem to getting help often follows a simple but powerful sequence. This visual breaks down that core process.
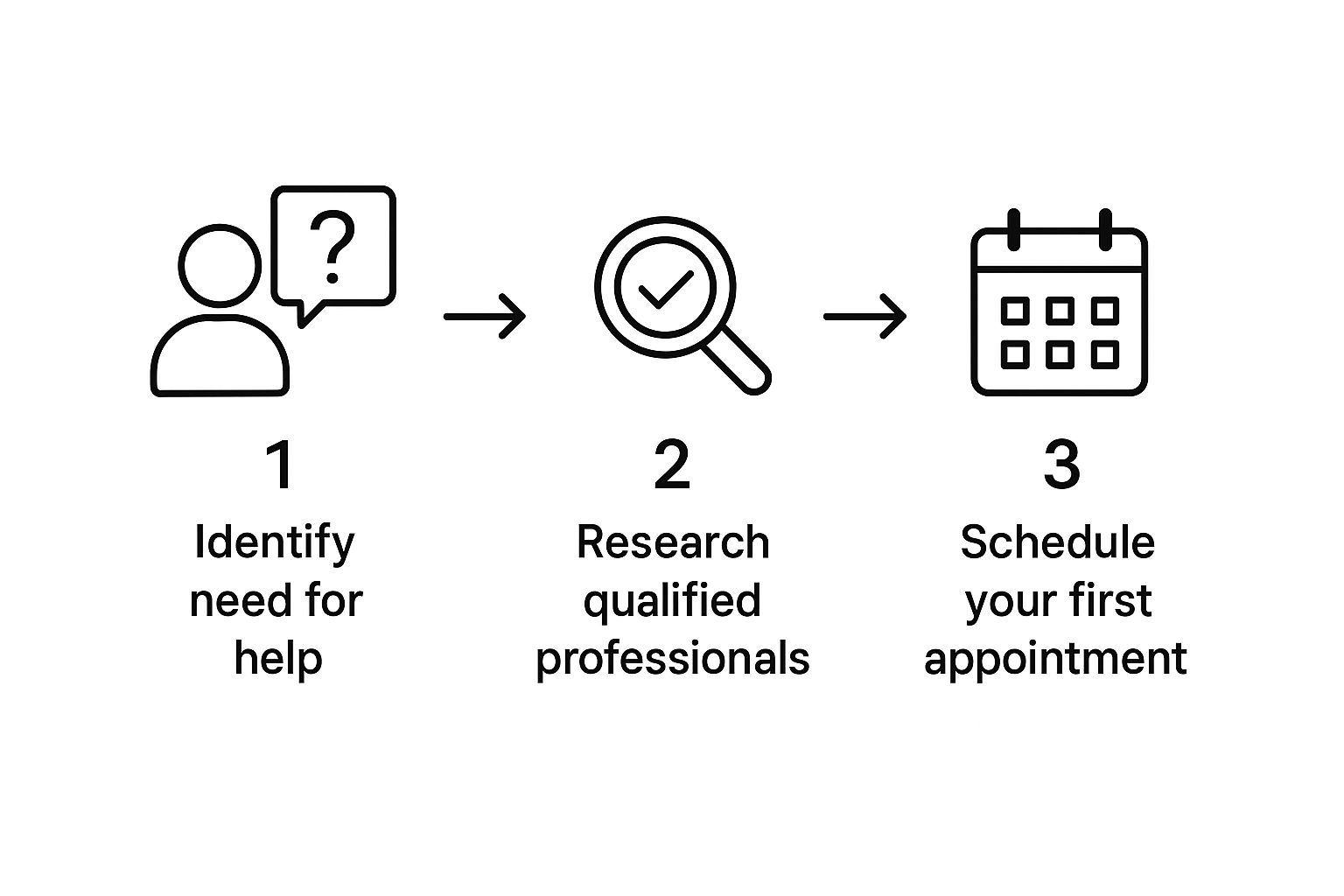
This isn’t just a flowchart; it’s a reminder that recovery is an active journey. It starts with awareness and moves toward professional support, with each step building on the one before it.
Diving Into Different Levels of Care
Addiction treatment is structured by intensity, often called “levels of care.” This framework makes sure you get the right amount of support—not so little that it’s ineffective, and not so much that it completely upends your life unnecessarily. The goal is always to match the program to the person.
Some of the most common options include:
- Medical Detoxification: This is often the first stop for anyone with a physical dependence on substances like alcohol, opioids, or benzodiazepines. It’s a medically supervised process designed to manage withdrawal symptoms safely and make you as comfortable as possible.
