If you’re facing heroin withdrawal, the first question on your mind is probably, “How long is this going to take?” Generally, the most intense part of the detox—the acute phase—lasts about five to ten days. Symptoms usually start cropping up within 6 to 12 hours after the last time someone uses.
This initial period is, without a doubt, the toughest stretch. But having a clear roadmap of what to expect day by day can make all the difference in preparing for the challenge ahead.
Understanding the Heroin Detox Timeline Day by Day
Going through heroin detox is a very real, very physical process. It’s your body recalibrating and learning how to work again without a substance it has come to depend on. While everyone’s journey is a bit different, the timeline tends to follow a recognizable pattern: symptoms appear, they hit a peak, and then they slowly start to fade.
Think of it like getting over a severe flu. You know the first couple of days will be rough, but you also know that relief is on the other side. This day-by-day breakdown is meant to be a guide through that process.
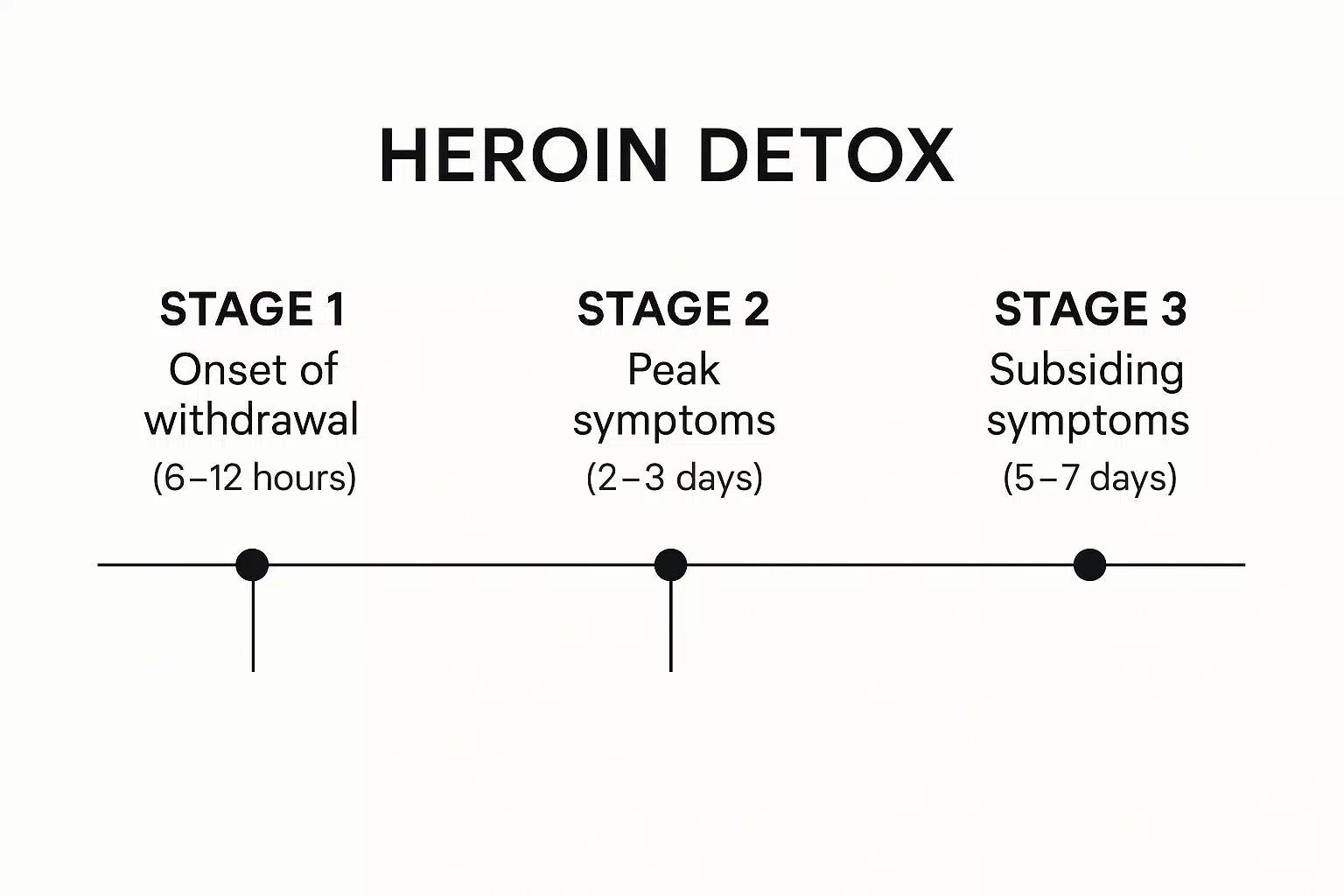
This visual breaks down the three main stages of the acute detox timeline, showing how symptoms start, peak, and then begin to recede.
