Understanding Hospital Detox Alcohol: Your Essential Guide to Safe Withdrawal
Hospital detox alcohol is a medically supervised process where individuals with alcohol dependence safely withdraw from alcohol under 24/7 professional care in a hospital setting. This level of care is critical because alcohol withdrawal can be life-threatening, with complications like seizures and delirium tremens (DTs) occurring in 3-5% of patients.
Three main ways to access hospital detox for alcohol:
- Emergency Room Admission – For severe withdrawal symptoms like seizures, confusion, or hallucinations
- Direct Admission via Referral – Planned detox through your doctor or mental health professional
- Addiction Helpline/Treatment Center – Confidential assessment and placement assistance
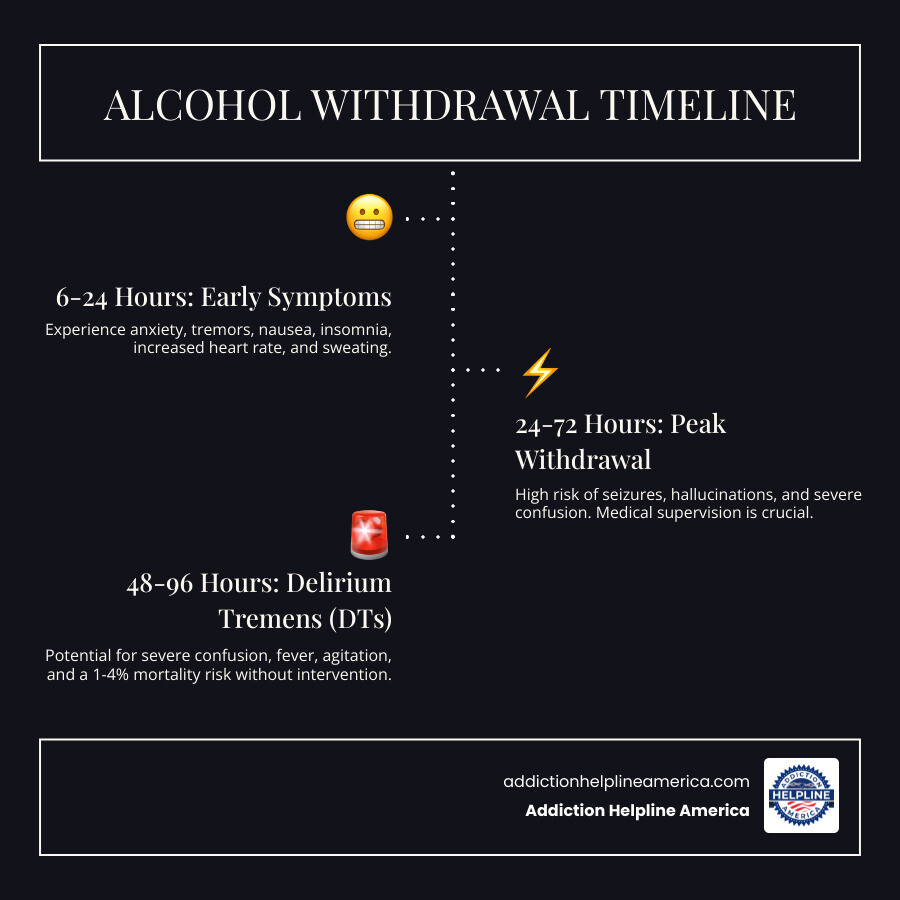
Why hospital detox matters: Alcohol withdrawal syndrome (AWS) can cause dangerous symptoms ranging from mild anxiety and tremors to potentially fatal complications. Symptoms typically begin 6-24 hours after the last drink and can last several days. Without proper medical management, severe withdrawal can lead to seizures, cardiac stress, dehydration, and delirium tremens—a condition with a mortality rate of 1-4% even with treatment.
Hospital-based detox provides constant medical monitoring, medication management (primarily benzodiazepines), nutritional support including thiamine to prevent Wernicke’s encephalopathy, and immediate intervention if complications arise. This supervised environment is exponentially safer than attempting detox at home, where medical emergencies cannot be quickly addressed.
At Addiction Helpline America, we’ve guided thousands of individuals and families through the hospital detox alcohol process, connecting them with appropriate medical facilities and providing ongoing support throughout their recovery journey. Our team understands the fear and uncertainty that comes with seeking help, and we’re here to make accessing safe, effective treatment as straightforward as possible.
