Understanding the Complexity of Severe Depression
Extreme depression treatment involves a comprehensive approach when standard therapies fail. Here’s what you need to know:
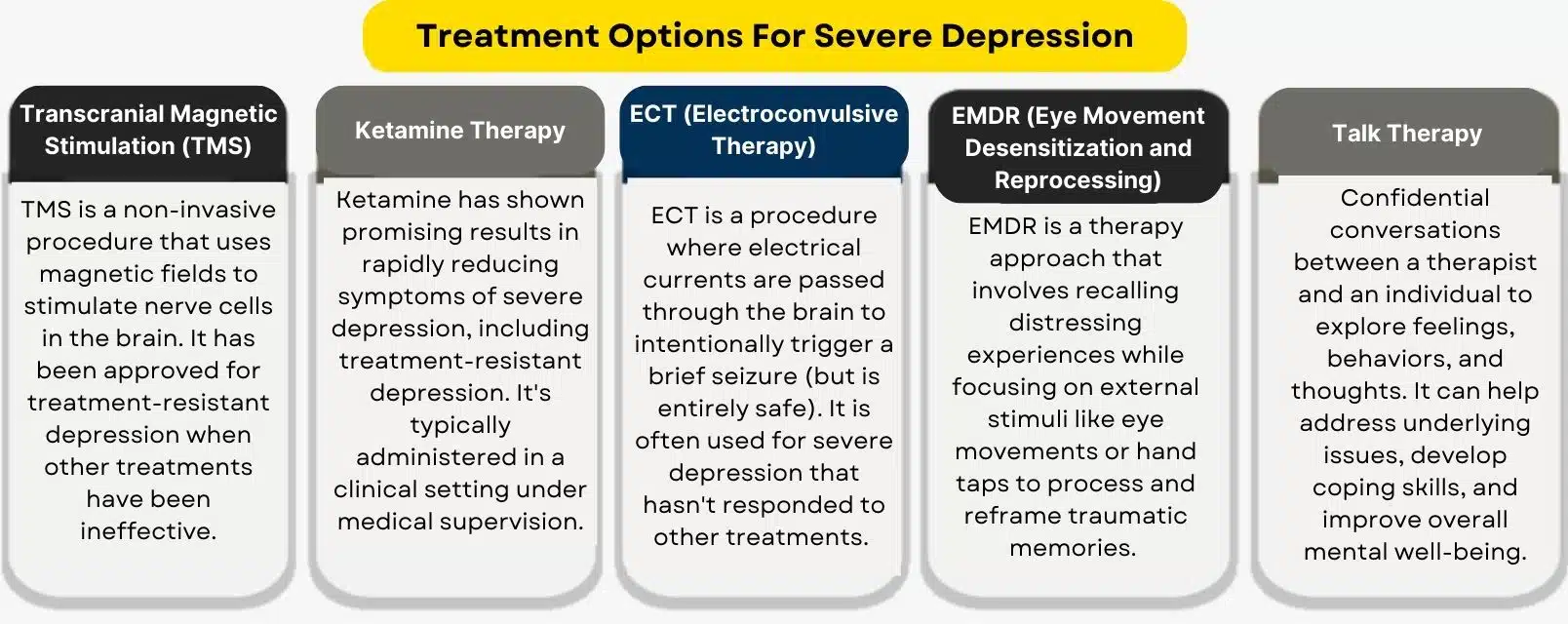
Core Treatment Options for Severe Depression:
- Advanced Medications: Switching antidepressants, augmentation with lithium or antipsychotics, pharmacogenetic testing
- Specialized Psychotherapy: CBT, IPT, DBT, and behavioral activation custom for severe cases
- Brain Stimulation: Electroconvulsive Therapy (ECT), Transcranial Magnetic Stimulation (rTMS), Vagus Nerve Stimulation (VNS)
- Rapid-Acting Treatments: Ketamine and esketamine therapy for immediate symptom relief
- Emerging Options: Psychedelic-assisted therapies currently in research trials
While many people respond to standard treatments, at least one-third of individuals with major depression experience treatment-resistant depression (TRD), where symptoms persist after trying two or more therapies.
TRD isn’t a dead end; it’s a signal that a different approach is needed. Medical science offers advanced interventions ranging from optimized medications and intensive therapy to innovative brain stimulation and emerging treatments that work through novel biological pathways.