- Inpatient or Residential Treatment: This is the most immersive and intensive level of care. You live at the treatment facility 24/7, receiving a highly structured schedule of therapy, counseling, and medical supervision.
- Outpatient Programs: These programs offer flexibility. You live at home and travel to a treatment center for sessions during the day or evening, which allows you to keep up with work, school, or family life.
So, how do you choose? It really depends on your specific circumstances. Someone with a long-term, severe addiction and an unstable home environment would probably get the most out of the structure and safety of inpatient care. On the other hand, a person with a strong support system and a less severe substance use disorder could thrive in an outpatient setting.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Comparing Addiction Treatment Program Types
To help you visualize the differences, this table breaks down the most common types of addiction treatment. Use it to get a clearer picture of which approach might be the best fit for your situation.
| Treatment Type | Best For | Level of Intensity | Typical Duration |
|---|---|---|---|
| Inpatient/Residential | Severe SUDs, unstable home environments, co-occurring disorders. | Highest | 30-90+ days |
| Partial Hospitalization (PHP) | Step-down from inpatient; needs significant structure but has a stable home. | High | 3-5 weeks |
| Intensive Outpatient (IOP) | Moderate SUDs; needs more than weekly therapy but requires flexibility. | Medium | 6-12 weeks |
| Standard Outpatient | Mild SUDs, strong support system, or for aftercare. | Low | Varies |
| Medical Detox | Physical dependence on substances like alcohol, opioids, or benzos. | Varies (High supervision) | 3-10 days |
Each of these programs serves a vital purpose. The right one for you depends entirely on where you are in your journey and the level of support you need to succeed.
A Closer Look at What Happens in Treatment
Let’s demystify what these programs actually look like day-to-day. Knowing what to expect can make the whole process feel much more manageable.
“The foundation of any quality treatment program is evidence-based therapy. This isn’t just unstructured talking. It’s using proven methods like Cognitive Behavioral Therapy (CBT) or Dialectical Behavior Therapy (DBT) to help you understand your triggers and build healthy, practical coping skills.”
What to Expect in Inpatient Residential Programs A day in residential care is structured from morning to night. Your schedule might include group therapy after breakfast, followed by one-on-one counseling, workshops on the science of addiction, and even holistic activities like yoga, art therapy, or fitness. This immersive setting pulls you away from daily triggers and gives you the space to focus entirely on recovery.
The Different Flavors of Outpatient Programs (OP) Outpatient care isn’t a single thing; it comes in different intensities:
- Partial Hospitalization Programs (PHP): This is the most intense outpatient option, often called “day treatment.” It typically involves 5-8 hours of programming per day, 5 days a week. It’s a great step-down from inpatient care.
- Intensive Outpatient Programs (IOP): A step below PHP, IOPs usually require 9-20 hours of treatment per week. This is often broken into 3-hour sessions, 3 to 5 days a week.
- Standard Outpatient: The least intensive option, this usually involves just one or two therapy sessions per week, perfect for aftercare or for those with mild SUDs.
The Role of Medication and Technology
For many people, medication is a game-changer. Medication-Assisted Treatment (MAT) is an approach that combines behavioral therapies with FDA-approved medications to treat substance use disorders. These medications work by reducing cravings, managing withdrawal, or blocking the euphoric effects of alcohol and opioids. For opioid use disorder, medications like buprenorphine and naltrexone have proven to be incredibly effective.
If you want to dig deeper into this, you can learn what medication-assisted treatment is in our detailed guide.
Technology is also playing a bigger role than ever. The substance abuse treatment market is projected to hit USD 13.75 billion by 2030, with a huge part of that growth coming from digital health. Telehealth platforms are making therapy and counseling more accessible, breaking down barriers like distance or stigma to provide the kind of ongoing support that is so vital for lasting recovery. Help is truly closer and more accessible than you think.
How to Find the Right Treatment Center for You
Choosing a facility is hands-down one of the biggest decisions you’ll make on the road to recovery. With what seems like a million options out there, it’s incredibly easy to feel lost. The goal isn’t just finding any center; it’s about finding the right one that truly gets your personal history, your specific needs, and your current situation.
Think of it like this: you wouldn’t see a foot doctor for a heart problem. Addiction treatment is no different. It’s most effective when the program is a solid match for the person. This is a critical piece of the puzzle in getting addiction help that actually works.
Start with Reputable Resources
Your first move should be to pull together a list of potential centers using trusted, unbiased sources. This is your best defense against predatory programs, helping you focus only on facilities with a proven track record of ethical care.
A fantastic starting point is the National Helpline from the Substance Abuse and Mental Health Services Administration (SAMHSA). It’s a free, confidential service that can give you referrals to local treatment facilities, support groups, and other community organizations.