Why Professional Detox Is a Medical Necessity
When someone who’s been drinking heavily for a long time suddenly stops, their body goes through a serious adjustment. The brain and body have become so used to alcohol that they actually depend on it to function. When it’s suddenly gone, the reaction can range from uncomfortable to downright dangerous. This is what doctors call Alcohol Withdrawal Syndrome (AWS), and it’s the main reason why hospital detox alcohol programs exist.
Here’s what makes AWS so unpredictable: it affects everyone differently. Some people might only deal with mild symptoms like anxiety, shaky hands, trouble sleeping, and nausea. For others, things get much more serious. Within the first day after stopping, symptoms can intensify to include racing heartbeat, high blood pressure, confusion, and heavy sweating.
The most dangerous complications typically show up between 48 and 96 hours after the last drink. This is when seizures, severe hallucinations, and Delirium Tremens (DTs) can occur. DTs is the most severe form of alcohol withdrawal, and it’s genuinely frightening. People experiencing DTs become profoundly confused, extremely agitated, and develop a high fever and rapid heartbeat. The statistics tell an important story: about 3-5% of people going through alcohol withdrawal will develop DTs, and even with medical treatment, it can be fatal in 1-4% of cases.
Beyond the neurological symptoms, alcohol withdrawal puts serious strain on your entire body. Seizures can happen without warning and cause injury or worse. The heart can develop dangerous irregular rhythms that require immediate intervention. Severe dehydration compounds every other symptom and creates its own risks. If you have existing health conditions, withdrawal can make them worse or trigger new medical emergencies.
This is exactly why trying to detox at home is so dangerous. You simply can’t predict how your body will respond, and if a medical emergency happens, every minute counts.
The difference between home detox and hospital detox alcohol care is honestly night and day. In a hospital setting, you have medical professionals watching you around the clock. They’re checking your vital signs, monitoring for complications, and ready to intervene immediately if something goes wrong. They can give you medications to prevent seizures, ease your discomfort, and keep your heart rhythm stable. Your safety is the top priority every single moment.
The American Society of Addiction Medicine makes this clear in their Clinical Guidelines for Alcohol Withdrawal: medical management during withdrawal isn’t optional for many people—it’s essential for survival.
At Addiction Helpline America, we’ve walked alongside thousands of people through this process. We understand that thinking about detox can feel overwhelming or even scary. But here’s what we want you to know: detox is a healing process, not a punishment. Yes, it’s challenging. But with proper medical support, it’s safe, and it’s the doorway to a life you might have thought was impossible.
The long-term rewards of sobriety are worth every difficult moment of withdrawal. You deserve to get through this safely, with compassionate care supporting you every step of the way. To learn more about what the entire journey looks like, take a look at our comprehensive guide on the detoxification process.
How to Access a Hospital Detox for Alcohol: 3 Key Pathways
When you’re ready to take the step toward recovery, knowing how to actually get into a hospital detox alcohol program can make all the difference. The process doesn’t have to be complicated or mysterious. There are three main pathways, and the right one for you depends on your current situation and how urgent your need is.
Method 1: Emergency Room (ER) Admission
Sometimes withdrawal doesn’t wait for a scheduled appointment. When symptoms become severe or frightening, the emergency room is exactly where you need to be. There’s no shame in this—it’s what emergency rooms are designed for.
You should head to the ER immediately if you or someone you care about experiences any of these warning signs: seizures or convulsions, severe confusion where you can’t recognize where you are or who people are, hallucinations (seeing or hearing things that aren’t real), chest pain or heart palpitations, vomiting blood or dark material that looks like coffee grounds, extremely rapid heartbeat, difficulty breathing, or thoughts of hurting yourself or others.
The ER team knows what to do. They’ll assess how severe your withdrawal is using standardized tools and immediately address any life-threatening symptoms. Their job is to stabilize you first—making sure your heart, breathing, and brain function are safe. Once you’re medically stable, they’ll arrange for you to transfer to an inpatient medical detoxification unit, either within that same hospital or at another facility equipped to provide the ongoing care you need. You won’t be left to figure out the next steps alone.
Method 2: Direct Admission via a Referral
If you’re not in immediate crisis but know you need help, planning your admission through a healthcare provider can give you time to prepare mentally and logistically. This is often the path people take when they’ve made the decision to get sober and want to do it safely.
Start by talking to your primary care physician or a mental health professional you trust. They can evaluate your drinking history, overall health, and any other conditions you might be dealing with. A thorough Alcohol and Drug Evaluation helps determine exactly what level of care will serve you best.
