
When you stop using a substance your body has become dependent on, it has to learn how to function without it again. The physical and psychological reactions that happen during this readjustment period are known as drug withdrawal symptoms.
These symptoms can show up within hours or days of your last dose, ranging from just mildly uncomfortable to severe and even life-threatening.
What Happens During Drug Withdrawal
Think of it like this: your brain and body got used to having a certain substance around all the time. It was like a constant helper managing everything from your mood to your energy levels. When that substance is suddenly gone, your system is thrown into chaos, scrambling to find its natural balance.
This intense recalibration is what we call withdrawal. It’s driven by two types of dependence that build up over time, and understanding them is key to knowing what to expect.
Physical vs. Psychological Dependence
Physical dependence is when your body has physically adapted to the presence of a drug and feels like it needs it to function normally. When you stop, your body protests with very real, tangible symptoms like shaking, sweating, nausea, and muscle aches.
Psychological dependence, on the other hand, is all about the mind. It’s that powerful, overwhelming feeling that you need the drug to cope, handle stress, or even just feel okay. This side of dependence fuels symptoms like intense cravings, anxiety, and irritability, which can often be the hardest part to overcome.
“Withdrawal isn’t a sign of weakness—it’s the body’s powerful, biological signal that it’s starting to heal. It’s a tough but temporary process as your brain and body relearn how to work on their own again.”
Common Withdrawal Symptoms At a Glance
Withdrawal looks different for everyone, but many symptoms are common across various substances. Here’s a quick look at what you might experience.
| Symptom Category | Common Examples |
|---|---|
| Physical Symptoms | Nausea, vomiting, diarrhea, muscle and bone pain, sweating, chills, tremors, fatigue, headaches, runny nose, goosebumps |
| Psychological Symptoms | Anxiety, depression, irritability, intense cravings, mood swings, confusion, insomnia, poor concentration, paranoia |
It’s important to remember that this isn’t an exhaustive list, and the intensity can vary dramatically depending on the substance, duration of use, and your own unique physiology.
The potential for dependence is more widespread than many realize. Back in 2018, the Centers for Disease Control and Prevention (CDC) reported that over 11% of Americans aged 12 or older had used an illicit substance in the past month. For a deeper dive into withdrawal timelines and treatments, American Addiction Centers offers some excellent resources.
While withdrawal is always challenging, some substances, particularly opioids, can produce incredibly severe symptoms. It’s crucial to understand the risks, which is why we put together a guide exploring the question of whether heroin withdrawal can be fatal.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
The Science of Why Withdrawal Feels So Intense

If you’ve ever wondered why withdrawal feels so physically and emotionally brutal, it’s not about a lack of willpower. It’s about biology. To really get why the experience is so overwhelming, we have to pull back the curtain and look at what’s happening inside the brain.
At its heart, the brain is an incredible balancing act. Its main job is to keep everything on an even keel, a state scientists call homeostasis. Think of it like a very sophisticated thermostat, constantly making tiny adjustments to keep your internal world stable and comfortable.
How Substances Change the Brain
When a drug or alcohol enters the picture, it throws that finely tuned system completely out of whack. Many substances, particularly addictive ones, hijack the brain’s reward system by flooding it with dopamine—the neurotransmitter that makes us feel pleasure and motivation.
The brain, in its endless quest for balance, sees this massive chemical flood and hits the brakes. It starts producing less of its own dopamine and even shuts down some of the receptors that pick it up. It’s the brain’s way of saying, “Whoa, it’s way too hot in here,” and turning down its internal furnace. This fundamental adjustment is called neuroadaptation.
With repeated use, the brain doesn’t just adapt; it completely rewires itself. It creates a new “normal” where the substance isn’t just a visitor—it’s a required part of the daily chemical equation.
The Shock of a Sudden Stop
So, what happens when you suddenly take that substance away? The artificial supply of feel-good chemicals is cut off, but the brain’s own production is still dialed way, way down. The thermostat, which got used to an external heater, is now stuck in the off position during a blizzard.
The result is a chemical panic. Your system goes into overdrive trying to rebalance, creating the intense physical and emotional storm of withdrawal. Your brain is essentially sending out a desperate S.O.S., screaming for the one thing it thinks it needs to function.