The journey can feel hopeless, but approximately 80-90% of people with depression who seek treatment eventually respond well. Recovery often involves a combination of medication, therapy, lifestyle changes, and advanced procedures custom to your unique situation.
At Addiction Helpline America, we guide individuals and families through the process of finding effective extreme depression treatment, including for those with co-occurring substance use disorders. We connect you with specialized resources and programs to help you steer advanced treatment options and find what works for you.

Common extreme depression treatment vocab:
Understanding Extreme and Treatment-Resistant Depression
When standard treatments fail, understanding what’s happening is the first step toward finding relief.
Defining Treatment-Resistant Depression (TRD)
Treatment-Resistant Depression (TRD) is the medical term for major depression that hasn’t responded to standard treatments. A doctor may diagnose TRD if you’ve tried two or more different antidepressants (or therapies) for at least six weeks each at an adequate dose, without significant improvement. This doesn’t mean you’re untreatable; it simply means your brain requires a different strategy.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Persistent Symptoms
The hallmark of TRD is that symptoms won’t let go. You might experience:
- A persistent sad, anxious, or empty mood.
- Loss of pleasure in activities you once enjoyed (anhedonia).
- Significant changes in appetite or weight.
- Sleep disturbances, such as insomnia or oversleeping.
- Profound fatigue and low energy.
- Difficulty concentrating, remembering, or making decisions.
- Intense feelings of worthlessness or guilt.
- Unexplained physical aches, pains, or digestive problems.
- Thoughts of death or suicide. If you are having these thoughts, please seek immediate help by contacting a crisis line or calling Addiction Helpline America.
When five or more of these symptoms persist for at least two weeks and interfere with daily life, a professional evaluation for extreme depression treatment is essential.
Factors Contributing to TRD
TRD is not your fault. It’s a complex issue with several potential contributing factors:
- Misdiagnosis: Sometimes, what appears to be depression is actually another condition, like bipolar disorder, which requires different treatment. Antidepressants alone can worsen bipolar disorder.
- Co-occurring Conditions: Depression often exists alongside other issues that complicate recovery.
- Substance Use Disorders: Alcohol and drugs can deepen depression and interfere with medication. A dual diagnosis approach that addresses both issues simultaneously is crucial. Addiction Helpline America specializes in connecting people with these programs.
- Anxiety Disorders: Anxiety and depression often amplify each other, making standard treatments less effective.
- Chronic Medical Conditions: Illnesses like hypothyroidism, heart disease, and cancer are strongly linked to depression. As the Cleveland Clinic explains, treating the underlying medical condition is a key part of mental health recovery.
Importance of a Comprehensive Diagnosis
Given these complexities, a thorough evaluation is critical before starting extreme depression treatment. A specialist will conduct a detailed mental health assessment, review your medical history, and may order lab tests to rule out physical causes. Getting the right diagnosis is the first step toward finding a treatment that will lead to real recovery.
Advanced Medication and Psychotherapy Strategies

When first-line treatments don’t work, it’s time to explore more advanced strategies. Finding the right extreme depression treatment often requires a creative and persistent approach, combining different medications or therapies into a personalized plan.
Medication Strategies for Extreme Depression Treatment
Medication management for severe depression is a careful process, as it can take 4-8 weeks to feel the full effect of a new drug. Common strategies include:
- Switching Antidepressants: If one medication doesn’t work, your doctor may try another from the same or a different class.
- Augmentation: This involves adding a second medication to boost your antidepressant’s effectiveness. Common options include lithium (a mood stabilizer) or low-dose atypical antipsychotics (like aripiprazole).
- Combining Antidepressants: Using two different antidepressants together can target multiple neurotransmitter systems.
- Pharmacogenetic Testing: This genetic test can help predict your response to certain medications and potential side effects, reducing some of the guesswork.
- Dosage Optimization: Your doctor will start with a low dose and gradually increase it to find the most effective amount with the fewest side effects. Never stop antidepressants abruptly, as this can cause withdrawal or a relapse.
Different classes of antidepressants include:
- SSRIs: Often a first-line choice, generally well-tolerated.
- SNRIs: Boost both serotonin and norepinephrine, helpful for co-occurring chronic pain.
- Atypical Antidepressants: Each has a unique profile; some are energizing while others aid sleep.
- Tricyclic Antidepressants (TCAs): Older, effective drugs with more significant side effects, often reserved for severe cases.