“When you’re looking at a facility, accreditation is non-negotiable. Look for seals of approval from organizations like The Joint Commission or the Commission on Accreditation of Rehabilitation Facilities (CARF). This is your guarantee that the center is held to high standards for quality and patient care.”
Key Questions to Ask the Admissions Team
Once you have a shortlist, it’s time to put on your consumer hat. Call the admissions department for each facility, but go in prepared with a list of specific questions. How they answer will tell you everything you need to know about their approach to treatment and the quality of their program.
Here’s a practical checklist to guide those important conversations:
- What evidence-based therapies do you use? You want to hear them talk about scientifically proven methods like Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), or Motivational Interviewing. Vague, fuzzy answers are a major red flag.
- What is your staff-to-client ratio? A lower ratio, something like one staff member for every 5-8 clients, typically means more one-on-one attention.
- How do you handle dual diagnosis? This is a big one. Roughly 50% of people with a severe mental illness also have a substance use disorder. If you’re dealing with depression, anxiety, or another mental health condition, you absolutely need a program that can treat both at the same time.
- What are your staff’s credentials? Don’t be shy. Ask about the qualifications of the clinical team. Are the therapists licensed? Is there a medical doctor on staff?
- What does a typical day look like? A high-quality program should have a full, structured schedule packed with therapeutic activities, not a lot of unstructured free time.
- Do you offer specialized programs? If it’s relevant to your situation, ask about things like gender-specific groups, programs for certain age groups, or treatment tracks that focus on specific substances like opioids or alcohol.
Taking the time to gather this information is a huge part of the process. For an even more detailed breakdown, our guide on choosing the right rehab facility dives deeper into what to look for.
Identifying Potential Red Flags
Knowing what to look for is only half the battle; you also need to know what to avoid. Some facilities are more interested in their bottom line than in patient outcomes. Be on high alert for any program that feels “off” or uses questionable tactics.
Common Red Flags to Watch Out For
| Red Flag | Why It’s a Problem |
|---|---|
| Guarantees of a “Cure” | Addiction is a chronic disease, and there is no magic cure. Good centers talk about recovery management and relapse prevention, not a one-and-done fix. |
| Vague Treatment Models | If they can’t clearly explain their therapeutic methods or lean heavily on non-clinical activities, the program probably lacks real clinical substance. |
| High-Pressure Sales Tactics | Admissions staff should be helpful and informative. If they sound more like a pushy salesperson trying to get a deposit right now, run the other way. |
| Lack of Transparency | A trustworthy facility will be completely open about its costs, rules, and treatment protocols. If they hesitate to answer your direct questions, it’s a bad sign. |
Doing this homework and asking the tough questions will empower you to find a program that not only feels right but is also clinically sound. This due diligence is your best tool for getting the effective addiction help you truly deserve.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Navigating the Costs of Addiction Treatment
Let’s be honest: the thought of paying for treatment can be a massive roadblock. For many people, the anxiety around cost is so overwhelming it stops them from even trying to get help. But I want to be very clear about this—cost should never be the final word on whether you or a loved one gets a chance at recovery.
There are more pathways to affordable, high-quality treatment than you might think. The key is knowing where to look and what questions to ask.
Decoding Your Insurance Benefits
If you have health insurance, your very first move should be to call your provider. This single conversation is crucial for figuring out exactly what your plan covers. Don’t just ask, “Is rehab covered?” You need to dig into the details to avoid any gut-wrenching surprise bills down the road.
When you dial the number on the back of your insurance card, have your policy information handy. Your goal is to get a crystal-clear picture of your financial responsibility.
You’ll want to get specific numbers for these terms:
- Deductible: This is the amount you have to pay out-of-pocket before your insurance plan starts contributing.
- Copayment (Copay): A flat fee you pay for a specific service, like a therapy session, after you’ve met your deductible.
- Coinsurance: The percentage of the bill you’re responsible for after your deductible is paid. For instance, your plan might cover 80%, leaving you with the remaining 20%.
- Out-of-Pocket Maximum: This is the absolute most you will have to pay for covered care in a plan year. Once you hit this cap, your insurance picks up 100% of the tab for covered services.
Knowing these figures ahead of time is the difference between feeling panicked and feeling prepared. For a deeper dive into this, take a look at our complete guide on paying for addiction treatment.
“It’s also critical to know your rights. The Mental Health Parity and Addiction Equity Act (MHPAEA) is a federal law that says most health plans can’t put stricter limits on addiction treatment than they do on other medical care. They have to play fair.”