Once your doctor makes a referral for hospital detox alcohol, the hospital’s admissions team takes over. They’ll verify your insurance coverage, answer questions about what to expect, and schedule your admission date. This gives you time to arrange work leave, notify family members, pack what you’ll need, and mentally prepare for this important step. Having a scheduled admission also means the facility will have a bed ready and your care team prepared for your arrival.
Method 3: Using an Addiction Helpline or Treatment Center
Perhaps the most supportive way to access hospital detox alcohol is by calling a dedicated addiction helpline like ours at Addiction Helpline America. We exist specifically to make this process easier for you.
When you call us, you’ll speak with a compassionate recovery advocate who understands what you’re going through. We’ll conduct a confidential assessment to understand your situation—your drinking history, any medical concerns, whether you have insurance, and what matters most to you in treatment. There’s no judgment here, just someone who wants to help you find the right care.
Based on what we learn, we’ll match you with a suitable hospital or medical detox facility from our network across the country. We work with quality facilities in states from Florida to Ohio to Arizona and beyond. Then we handle the complicated parts: verifying insurance pre-authorization, coordinating with the facility’s admissions team, and arranging your admission. If you need immediate placement because your situation is urgent, we can often make that happen quickly.
We know that making the call is hard enough. You shouldn’t also have to steer insurance bureaucracy or worry about logistics. That’s what we’re here for. After detox, if you’re considering what comes next, our information on inpatient rehab programs can help you understand your options for continued treatment and long-term recovery support.
What to Expect During Your Hospital Detox Alcohol Stay
Taking the step to enter a hospital detox alcohol program is one of the most courageous decisions you’ll ever make. We know it can feel intimidating to walk through those doors, not knowing exactly what lies ahead. That’s why we want to walk you through what typically happens during your stay, so you can focus on healing rather than worrying about the unknown.
The Admission and Assessment Process
When you first arrive, you’ll be greeted by caring staff members who understand what you’re going through. They’ve helped countless people just like you, and their goal is to make you feel safe and supported from the very first moment.
The admission process starts with gathering important information about you. You’ll want to bring any medications you’re currently taking, your insurance card, a photo ID, and comfortable clothing for your stay. Leave valuables at home if possible, as hospital detox units typically have limited storage for personal items.
Your medical team will sit down with you for a comprehensive medical history review. They’ll ask about your overall health, any chronic conditions like diabetes or heart disease, and what medications you take regularly. This isn’t about judgment—it’s about keeping you safe. The more honest you can be, the better they can care for you.
Next comes a detailed substance use evaluation. The staff will ask about your drinking patterns—how much you typically drink, how long you’ve been drinking heavily, and whether you’ve tried to stop before. If you’ve experienced withdrawal symptoms in the past, they’ll want to know about those too. Again, complete honesty here is crucial for your safety.
You’ll also go through a psychological screening to check for co-occurring mental health conditions like depression or anxiety. Many people with alcohol dependence struggle with these conditions, and identifying them early helps your treatment team provide better care.
Throughout your stay, the medical team will use something called the Clinical Institute Withdrawal Assessment for Alcohol, or CIWA-Ar scale. This standardized tool measures ten different withdrawal symptoms, from anxiety and tremors to confusion and hallucinations. Your nurse will check in regularly and ask you questions to score your symptoms. This score helps determine exactly what medications you need and when you need them. You can read more about the Clinical Institute Withdrawal Assessment to understand how it guides your personalized treatment.
Medical Management During Hospital Detox Alcohol
The heart of hospital detox alcohol is round-the-clock medical care. Your vital signs—heart rate, blood pressure, temperature, and breathing—will be monitored constantly. A nurse will check on you frequently, and in many facilities, you’ll be connected to monitors that alert staff immediately if anything changes. This 24/7 monitoring is what makes hospital detox so much safer than trying to detox at home.
Medication management is central to your comfort and safety during withdrawal. Benzodiazepines are the gold standard for treating alcohol withdrawal. You’ll most likely receive either Diazepam (known by the brand name Valium) or Lorazepam (Ativan). These medications work by calming your overactive nervous system, which has been thrown into chaos by the sudden absence of alcohol.
The purpose of these medications goes beyond just making you more comfortable, though that’s certainly important. Benzodiazepines actively prevent seizures, which are one of the most dangerous complications of alcohol withdrawal. They also reduce anxiety, stop tremors, and help you rest—all crucial for healing.