- MAOIs: Powerful but require strict dietary restrictions; usually a last resort.
The American Academy of Family Physicians provides comprehensive guidance on these medication options.
Psychotherapy for Extreme Depression Treatment
For extreme depression treatment, combining medication with specialized therapy often yields the best results. Key approaches include:
- Cognitive Behavioral Therapy (CBT): Helps you identify and change the negative thought patterns and behaviors that fuel depression.
- Interpersonal Psychotherapy (IPT): Focuses on improving relationships and social connections that impact your mood.
- Dialectical Behavior Therapy (DBT): Teaches skills for mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness. It is especially helpful for severe emotional dysregulation and suicidal thoughts.
- Behavioral Activation (BA): Breaks the cycle of withdrawal by gradually increasing engagement in positive, meaningful activities.
- Psychodynamic Therapy: Explores how past experiences and unconscious conflicts influence your current feelings.
- Supportive Therapy: Provides empathy, encouragement, and a safe space to express feelings without judgment.
The American Psychological Association outlines evidence-based psychotherapies proven effective for depression. Finding the right therapist is crucial, so don’t be afraid to seek a different one if the fit isn’t right.
At Addiction Helpline America, we help people find specialized programs offering comprehensive extreme depression treatment, including for those with co-occurring substance use issues. You don’t have to figure this out alone.
Innovative Procedures for Extreme Depression Treatment

When medication and therapy aren’t enough, innovative procedures that work directly on the brain can offer new hope. These scientifically-backed interventions are an important part of the toolbox for extreme depression treatment.
Electroconvulsive Therapy (ECT)
Modern ECT is one of the safest and most effective treatments for severe depression, especially when suicide risk is high. While you are under general anesthesia, doctors pass small, controlled electrical currents through the brain to induce a brief seizure. This process changes brain chemistry and can rapidly reverse severe depressive symptoms. The most common side effect is temporary memory loss around the time of treatment, which has been significantly reduced with modern techniques.
Repetitive Transcranial Magnetic Stimulation (rTMS)
rTMS is a non-invasive procedure that uses magnetic pulses to stimulate underactive mood-regulating areas of the brain. During treatment, you are awake and can resume normal activities immediately afterward. A typical course involves daily 30-40 minute sessions for several weeks. Side effects are minimal, usually limited to mild scalp discomfort, and there is no memory loss. For more on brain stimulation, Rethink Mental Health offers valuable resources.
Ketamine and Esketamine Therapy
Ketamine is a rapid-acting treatment that works differently from traditional antidepressants, offering relief in hours or days. It is administered as an IV infusion (ketamine) or an FDA-approved nasal spray (esketamine/Spravato). Both must be given in a certified healthcare setting to monitor for potential risks like dissociation (feeling detached from reality) and temporary increases in blood pressure. This breakthrough is especially valuable for people with acute symptoms and suicidal thoughts.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Vagus Nerve Stimulation (VNS)
VNS is a long-term option for chronic, treatment-resistant depression. A small, pacemaker-like device is surgically implanted in the chest and sends regular, mild electrical impulses to the brain via the vagus nerve. It is considered after other treatments have failed, and its benefits develop gradually over several months. Risks include those associated with surgery and potential side effects like voice changes or coughing.
Emerging and Psychedelic-Assisted Therapies

The future of depression treatment includes groundbreaking research into psychedelic-assisted therapies. Psilocybin (from mushrooms) and MDMA, when combined with psychotherapy in clinical trials, appear to promote neuroplasticity and help people process trauma. Ibogaine is also being studied for its potential to treat both depression and addiction. While not yet widely available, these treatments represent significant hope. You can explore Mayo Clinic’s clinical trials database for ongoing research.
Addiction Helpline America stays current on all evolving treatment options. We can help you steer these innovative procedures and connect you with the specialized resources that match your needs.
Complementary and Lifestyle Approaches to Support Recovery
Powerful recovery plans for extreme depression treatment integrate professional care with daily choices that support healing. While advanced treatments provide the foundation, lifestyle approaches are essential for long-term well-being.
- Regular Exercise: Physical activity is a natural mood booster. Even a 10-minute walk releases endorphins. Start small and build consistency. The goal is to show up for yourself and get moving.
- Balanced Diet: Your brain needs proper fuel. A diet rich in whole foods, lean proteins, and complex carbohydrates can support your mental health and overall recovery.