What to Do If You Don’t Have Insurance
If you don’t have insurance or find that your coverage just isn’t enough, please do not lose hope. You still have excellent options for getting the help you need. Many top-tier treatment programs are accessible through other means.
Start by looking into state-funded and government-supported programs. Every state gets federal money specifically for substance use disorder treatment. These programs are often free or extremely low-cost for residents who qualify. A good place to start your search is on your state’s Department of Health website.
Here are a few other avenues worth exploring:
- Sliding-Scale Fees: Many non-profits, and even some private facilities, will adjust their prices based on what you can realistically afford. They “slide” the fee down to match your income.
- Scholarships and Grants: It never hurts to ask an admissions department if they offer financial aid. Some treatment centers have their own scholarship funds set up by donors to help people get care.
- Personal Financing: This option requires careful thought, but sometimes a personal loan is a practical way to cover the cost of a program that could save your life.
This growing range of financial support reflects a major shift in how we see addiction. The global addiction treatment market is currently valued at around USD 10.06 billion and is expected to grow. Why? Because of better public awareness and a wider understanding of addiction as a treatable medical condition, which is driving more accessible programs. You can find more details on these market trends from Coherent Market Insights.
The bottom line is this: financial hurdles can be overcome. It takes some persistence and the right information, but a path to affordable, life-changing care is out there.
Building Your Long-tTerm Recovery Support System
Graduating from a treatment program is a massive accomplishment. It’s a genuine turning point. But I’ve learned from experience that it’s crucial to see it for what it truly is: the starting line, not the finish. The real work of building a new, sober life begins the moment you walk out those doors, and you absolutely don’t have to do it alone.
This is where creating a solid support system becomes the most important part of your journey. This network is your safety net, your sounding board, and your team of cheerleaders all rolled into one. It’s a core part of getting addiction help that actually lasts.
Finding Your Community in Peer Support Groups
For millions of people, peer support groups are the bedrock of long-term recovery. There’s a unique kind of understanding you can only get from people who have walked a similar path. Finding the right group is really about finding a community where you feel seen, heard, and accepted without judgment.
Some of the most common and effective options include:
- Alcoholics Anonymous (AA) and Narcotics Anonymous (NA): These are the original 12-step programs. They are built on a foundation of fellowship, mutual support, and working through a set of spiritual steps with a sponsor.
- SMART Recovery: This group uses a different toolkit, pulling from science-based methods like cognitive-behavioral therapy (CBT). It’s all about self-empowerment and building practical skills to manage your thoughts, feelings, and behaviors.
- Refuge Recovery: If you connect with a more meditative approach, Refuge Recovery uses Buddhist principles and practices like mindfulness to guide people through healing from addiction.
I know walking into that first meeting can feel incredibly intimidating. Just remember, every single person in that room was a newcomer once. You don’t even have to speak if you don’t want to; just listening can be incredibly powerful. My advice is to try out a few different meetings and groups until one just clicks and feels like home.
The Critical Role of Friends and Family
While peer groups offer a special kind of camaraderie, reconnecting with trusted friends and family is just as vital. These are the people who knew you before and genuinely want to see you thrive. That said, these relationships might need some careful rebuilding.
Healing these connections takes time, patience, and a whole lot of honesty. Be open about your recovery journey, but also be ready to truly listen to their feelings. Family therapy can be an amazing tool to help repair trust and establish healthier communication patterns that protect your sobriety. The importance of support systems in recovery can’t be overstated; these personal connections provide a deep sense of belonging and accountability.
“Recovery isn’t just about stopping substance use; it’s about building a life so fulfilling and meaningful that you no longer need to escape from it. This new life is constructed one healthy relationship and one joyful experience at a time.”
Developing a Practical Relapse Prevention Plan
A relapse prevention plan is your personal roadmap for navigating the inevitable challenges of recovery. It’s a proactive strategy, not a sign of weakness or doubt. Thinking through potential triggers and creating a clear plan of action ahead of time empowers you to handle tough situations with confidence.
Make sure your plan is written down and shared with your therapist or a trusted support person.
Key Components of a Strong Relapse Prevention Plan
| Component | What to Include | Example |
|---|---|---|
| Identify Triggers | List specific people, places, things, and feelings that create cravings. | Stress from work deadlines; driving past a specific bar; feeling lonely on a Friday night. |
| Develop Coping Skills | Write down healthy actions you can take when a trigger appears. | Call my sponsor; go for a run; practice deep breathing exercises for 10 minutes; journal about my feelings. |
| Create an Emergency Contact List | List people you can call for immediate support, day or night. | Sponsor, therapist, a close friend in recovery, a trusted family member. |
| Build a Sober Lifestyle | Plan activities and hobbies that bring you joy and don’t involve substances. | Joining a hiking club; taking a pottery class; volunteering at an animal shelter; learning to play guitar. |
This isn’t a document you create once and forget about. Your plan should evolve as you grow in recovery. The real goal is to build a life filled with new passions and purpose. Discovering sober hobbies isn’t just about filling time—it’s about rediscovering who you are and what brings you genuine happiness.