“Withdrawal is the painful, chaotic period where the brain struggles to reset its internal thermostat back to its original, natural setting after being artificially controlled for so long.”
This biological battle is what you feel as drug withdrawal symptoms. For instance, if you stop using a substance that suppresses the nervous system, you can expect a massive rebound effect—anxiety, shakiness, or in severe cases, even seizures.
Understanding Tolerance and Dependence
This whole process also explains tolerance. It’s why you eventually need more and more of a substance just to feel the same effects. As the brain becomes less sensitive to the chemical flood, it takes a higher dose to get the job done. Tolerance and dependence are two sides of the same coin, both born from the brain’s relentless drive to find equilibrium.
Let’s break down the core ideas:
- Homeostasis: This is the brain’s baseline—its natural, stable chemical balance.
- Neuroadaptation: This is how the brain physically changes its wiring and chemistry to cope with the regular presence of a substance.
- Dependence: This is the state where the brain needs the substance to maintain its new, altered balance. When it’s gone, withdrawal begins.
Grasping this science is a game-changer for anyone in recovery. It shifts the narrative from one of personal failure to a predictable, physiological process of healing. Your body isn’t betraying you; it’s fighting like hell to get back to its natural state. It’s a tough journey, one that requires patience and, very often, professional help to see through safely.
Withdrawal Timelines for Common Substances
Trying to understand a drug withdrawal timeline can feel a lot like getting a weather forecast before a big storm. You know something is coming, but you can’t predict the exact timing or intensity. Still, knowing the general pattern—when symptoms start, when they’ll be at their worst, and how long they might last—is incredibly helpful for preparing yourself. Just remember, these are guides, not guarantees. Everyone’s body and experience are different.
This isn’t just a personal struggle; it’s a global health issue. The numbers are staggering. It’s estimated that 18.4% of adults worldwide engage in heavy episodic drinking, and 15.2% are daily smokers. When you factor in other substances, you realize millions face withdrawal every year. The stakes are high, too. Untreated alcohol withdrawal can lead to delirium tremens, a condition with a mortality rate as high as 5%. You can dig deeper into these global statistics in a detailed StatPearls review on substance withdrawal.