- Sleep Hygiene: Depression and sleep are deeply connected. Break the negative cycle by setting a consistent sleep schedule, creating a dark and cool environment, and avoiding screens before bed.
- Stress Management: Tools like mindfulness meditation, yoga, and deep breathing exercises are evidence-based ways to regulate emotions and reduce the negative thought spirals that feed depression.
- Avoid Alcohol and Drugs: Substances may offer temporary relief but ultimately worsen depression and interfere with medication. If you’re struggling with substance use, addressing it is essential for recovery.
- Build a Support System: Social connection is healing. Lean on trusted family, friends, or a support group for emotional strength and to know you’re not alone.
Communicating with Your Healthcare Team
Your relationship with your providers is a partnership. You are the expert on your own experience.
- Advocate for Yourself: Be honest about your symptoms, side effects, and what isn’t working. Your doctor can’t help with what they don’t know.
- Prepare for Appointments: Write down your symptoms, questions, and a list of all medications and supplements you’re taking. Consider bringing a trusted friend or family member for support.
- Ask Questions: Inquire about the risks and benefits of a treatment, how long it might take to work, and what alternatives exist. Good care involves shared decision-making.
- Track Your Symptoms: Use a journal or app to note patterns in your mood. This data is invaluable for fine-tuning your treatment plan.
- Find a Specialist: If your symptoms persist, ask your primary care doctor for a referral to a psychiatrist or mental health specialist with expertise in complex cases.
At Addiction Helpline America, we understand that navigating extreme depression treatment is overwhelming, especially with co-occurring conditions. We’re here to help you find specialized programs and providers that address all aspects of your health.
Frequently Asked Questions about Extreme Depression Treatment
Navigating extreme depression treatment brings up many questions and concerns. Here are answers to some of the most common ones.
How do I know if I have treatment-resistant depression?
Treatment-resistant depression (TRD) is medically defined as major depression that has not significantly improved after adequate trials of at least two different antidepressant medications. However, only a qualified mental health professional can make this diagnosis. A specialist will conduct a comprehensive evaluation to confirm your diagnosis, rule out other conditions (like bipolar disorder or a medical issue), and assess for factors like co-occurring substance use that might be interfering with your recovery.
Are advanced treatments like ECT and Ketamine safe?
Yes, when administered by qualified professionals in appropriate medical settings, these treatments are considered safe and effective. Modern ECT is performed under general anesthesia and is a highly controlled procedure; its main risk is temporary memory loss, which has been greatly reduced with current techniques. Ketamine and esketamine are administered in supervised clinical environments to manage potential side effects like dissociation or temporary blood pressure changes. For many people with severe depression, the significant benefits of these treatments outweigh the manageable risks.
How long does it take to find an effective treatment?
This is one of the most frustrating parts of treatment, as the timeline varies for everyone. It is often a process of careful trial and observation. Traditional antidepressants can take 4 to 8 weeks to show their full effect. Brain stimulation therapies like rTMS involve daily sessions over several weeks. In contrast, ketamine can offer rapid relief within hours or days, though it typically requires ongoing sessions as part of a larger plan. The process requires patience and persistence. The good news is that the vast majority of people with TRD do eventually find an effective treatment plan, which often involves a combination of different approaches.
At Addiction Helpline America, we understand how isolating this process can feel, especially when complicated by substance use. Our team specializes in connecting people to treatment programs designed for complex, treatment-resistant cases. We’re here to help you steer your options and find the relief you deserve.
Conclusion
If you are looking for answers about extreme depression treatment, we want you to hold onto this: hope is real, and recovery is possible.
Even when you feel you’ve exhausted every option, there are still pathways to healing. Recovery from severe or treatment-resistant depression is rarely a single solution. It is a multi-faceted approach that may combine medication, therapy, lifestyle changes, and innovative procedures. Finding the right combination takes persistence, but it is achievable.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
At Addiction Helpline America, we understand this challenging process, especially when co-occurring conditions like substance use disorders are involved. We provide free, confidential, and personalized guidance to connect people across the nation with specialized treatment programs designed for severe and treatment-resistant cases.
We are here to listen, understand your needs, and connect you with options that make sense for your life. You do not have to figure this out alone or continue to suffer in silence. Your story doesn’t end with depression. Let us help you write the next chapter toward healing and peace.
Find professional help for depression and co-occurring disorders
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.