As you can see, the most severe symptoms are typically packed into the first 72 hours before they start to ease up.
The First 24 Hours
The first signs of withdrawal kick in pretty quickly after the last dose. You’ll likely start feeling the effects within 6 to 12 hours, with things getting progressively more intense over the next two to three days.
Early on, it can feel a lot like you’re coming down with a bad flu. We’re talking muscle aches, a runny nose, feeling anxious, and powerful cravings for the drug. These feelings will build as more time passes.
Days 2 to 3: The Peak of Withdrawal
This is the hardest part. The second and third days are typically when withdrawal symptoms are at their absolute worst, and it can be an incredibly difficult and uncomfortable experience. The early flu-like symptoms will intensify, and new, more severe ones will likely appear.
“During the peak of heroin withdrawal, the body and mind are under immense stress. This is the point where having professional medical supervision is most crucial for managing symptoms safely and effectively.”
Common symptoms during this peak period include:
- Severe nausea, vomiting, and diarrhea
- Intense, deep pain in the muscles and bones
- Heavy sweating, uncontrollable chills, and goosebumps
- Extreme restlessness, agitation, and an inability to sleep
This is the height of the physical battle as your body works overtime to find its balance again. For a more detailed exploration of what to expect, check out this in-depth guide on heroin withdrawal symptoms and timelines.
Days 4 to 7: Symptoms Begin to Subside
After you get through the peak, things slowly start to get better. From about day four onward, the most intense physical symptoms begin to ease up. You’ll likely still feel exhausted and unwell, but the worst of it is usually in the rearview mirror.
The vomiting and diarrhea should lessen, making it possible to keep fluids and a little food down. Those deep muscle aches will start to fade, and you might finally be able to get some much-needed rest. While the physical side is improving, be prepared for emotional symptoms like depression and anxiety to stick around for a bit longer.
Heroin Acute Withdrawal Timeline at a Glance
To give you a clearer picture, here is a simple breakdown of what to expect during the acute phase of heroin withdrawal. This table summarizes the progression of symptoms and their general intensity.
| Timeframe | Common Symptoms | Intensity Level |
|---|---|---|
| 6-12 Hours | Muscle aches, anxiety, runny nose, sweating, yawning, cravings | Mild to Moderate |
| Days 2-3 (Peak) | Severe nausea, vomiting, diarrhea, intense muscle/bone pain, insomnia, chills | High / Severe |
| Days 4-7 | Lingering aches, fatigue, anxiety, depression, poor appetite | Moderate to Low |
This timeline provides a general framework, but remember that a medically supervised detox can help manage the severity of these symptoms, making the process much safer and more bearable.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Why Heroin Withdrawal Happens: A Look Inside the Brain
To really get a handle on the heroin detox timeline, it helps to understand what’s actually going on inside your brain. Withdrawal isn’t some kind of moral failing or a lack of willpower. It’s a completely predictable biological response—your brain trying to find its balance again after becoming dependent on an incredibly powerful drug.
Imagine your brain’s natural system for managing pain and pleasure is like a finely-tuned factory. This factory produces its own chemicals, mainly endorphins, which act as the body’s built-in painkillers and mood boosters. They keep everything running smoothly, helping you feel stable and content.
The Brain Factory Takeover
When you use heroin, it floods your brain with signals that are way more powerful than your natural endorphins. It’s like a massive outside corporation coming in, seizing control of your little factory, and cranking production up to an insane, unsustainable level.
Your brain, sensing this massive overload, does what any smart factory manager would do: it shuts down its own production lines. Why bother making its own stuff when there’s already an overwhelming supply coming in from an outside source? After a while, the brain becomes so reliant on heroin that its own factory goes completely dormant. It essentially forgets how to function on its own.