The image below gives you a visual roadmap of what to expect—from the first signs of trouble to the peak of the storm and, finally, to when things start to calm down.
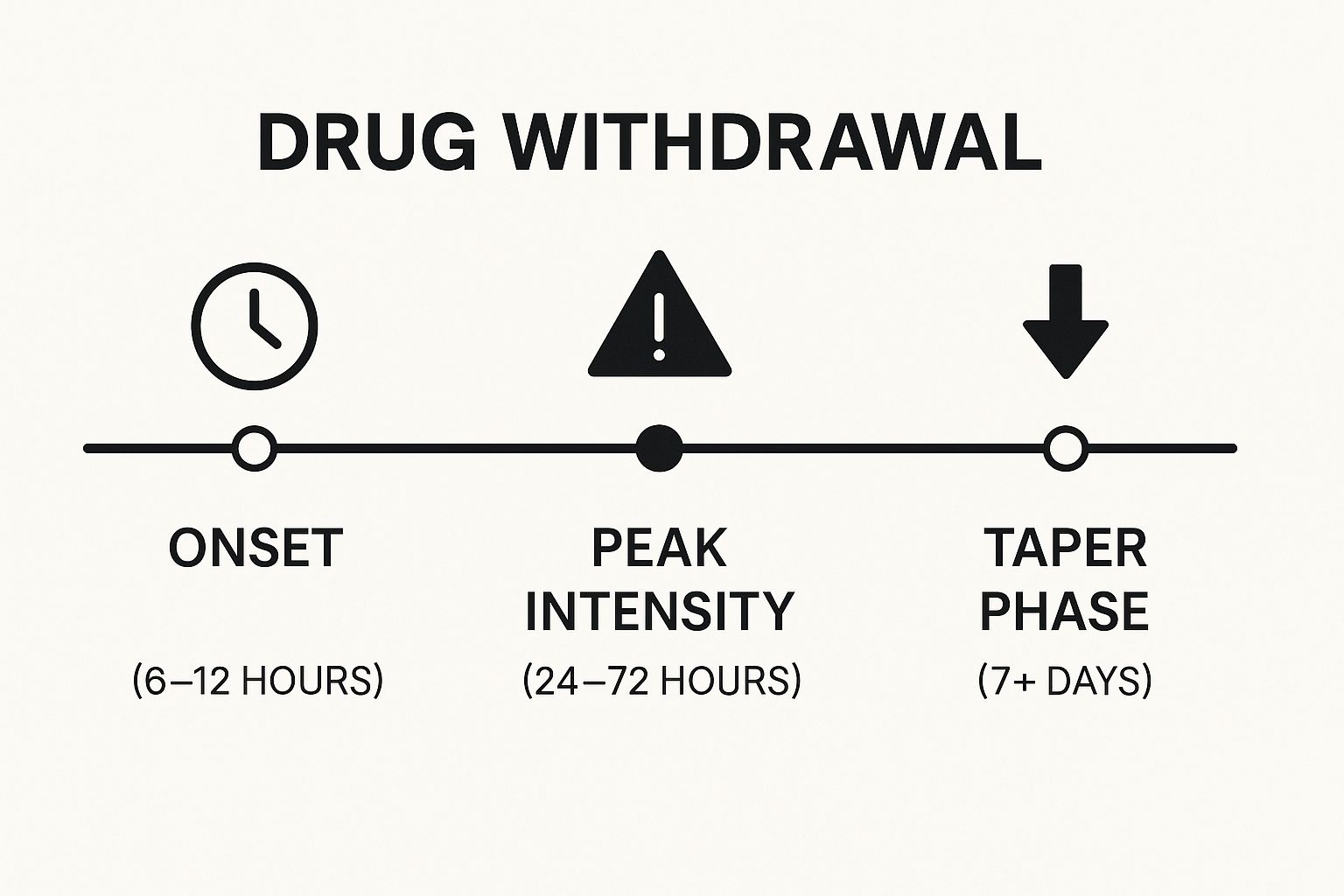
As you can see, those first few days are often the most difficult. This is the critical window where getting professional medical support can make all the difference.
To give you a clearer picture, I’ve broken down the timelines for some of the most common substances people struggle with. This table offers a quick side-by-side comparison.
Typical Withdrawal Timelines by Substance
| Substance | Symptom Onset | Peak Intensity | Typical Duration |
|---|---|---|---|
| Alcohol | 6–12 hours | 24–72 hours | 5–7 days |
| Short-Acting Opioids | 8–24 hours | 48–72 hours | 4–10 days |
| Stimulants | Within hours | 24–72 hours | 1–2 weeks |
| Benzodiazepines | 1–7 days | Around 2 weeks | Several weeks+ |
As these timelines show, the experience varies dramatically depending on the drug. Let’s break down what each of these really looks and feels like.
H3: Timeline for Alcohol Withdrawal
Since alcohol is a depressant, your brain gets used to functioning in a slowed-down state. When the alcohol is removed, the brain rebounds with a jolt, and symptoms can start surprisingly fast.
- Onset: You can start feeling the effects within just 6 to 12 hours after your last drink.
- Peak: This is the most dangerous period. Symptoms like seizures and delirium tremens (DTs) are most likely to occur between 24 and 72 hours.
- Duration: The most severe symptoms usually start to fade within 5 to 7 days, though it’s common to feel “off” for several more weeks.
I can’t stress this enough: because alcohol withdrawal can be fatal, it’s something you should never attempt on your own. Medically supervised detox is the only safe way to do it.
H3: Timeline for Opioid Withdrawal
Opioid withdrawal timelines really depend on the specific drug. Short-acting opioids hit fast and hard, while long-acting ones create a more drawn-out process.
Short-Acting Opioids (Heroin, Fentanyl, Oxycodone) People often describe this as the worst flu of their life. It’s intensely miserable, though it’s not typically life-threatening on its own.
- Onset: Symptoms usually kick in within 8 to 24 hours after the last dose.
- Peak: Expect the worst of it around the 48 to 72-hour mark, with severe muscle aches, nausea, and cramping.
- Duration: The acute phase, where you feel the sickest, generally lasts for 4 to 10 days.