Many hospitals now use what’s called symptom-triggered therapy. Instead of giving you medication on a fixed schedule, your nurses use your CIWA-Ar scores to determine when you need medication. If your symptoms are mild, you might not need much medication at all. If they’re more severe, you’ll receive what you need to stay safe and comfortable. This personalized approach means you get exactly the right amount of medication for your body.
Nutritional support is another critical piece of the puzzle. Years of heavy drinking often leave people severely deficient in essential vitamins, particularly thiamine (vitamin B1). Without enough thiamine, you’re at risk for Wernicke’s encephalopathy, a serious condition that causes confusion, vision problems, and difficulty with muscle coordination. To prevent this, you’ll receive thiamine supplementation, often through an IV at first, then by mouth.
You’ll also receive other supportive medications as needed. Anti-nausea drugs help if you’re vomiting. Pain relievers address headaches and body aches. Sleep aids can help you rest when anxiety keeps you awake. The medical team will also ensure you’re staying hydrated, as dehydration is common during withdrawal.
For a more detailed look at the medications used in alcohol withdrawal treatment, the National Institute on Alcohol Abuse and Alcoholism offers excellent information on medications for alcohol withdrawal.
Addressing Co-Occurring Mental Health Conditions
Here’s something important that many people don’t realize: alcohol dependence rarely exists alone. Depression, anxiety disorders, PTSD, and other mental health conditions frequently co-occur with alcohol use disorder. In fact, it’s so common that we have a specific term for it—dual diagnosis.
The good news is that a quality hospital detox alcohol program recognizes this connection. During your admission, you’ll undergo a psychiatric evaluation to identify any underlying mental health issues. This isn’t a separate process that happens later—it’s integrated into your care from day one.
Your treatment team typically includes psychiatrists, therapists, and counselors who specialize in both addiction and mental health. Even during the detox phase, you may begin initial counseling sessions. These conversations help you start processing the emotional aspects of your addiction and give you tools to cope with difficult feelings without turning to alcohol.
Managing anxiety and depression during detox isn’t just about feeling better in the moment—it’s about setting yourself up for long-term success. When mental health conditions go untreated, they become major triggers for relapse. By addressing them early, you’re building a stronger foundation for recovery.
This integrated approach treats you as a whole person, not just a collection of symptoms. Your physical withdrawal needs attention, yes, but so do your emotional wounds and mental health struggles. Both matter equally, and both receive care in a comprehensive hospital detox program.
If you’re interested in learning more about facilities that excel at treating both addiction and mental health conditions simultaneously, resources like dual diagnosis treatment centers can provide additional information about what integrated care looks like beyond the detox phase.
At Addiction Helpline America, we understand that the journey through detox is challenging, but you don’t have to face it alone. Every person on your treatment team is there because they believe in recovery and want to see you succeed. This is your time to heal, and you deserve compassionate, comprehensive care every step of the way.
Frequently Asked Questions about Hospital Alcohol Detox
We understand that considering hospital detox alcohol brings up many questions—and probably some anxiety too. You’re not alone in wondering what to expect. Here are the questions we hear most often, answered with the clarity and honesty you deserve.
How long does hospital alcohol detox typically last?
Most people spend between 2 to 7 days in a hospital detox program for alcohol. That’s the typical range, but your personal timeline might be different—and that’s completely okay.
Several factors influence how long you’ll need medical supervision. The severity of your alcohol dependence plays a significant role. If you’ve been drinking heavily for years, your body will likely need more time to adjust than someone with a shorter history of use. Your individual response to treatment matters too—some people’s bodies stabilize quickly, while others need a bit more time and support.
Co-occurring medical or mental health conditions can extend your stay as well. If you’re managing diabetes, heart issues, depression, or anxiety alongside alcohol withdrawal, the medical team will want to ensure everything is properly addressed before you transition to the next phase of recovery. Previous withdrawal episodes, especially if you’ve experienced seizures or Delirium Tremens before, may also indicate a need for a longer, more cautious detox period.
The bottom line is this: you’ll stay as long as you need to be medically safe and stable. Our priority is your wellbeing, not rushing you through a process that requires careful attention.
What medications are used to manage alcohol withdrawal?
Benzodiazepines are the first-line treatment for alcohol withdrawal, and for good reason. These medications—including Diazepam (Valium), Lorazepam (Ativan), and Chlordiazepoxide (Librium)—are highly effective at calming your overactive nervous system during withdrawal. When you stop drinking after prolonged use, your brain goes into overdrive. Benzodiazepines help restore balance, preventing the most dangerous complications like seizures and reducing uncomfortable symptoms like anxiety, tremors, and agitation.