Common Questions About Getting Addiction Help
The road to recovery is paved with questions. It’s natural to feel uncertain about how everything works, from telling your boss to figuring out if a loved one can be made to get help. We’ve been there, and we’ve heard it all. This section gives you straight answers to the questions we hear most often, so you can feel more confident taking the next step.
Can I Be Forced Into Rehab?
This is a big one, and a totally valid question. The short answer is, usually not. Addiction treatment is almost always a voluntary choice. Lasting recovery really only sticks when someone is personally motivated and ready to do the work. You can’t just check an adult into a treatment program against their will in most cases.
That said, there are some very specific legal situations where involuntary commitment can happen. These laws vary a lot from state to state but typically require a court order. This usually only happens when a person’s substance use makes them a legal danger to themselves or others. It’s a complicated legal process, so your best bet is to talk to a medical professional or a legal expert to understand the rules where you live.
What Should I Tell My Employer About Treatment?
Thinking about this conversation can be incredibly stressful. But here’s the good news: you have rights, and you don’t have to share every last detail of your personal health. Your privacy is protected.
Thanks to federal laws like the Family and Medical Leave Act (FMLA) and the Americans with Disabilities Act (ADA), your job may be protected while you seek treatment for a substance use disorder, which is legally recognized as a medical condition.
You can just tell your boss or HR that you need to take medical leave.
“You absolutely have a right to medical privacy. A simple, direct statement like, ‘I need to take a medical leave of absence for a personal health issue under my doctor’s supervision,’ is all you need to say. Your HR department will know exactly what to do and can walk you through the FMLA paperwork without you having to disclose the specifics of your treatment.”
HR professionals are trained to handle these requests with confidentiality. They’ll know the company’s policies and help you get things sorted.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
How Do I Help Someone Who Refuses Treatment?
Watching someone you love struggle with addiction and refuse help is one of the most painful experiences you can go through. It’s so important to remember that you can’t control their choices. You simply can’t force them to want to get better.
What you can do is change how you engage with them and the situation.
- Offer Support, Not Control: Let them know you love them and that you’ll be there to support their recovery when they’re ready.
- Set Healthy Boundaries: This is about protecting your own well-being. It might mean not giving them money, refusing to make excuses for their behavior, or setting clear rules about what’s acceptable in your home.
- Encourage, Don’t Preach: Lectures and ultimatums almost always backfire and just create more distance. Instead, look for moments where you can have an open, non-judgmental conversation.
- Get Professional Guidance: Working with a professional interventionist or a family therapist can be a game-changer. They can give you real strategies for communicating effectively and help you structure a conversation that’s designed to guide your loved one toward accepting help, not push them away.
Your role is to be a steady source of support. But ultimately, the decision to get help has to be theirs.
What Should I Pack for a Residential Program?
Knowing what to pack can make walking into a residential program feel a little less intimidating. Every facility has its own list of what’s allowed and what’s not, but some general rules apply almost everywhere.
What to Bring to Rehab
| Category | Examples |
|---|---|
| Comfortable Clothing | Bring about a week’s worth of casual, comfy clothes. Layers are always a good idea since you never know about the thermostat. If the facility has a gym or pool, pack workout clothes and a swimsuit. |
| Personal Toiletries | Stick to new, unopened, alcohol-free products. Think toothbrush, toothpaste, shampoo, soap, etc. Most places will check these items when you arrive. |
| Important Documents | Your driver’s license or ID, insurance card, and maybe a small amount of cash for vending machines are usually fine to bring. |
| Contact Information | It’s helpful to have a physical list of important phone numbers for family, friends, and doctors. |
| Comfort Items | A journal, some photos of loved ones, or a few recovery-focused books are often encouraged. These things can help you feel more grounded and focused on your goals. |
Before you start packing, always get the specific list from the facility’s admissions team. They’ll give you the exact rundown of what to bring and what to leave at home to ensure a safe and supportive environment for everyone.
If you or someone you know is ready to take the next step, you don’t have to figure it all out alone. Addiction Helpline America is here to connect you with compassionate professionals who can provide the support and guidance you need. Visit us today to start your journey toward a healthier life.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.