If you’re dealing with heroin, knowing the specifics can help you prepare. We have a guide that explains in more detail how long it takes to detox from heroin.
Long-Acting Opioids (Methadone) Because these substances linger in your system, the withdrawal process is much more gradual and prolonged.
- Onset: It can take 2 to 4 days before you even start to feel symptoms.
- Peak: The peak intensity is delayed, often occurring several days into the process.
- Duration: The whole ordeal can easily last 10 days or even longer.
H3: Timeline for Stimulant Withdrawal
Withdrawal from stimulants like cocaine or meth is a completely different beast. It’s often called a “crash,” and the battle is more psychological than physical.
- Onset: The crash can start almost immediately, sometimes just hours after the last use.
- Peak: The first 24 to 72 hours are marked by profound fatigue, deep depression, and powerful cravings.
- Duration: While the initial crash subsides, the psychological fallout—depression, anxiety, and cravings—can stick around for weeks or even months.
“The real danger with stimulant withdrawal isn’t so much physical, but the crushing psychological weight. The intense cravings and severe depression create a very high risk for relapse.”
H3: Timeline for Benzodiazepine Withdrawal
Like alcohol, “benzos” are central nervous system depressants, and stopping them can be both dangerous and drawn-out. A slow, medically guided taper is the only safe approach.
- Onset: For short-acting benzos like Xanax, withdrawal can start in 1 to 2 days. For longer-acting ones like Valium, it might not begin for 2 to 7 days.
- Peak: Symptoms often reach their most severe point around the second week.
- Duration: The acute phase can last for several weeks. Many people then experience a “protracted withdrawal” where symptoms can pop up unpredictably for months or even years.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Tapering Off Antidepressants: What to Expect

When we talk about drug withdrawal symptoms, our minds often jump to substances like alcohol or opioids. But there’s another class of medication that comes with a completely different, and often misunderstood, withdrawal process: antidepressants.
First, let’s be clear. Antidepressants aren’t addictive in the classic sense—they don’t cause cravings or the kind of compulsive use seen with illicit drugs. However, stopping them can trigger a very real and difficult set of symptoms, especially if you do it too quickly. This is known as antidepressant discontinuation syndrome. It’s not a moral failing; it’s a physical response. Your brain has simply gotten used to the medication and needs time to adjust.
What Does Antidepressant Withdrawal Feel Like?
Imagine your brain’s chemistry is like a complex soundboard. For a while, the medication has been helping manage the levels of certain neurotransmitters, like serotonin. When you suddenly take it away, the controls are all out of whack, and your brain scrambles to find its equilibrium. This is what causes that disorienting cascade of symptoms.
Many people experience a range of physical and psychological effects, including:
- Dizziness and Vertigo: That frustrating, off-balance feeling that makes it hard to focus.
- “Brain Zaps”: A bizarre but common sensation often described as a brief electric shock in your head.
- Nausea and Flu-Like Symptoms: You might feel achy, tired, and generally unwell.
- Sensory Disturbances: Lights may seem too bright, and normal sounds can feel jarring.
- Mood Shifts: Irritability, anxiety, and strange, vivid dreams are also common.
It’s so important to remember that these are physiological reactions to a chemical change. They aren’t a sign that you’re “not strong enough” or that your original condition is immediately returning, though it can certainly feel that way.
“Antidepressant discontinuation syndrome is a real clinical issue. Research points to a 15% absolute risk increase for withdrawal symptoms after someone stops their medication. These effects aren’t just minor annoyances; they can be severe and, in some cases, linger for months or even years.”
The Critical Role of a Medically Supervised Taper
This is exactly why you should never stop taking an antidepressant “cold turkey.” The only safe and effective way to come off these medications is to work with your doctor on a slow, deliberate tapering plan. This usually means reducing your dose bit by bit over several weeks or months.
This gradual reduction gives your brain the time it needs to recalibrate and slowly start managing its own neurotransmitter production again. A slow taper is the best tool you have to minimize the intensity of discontinuation symptoms and make the process as smooth as possible.
Is It Withdrawal or Relapse?