The medical team carefully tailors your medication dosage based on your symptoms. They use assessment tools like the CIWA-Ar scale to determine exactly how much medication you need and when you need it. This symptom-triggered approach means you’re never over-medicated or under-supported.
Beyond benzodiazepines, you’ll receive other supportive medications to address the full spectrum of withdrawal effects. Thiamine (Vitamin B1) is absolutely critical—it prevents Wernicke’s encephalopathy, a serious neurological condition that can develop in people with chronic alcohol use. You’ll likely receive this intravenously at first, along with folic acid and multivitamins to address other nutritional deficiencies.
Anti-nausea medications help with stomach distress. Blood pressure medications may be needed if your blood pressure spikes during withdrawal. Once the acute phase passes, sleep aids can help restore healthy sleep patterns. Every medication serves a specific purpose in making your detox as safe and comfortable as possible. For more detailed information about these medications, the National Institute on Alcohol Abuse and Alcoholism offers comprehensive research on medications for alcohol withdrawal.
Is hospital detox for alcohol covered by insurance?
Yes, hospital detox alcohol is often covered by insurance because it’s recognized as a medically necessary treatment. That said, coverage varies depending on your specific plan, so understanding your benefits is important.
Insurance companies typically require proof of medical necessity—meaning there’s a clinical determination that you cannot safely detox outside a hospital setting due to the risk of severe withdrawal complications. For most people entering hospital detox alcohol, this threshold is easily met given the potential dangers of alcohol withdrawal.
If you have Medicare or Medicaid, coverage guidelines are generally well-defined. Medicare covers inpatient hospital stays for alcohol detoxification when medical complications are likely and require constant physician availability or specialized medical equipment. Medicaid coverage varies by state but typically includes detoxification services as part of substance use disorder treatment benefits.
Private insurance plans, especially those under the Affordable Care Act, are required to cover mental health and substance use disorder services, including detoxification. However, your specific coverage will depend on factors like your deductible, co-pays, and whether the facility is in your insurance network.
This is where we come in. At Addiction Helpline America, we work directly with your insurance provider to verify your benefits, determine any out-of-pocket costs, and handle the pre-authorization process. We want you to know exactly what to expect financially before you begin treatment—no surprises, no confusion. Even if there are some out-of-pocket expenses, we’ll help you understand your options and find a solution that works for your situation.
The cost of treatment should never be a barrier to getting the help you need. Let us handle the insurance logistics so you can focus on what matters: your recovery.
Conclusion
Taking the first step toward recovery from alcohol dependence requires courage, and we’re here to tell you that choosing hospital detox alcohol is one of the safest, most compassionate decisions you can make for yourself or a loved one. Throughout this guide, we’ve walked through why professional medical supervision isn’t just helpful—it’s genuinely life-saving. The risks of alcohol withdrawal, from seizures to Delirium Tremens, are real and serious, but they’re also manageable when you have the right medical team by your side.
We’ve shown you three clear pathways to access care: rushing to the emergency room when symptoms become severe, planning a structured admission through your doctor’s referral, or reaching out to a dedicated helpline like ours that can guide you through every detail. Each route leads to the same destination—a safe, supervised environment where medical professionals monitor you around the clock, administer medications like benzodiazepines to ease your symptoms, and address any mental health concerns that may be intertwined with your addiction.
But here’s something important to understand: detox is just the beginning. Think of it as clearing the fog so you can finally see the road ahead. Your body will stabilize, the immediate danger will pass, and you’ll start feeling physically better. But lasting recovery—the kind that transforms your life—requires continuing the journey beyond those first few days.
At Addiction Helpline America, we don’t just help you find the right hospital detox alcohol program and then disappear. We’re committed to walking alongside you through every phase of recovery. Once you’ve completed detox, the next crucial step is transitioning into a comprehensive treatment program that addresses the deeper roots of addiction and gives you the tools to build a fulfilling, sober life. We encourage you to explore types of treatment programs to find what comes next—whether that’s inpatient rehabilitation, outpatient therapy, or specialized dual diagnosis care.
Your journey toward healing starts with a single phone call. We’re here, ready to listen without judgment, to answer your questions, and to connect you with the care you deserve. Recovery is possible, and you don’t have to figure it out alone. Let’s take this first step together.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.