“Withdrawal is that chaotic, painful period when the external supply of heroin is suddenly cut off, but the brain’s own production factory is still offline. This chemical imbalance is what triggers the brutal physical and emotional symptoms.”
This sudden stop is why understanding how long it takes to detox from heroin is so critical. Your body is left scrambling to restart its own internal systems from a dead stop, and that process is never quick or painless.
Rebooting the System
When the heroin is gone, the brain is caught in a huge deficit. All those powerful opioids have vanished, but the internal factory isn’t ready to fire back up yet. This chemical vacuum is what creates the intense symptoms we call withdrawal.
- Pain Signals on Overdrive: Without any opioids—natural or otherwise—to manage pain, every little ache and cramp feels amplified. This is what causes the severe muscle and bone pain so common in withdrawal.
- Emotional Chaos: The brain’s pleasure and reward centers have gone dark. This leads to profound feelings of depression, crippling anxiety, and intense agitation.
- Physical Meltdown: Basic bodily functions, like regulating temperature and digestion, are thrown completely out of whack. This is where the chills, sweats, vomiting, and diarrhea come from.
This process really puts into perspective why detox is so incredibly difficult. The brain isn’t just “adjusting”; it’s going through a full-blown, difficult reboot. The time this takes can also depend on how long the drug remains in the body. You can learn more by exploring how long heroin stays in your system.
When you look at withdrawal through this biological lens, it helps reframe the whole experience. It’s not a character issue; it’s a neurological one. Your brain is healing, fighting, and re-learning how to work on its own again—and that’s a courageous first step toward getting your life back.
Factors That Shape Your Personal Detox Timeline
While the general day-by-day withdrawal timeline is a helpful map, it’s just that—a map. It’s not the actual territory. The question “how long does it take to detox from heroin?” has no single answer because no two people are exactly alike. Your journey is uniquely yours.
Think of it this way: two people might get the same flu bug, but one could be over it in three days while the other is laid up for a week. Their overall health, lifestyle, and unique physiology all come into play. It’s the exact same principle with heroin detox.
Understanding what shapes your personal timeline is key. It helps you set realistic expectations and shows why a cookie-cutter approach to recovery simply doesn’t work.
Your History with Heroin Use
The biggest factor by far is your history with the substance. This isn’t just one thing, but a combination of habits that determine just how physically dependent your body has become. The deeper the dependence, the longer and more intense the withdrawal will likely be.
Here’s what really moves the needle:
- How long you’ve been using: Someone who has used heroin for several years has given their brain a long time to adapt. Their detox will almost certainly be more complex and drawn-out than for someone who has used for only a few months.
- How much and how often: Using high doses multiple times a day creates a powerful physical dependence. When the drug is suddenly gone, the body experiences a much greater shock, triggering more severe symptoms.
- How you used it: The method of administration matters. Injecting heroin sends the drug straight to the brain almost instantly, which can build a more intense dependence much faster than smoking or snorting.
Your Overall Physical and Mental Health
Your general health at the start of detox is another massive piece of the puzzle. A healthy body is simply better equipped to handle the incredible stress of withdrawal. On the flip side, any underlying health problems can make the process tougher and potentially longer.
Co-occurring mental health conditions—like depression, anxiety, or PTSD—are also huge factors. The psychological side of withdrawal is already brutal, but if you’re already struggling with a mental health disorder, those symptoms can be magnified intensely. This emotional turmoil can make the physical pain feel even worse.
“It’s a vicious cycle. Withdrawal makes existing mental health symptoms flare up, and those amplified symptoms make the detox process feel almost unbearable. This is precisely why integrated care, with both medical and psychological support, is absolutely essential.”
Your Individual Biology and Support System
Finally, there are the factors that are just part of who you are. You can’t control them, but they still have a major impact on your experience.
- Genetics and Metabolism: Your unique genetic code influences how fast your body processes and clears substances. This can directly affect when withdrawal starts and how long it lasts.
- Your Environment: Having a stable, safe, and supportive place to detox makes a world of difference. Trying to get through this in a stressful or triggering environment adds a massive psychological weight and seriously increases the risk of relapse.