One of the trickiest parts of this process is figuring out if what you’re feeling is a withdrawal symptom or a sign that your depression or anxiety is returning. The key differences usually come down to the timing and the nature of the symptoms.
| Symptom Type | Antidepressant Withdrawal | Depression or Anxiety Relapse |
|---|---|---|
| Onset | Hits you quickly, often within a few days of lowering or stopping your dose. | Tends to creep back in gradually over several weeks or even months. |
| Nature | Often includes distinct physical feelings you didn’t have before, like “brain zaps” or dizziness. | Usually feels like a return of your original mood symptoms, such as deep sadness, loss of interest, or persistent worry. |
| Resolution | Symptoms typically get better if you go back to your previous dose (under medical guidance). | Symptoms don’t go away just by reinstating the medication. |
Understanding this difference is vital for working with your doctor to make the right call for your health. While discontinuing antidepressants is a very different experience from the acute physical process detailed in guides like the heroin withdrawal timeline, it still demands careful management, professional guidance, and plenty of self-compassion.
Practical Strategies for Managing Symptoms
Knowing what withdrawal symptoms to expect is one thing, but actually getting through them is a whole different ball game. While a medically supervised detox is the only truly safe path, there are things you can do to support yourself and ease some of the physical and mental strain along the way.
Think of it like recovering from a nasty flu. You can’t just will it away, but you can create the right conditions for your body to heal. You drink fluids, eat simple foods, and get plenty of rest. These small, practical steps build a foundation of stability while your body does the hard work of getting back to normal.
Nurturing Your Body and Mind
Your body is working overtime to find its equilibrium again, and that process burns a massive amount of physical and mental energy. Taking care of the basics can make a world of difference in how you feel from one hour to the next. The goal isn’t to erase the discomfort, but to turn the volume down.
Start with small, manageable goals. Don’t overwhelm yourself.
- Stay Hydrated: Dehydration is a huge issue during withdrawal, especially if you’re dealing with sweating, vomiting, or diarrhea. Keep a water bottle with you at all times and take small sips, even if you don’t feel thirsty.
- Prioritize Gentle Nutrition: An upset stomach makes eating seem impossible. Stick with bland, easy-to-digest foods—think bananas, rice, applesauce, and toast (the BRAT diet). Small, frequent snacks are usually much easier to handle than three big meals.
- Create a Restful Environment: Your nervous system is on high alert, so minimize stress wherever you can. Dim the lights, cut down on noise, and let people know you need some quiet time. A calm space is a powerful tool.
“Remember, these strategies are designed to support a medically supervised detox, not replace it. Your primary focus should be on safety and following the guidance of healthcare professionals.”
Soothing Physical Discomfort
Those deep muscle aches, the chills, and that awful restlessness can be completely draining. You won’t feel like running a marathon, but some very gentle movement can bring surprising relief.
Here are a few simple things to try:
- Warm Baths: Never underestimate the power of a warm bath. Adding some Epsom salts can help relax knotted muscles and soothe those persistent aches. The warmth itself is incredibly calming.
- Gentle Stretching: You don’t need to do a full yoga routine. Just a few slow, simple stretches can release tension and get your blood moving. Focus on tight spots like your neck, back, and legs.
- Mindful Breathing: When a wave of anxiety hits, your breathing gets fast and shallow, making everything feel worse. Try this: breathe in slowly through your nose for 4 seconds, hold it for 4, and then exhale slowly through your mouth for 6. This simple act can kickstart your body’s natural relaxation response.
Managing Psychological Challenges
For many people, the mental and emotional side of withdrawal is the toughest part. The anxiety, the irritability, the mood swings, and the powerful cravings can feel relentless. Having a few tools in your back pocket is essential.
Distraction is your best friend here. Find low-energy activities that can occupy your mind, like listening to a podcast, watching a comforting movie, or getting lost in a simple book.
It’s also a time for radical self-compassion. Remind yourself that these feelings are a normal part of healing and that they will pass. Understanding what’s happening in your brain can also take away some of the fear. To learn more, check out our guide on how long cravings last and how to beat them.
When You Must Seek Professional Medical Help

While many drug withdrawal symptoms are incredibly uncomfortable, some are much more than that—they’re genuine medical emergencies. Trying to “tough it out” alone, especially with certain substances, is like trying to navigate a hurricane in a rowboat. The risks are just too high.