These variables are exactly why a one-size-fits-all detox plan is doomed to fail. A personalized program that takes your unique history and health into account is the safest and most effective way to start your recovery. It also shows why detox is only the beginning. To get a better sense of the full road ahead, it’s helpful to understand how long rehab programs typically last.
Beyond the First Week: Understanding Post-Acute Withdrawal

Getting through that first week of heroin detox is a massive accomplishment. The worst of the physical, flu-like misery has likely passed, and you might feel like you’ve finally crossed the finish line. And in many ways, you have. But the true answer to “how long does it take to detox from heroin?” goes far beyond that initial physical battle.
Now, the real work of healing the brain begins, and this phase comes with its own unique set of hurdles. This period is defined by a condition known as Post-Acute Withdrawal Syndrome, or PAWS.
Think of PAWS as the brain’s echo of withdrawal. The violent storm of acute physical symptoms is over, but the neurological aftershocks can linger for a while. This isn’t a sign of failure; it’s a completely normal part of your brain recalibrating and finding its footing after a long period of substance use.
What Is Post-Acute Withdrawal Syndrome?
PAWS is a cluster of symptoms, mostly psychological and emotional, that can stick around for weeks, months, or sometimes even longer after the acute phase is done. These symptoms often come and go in waves, which is why some days you might feel on top of the world, while others feel like an uphill battle.
Understanding what PAWS is can be a game-changer. It’s easy to feel disheartened when you’ve put in the hard work to get through the physical agony, only to find yourself wrestling with anxiety or sudden mood swings. Recognizing these feelings as a predictable part of the healing process is the first, most crucial step to managing them.
“Post-Acute Withdrawal Syndrome isn’t a setback; it’s a sign that your brain is actively working to restore its natural chemical balance. The symptoms are the growing pains of neurological recovery.”
This happens because even though the drug is out of your system, your brain chemistry is playing catch-up. Key neurotransmitter systems—the ones in charge of your mood, sleep, and stress levels—were suppressed for a long time. They simply need a while to reboot and start functioning properly on their own again.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Common Symptoms of Heroin PAWS
The symptoms of PAWS can be subtle, but their impact on daily life and recovery can be significant. They’re a far cry from the acute withdrawal symptoms and demand a totally different set of coping skills.
Some of the most common challenges people face during this phase include:
- Persistent Anxiety: A nagging sense of worry or unease that doesn’t seem to have a clear cause.
- Irritability and Mood Swings: Finding yourself shifting from angry to sad for no apparent reason.
- Chronic Fatigue and Low Energy: A deep sense of mental and physical exhaustion, even after a full night’s sleep.
- Difficulty Sleeping (Insomnia): Trouble falling or staying asleep, or having vivid, unsettling dreams.
- Cognitive Issues: Frustrating problems with concentration, memory, and simple decision-making, often called “brain fog.”
- Depression and Anhedonia: A lingering low mood and, most frustratingly, the inability to feel pleasure from things you used to love.
These symptoms can be incredibly trying and can sometimes trigger cravings. The brain has a long memory and recalls that using heroin offered a fast—though destructive—escape from these very feelings.
Navigating the Challenges of PAWS
The key to getting through PAWS is to know what you’re up against and to have a solid plan. This isn’t about just gritting your teeth and pushing through; it’s about building a robust support system and developing healthy, sustainable coping mechanisms. How long this phase lasts is different for everyone.
Here are a few strategies that make a real difference:
- Education: Just knowing that PAWS is a real, documented, and temporary part of recovery can bring immense relief. It helps you understand that what you’re feeling is normal, reducing the fear and self-blame that can creep in.
- Consistent Routine: Your brain thrives on predictability while it’s healing. Sticking to a regular schedule for sleeping, eating, and exercise provides a sense of stability when your emotions feel chaotic.
- Ongoing Support: This is where long-term recovery programs truly prove their worth. Regular therapy, support groups like NA, and staying connected with sober friends give you a vital outlet and serve as a constant reminder that you are not alone in this.
- Stress Management: Learning to manage stress without substances is crucial. Things like mindfulness, meditation, gentle exercise, or even just spending quiet time in nature can help soothe a nervous system that’s been in overdrive.
Learning to manage PAWS is one of the most important parts of preventing relapse. It’s about building a foundation for a fulfilling, sustainable life in recovery and understanding that detox is just the first step on a much longer, but incredibly rewarding, journey.
Why Medical Detox Is Your Safest Path Forward
Trying to quit heroin on your own might feel like the strong thing to do, but it’s a gamble you just don’t need to take. While the privacy of your own home seems comforting, the reality is that heroin withdrawal isn’t just a bad flu—it’s a serious medical event that really needs professional eyes on it. Going it alone is not just incredibly difficult; it can be outright dangerous.
The biggest issue is how severe the symptoms can get. While it’s true that heroin withdrawal itself is rarely fatal, the side effects absolutely can be. Think about it: constant vomiting and diarrhea can lead to severe dehydration and throw your body’s electrolyte levels into chaos, which can seriously impact your heart. There’s also a very real risk of aspirating on vomit, leading to dangerous lung infections like pneumonia.
The Shield of Professional Medical Care
A professional medical detox center is your shield against these dangers. It’s a safe, stable place where you’re never left to fend for yourself. That’s the key difference between trying to “tough it out” at home versus getting compassionate, expert care from people who know exactly what you’re going through.
In a medical setting, you get around-the-clock support designed just for you:
- 24/7 Monitoring: Nurses and doctors are always there, keeping an eye on your heart rate, blood pressure, and other vital signs. They can spot a problem long before it becomes an emergency.
- Symptom Management: They have medications that can take the edge off the worst of it—things to stop the nausea and vomiting, or non-addictive options like clonidine to help with the anxiety and shakes.
- Hydration and Nutrition: If you can’t keep food or water down, they can use IV fluids to prevent dehydration. This ensures your body has the strength it needs to get through this.
“A medically supervised detox isn’t about making withdrawal completely comfortable—that’s just not realistic. It’s about making it safe. It’s about minimizing the suffering so you can get through it without caving to the pain and cravings.”
A Foundation for Lasting Recovery
Beyond just getting you through the physical storm, medical detox tackles the intense psychological battle. The powerful cravings and emotional agony that hit during withdrawal are the main reasons people relapse. In fact, one of the biggest dangers of detoxing alone is the high risk of overdose. After a few days off heroin, your tolerance plummets. If you relapse and use your old dose, it can easily be fatal.
A professional facility puts a life-saving buffer between you and that risk. It gets you away from the people, places, and things that trigger your use and provides a steady stream of emotional support. This dramatically boosts your chances of making it through this crucial first step. As you move past the worst of it, understanding the role of detox in a full rehab program is what helps you build a life that lasts.
Choosing medical detox is really an act of self-care. It’s a way of saying you take this seriously and are giving yourself the best possible shot. It provides the safety, comfort, and expert help you need to get through this and start building a solid foundation for your future.
How Medication-Assisted Treatment Eases the Journey

Let’s be clear: getting through heroin withdrawal is a monumental task. Trying to do it without medical support is not just incredibly difficult, it’s often unsafe. This is where Medication-Assisted Treatment (MAT) comes in as one of the most powerful tools we have. It’s a strategy that uses specific, FDA-approved medications to make the entire detox process safer, more bearable, and far more likely to succeed.
Think of acute withdrawal as a raging wildfire. MAT acts like a specialized fire retardant—it doesn’t extinguish the blaze instantly, but it cools the flames enough to let you regain control. It lowers the intensity, preventing you from being overwhelmed and giving you the stability to start the real work of healing.
Turning Down the Volume on Withdrawal
The genius behind MAT is how it interacts with the brain. The medications used in this approach gently attach to the same opioid receptors that heroin latches onto, but they do it in a controlled, safe way that doesn’t produce a euphoric high. This simple action effectively turns down the volume on the most brutal withdrawal symptoms and cravings.
Instead of being hit with the full, agonizing force of withdrawal, your body is gradually guided toward a stable state. This creates invaluable breathing room, shifting your focus from just surviving the next few minutes to actually engaging with the recovery process.
“Medication-Assisted Treatment is not about substituting one addiction for another. It is a scientifically proven medical strategy that stabilizes brain chemistry, reduces illicit opioid use, and gives individuals a fighting chance to engage in meaningful, long-term recovery.”
With the physical chaos finally managed, you can start the crucial psychological work that true recovery requires. To get a more complete picture, it’s worth exploring what Medication-Assisted Treatment is and how it integrates into a comprehensive treatment plan.