Your health and safety have to be the top priority. For substances like alcohol and benzodiazepines, quitting cold turkey can be fatal. When the body rebounds after being dependent on these depressants, it can trigger a cascade of severe complications that need immediate medical attention to prevent permanent damage or even death.
Recognizing Life-Threatening Red Flags
You absolutely have to know which symptoms are waving a giant red flag. If you or someone you’re with experiences any of the following, it’s not a “wait and see” situation. It’s time to act.
These are dangerous warning signs that require an emergency response:
- Seizures or convulsions, which can strike without any warning.
- Hallucinations, meaning seeing or hearing things that aren’t actually there.
- Delirium tremens (DTs), a severe form of alcohol withdrawal that brings on intense confusion, a racing heart, and high fever.
- Severe confusion or disorientation that makes it impossible to think straight.
- Suicidal thoughts or self-harming behaviors, which can become dangerously intense during withdrawal.
“Think of these symptoms with the same urgency as a heart attack or a stroke. Don’t hesitate or hope it will pass. Call 911 or get to the nearest emergency room immediately.”
The Safety of Medically Supervised Detox
This is precisely why professional help isn’t just a good idea—it’s essential. A medically supervised detox program provides a safe, controlled environment where your vital signs are monitored 24/7 by people who know exactly what to look for.
These medical professionals are ready to manage dangerous drug withdrawal symptoms with medication, keeping you stable and as comfortable as possible. This isn’t just about getting through the worst of it; it’s about setting you up for a successful recovery.
In a professional detox facility, you’re not only safe from the immediate medical risks but also protected from the temptation to relapse. It’s a compassionate and structured start that dramatically improves your odds of moving on to the next stage of your treatment.
If you’re ready to take that critical first step, learning how to get into rehab can give you a clear roadmap. Making that call might just be the most important thing you ever do for yourself.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Your Top Questions About Drug Withdrawal, Answered
When you’re thinking about recovery, it’s natural to have a lot of questions. Getting straight answers about the withdrawal process can clear up some of the mystery and show why getting professional support is so important. Let’s tackle some of the most common concerns.
Can I Just Detox from Drugs at Home?
Going it alone and trying to detox at home is something we strongly advise against. For certain substances, especially alcohol and benzodiazepines, withdrawal can be more than just uncomfortable—it can be downright dangerous, leading to seizures or delirium tremens without a doctor’s watch.
Even beyond the immediate physical dangers, the sheer intensity of withdrawal symptoms makes the risk of relapse incredibly high. A medically supervised detox program gives you a safe space where professionals can manage your symptoms, which not only keeps you safe but also gives you a much better shot at making it through. The first step should always be talking to a healthcare professional before you stop using any substance.
What Is Post-Acute Withdrawal Syndrome (PAWS)?
Once the initial, intense phase of withdrawal is over, some people experience what’s known as Post-Acute Withdrawal Syndrome, or PAWS. These are symptoms that can stick around for weeks, months, or sometimes even longer, and they tend to be more emotional and psychological.
You might experience things like:
- Mood swings that seem to come out of nowhere
- A nagging sense of anxiety or irritability
- Feeling drained and tired all the time
- Trouble sleeping through the night
- Brain fog or difficulty concentrating
PAWS is basically your brain’s way of slowly recalibrating its chemistry after a long period of substance use. Knowing that these challenges might pop up is a huge part of long-term recovery, as it allows you to prepare and build coping skills to stay on track.
Is Withdrawal the Same for Everyone?
Not at all. The withdrawal journey is deeply personal, and what one person goes through can be completely different from another’s experience.
“Your personal withdrawal journey is shaped by a unique combination of elements, including the specific substance used, the duration and amount of use, your overall physical and mental health, and even your genetics.”
While we can talk about general timelines, your path will be your own. This is exactly why a one-size-fits-all approach doesn’t work. A personalized, medically supervised detox plan is designed around you to make the process as safe and smooth as possible.
If you or someone you care about is struggling, please know you aren’t alone. Addiction Helpline America is a confidential, 24/7 resource that can connect you with the right help. Call us anytime to find the support you need to start your journey. You can learn more by visiting Addiction Helpline America’s website.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.