Key Medications Used in Heroin Detox
Doctors have a few trusted medications they turn to when helping someone through heroin withdrawal. The right choice always depends on a person’s unique health history and specific situation.
- Buprenorphine (often in Suboxone): As a partial opioid agonist, buprenorphine is a go-to option. It binds to opioid receptors just enough to stop withdrawal and curb cravings but has a “ceiling effect”—meaning that after a certain point, taking more doesn’t increase its effects. This built-in safety feature significantly lowers the risk of misuse.
- Methadone: This is a long-acting full opioid agonist that has been a gold standard in opioid treatment for decades. Given in controlled, clinical doses, it effectively prevents withdrawal symptoms and keeps cravings at bay. It must be administered in a licensed clinic.
- Lofexidine and Clonidine: These are non-opioid medicines that are fantastic for tackling some of the most uncomfortable physical symptoms—like anxiety, sweating, muscle aches, and a racing heart. While they don’t stop the cravings, they can make the overall experience much more tolerable.
Building a Bridge to Long-Term Recovery
In the end, MAT is a bridge. It’s what gets you from the dangerous, unstable world of active addiction to a place where you’re healthy and clear-headed enough to build a new life. It’s not a magic bullet, but it’s a powerful foundation.
The research is undeniable: people who use MAT during and after detox have dramatically lower relapse rates. This approach treats opioid dependence for what it is—a medical condition—and uses a proven medical solution to address it. It’s a compassionate, evidence-based strategy that makes recovery not just possible, but sustainable.
Your Questions About Heroin Detox, Answered
Thinking about heroin detox brings up a lot of questions. It’s completely normal to feel uncertain, even after learning about the general timeline. Let’s tackle some of the most common and pressing concerns people have when they’re getting ready to face withdrawal.
My goal here is to give you straight, clear answers to help you feel more prepared and confident about the road ahead.
Is It Really That Dangerous to Detox from Heroin at Home?
I’m going to be direct here: detoxing from heroin at home is not a good idea. It’s actively discouraged by medical professionals because the risks are just too high. The withdrawal symptoms, especially the severe vomiting and diarrhea, can cause life-threatening dehydration and throw your body’s electrolytes dangerously out of balance, which can even impact your heart.
On top of the physical risks, the sheer intensity of the cravings and pain makes relapsing almost inevitable for most people. And this is the most dangerous part: after even a few days of not using, your tolerance plummets. If you relapse, the same dose you used to take could now be a fatal overdose.
“A medically supervised detox program isn’t just about comfort—it’s about safety. It provides a secure, controlled environment designed to manage these risks and give you the best possible chance of getting through withdrawal successfully.”
What’s the Fastest Way to Get Through Heroin Detox?
Everyone wants the process to be over as quickly as possible—that’s a completely natural feeling. But when it comes to heroin withdrawal, there are no safe shortcuts. You might hear about “rapid detox” or “ultra-rapid detox,” which often use anesthesia to get you through the worst of it while you’re unconscious. These methods come with serious medical risks and completely skip over the crucial psychological work needed to start building a real recovery.
The safest, most effective approach is a professionally managed detox that focuses on making you stable and comfortable. It allows your body the time it needs to heal properly. Think of it this way: you’re preparing for a marathon, not a sprint, and this is the essential first step.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
How Long Will I Feel Sick After I Stop Using Heroin?
The worst of it—that intense, flu-like physical sickness—usually peaks and then gets much better within about 7 to 10 days. Once you’re past that initial window, the most severe physical pain is typically behind you.
But the process isn’t completely over. It’s very common to experience something called Post-Acute Withdrawal Syndrome (PAWS). This is where you’ll have lingering psychological and emotional symptoms like mood swings, anxiety, fatigue, and trouble sleeping. These can stick around for weeks or even months, but they tend to come and go in waves, becoming less intense over time. This is a normal part of your brain chemistry rebalancing, and getting continued support through therapy and support groups is key to getting through it.
If you or someone you know is caught in the cycle of addiction, please know that help is available and you don’t have to do this alone. Addiction Helpline America is a free, confidential resource available 24/7 to connect you with the support you need to begin your recovery. You can take that crucial first step by reaching out at https://addictionhelplineamerica.com.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.















