
Free 24/7 Confidential Schizophrenia Treatment Helpline
Drug treatment for schizophrenia is the cornerstone of managing this chronic mental health condition. Here’s a quick overview:
- Primary Treatment: Antipsychotic medications are the main therapy.
- Two Main Types: First-generation (conventional) and second-generation (atypical) antipsychotics.
- How They Work: They alter brain chemicals like dopamine and serotonin to control symptoms.
- Treatment Duration: Most individuals require long-term medication to prevent relapse.
- Success Rate: Maintenance therapy reduces relapse from 60-80% down to 18-32%.
- Most Prescribed: Olanzapine, quetiapine, and risperidone are frequently used in the U.S.
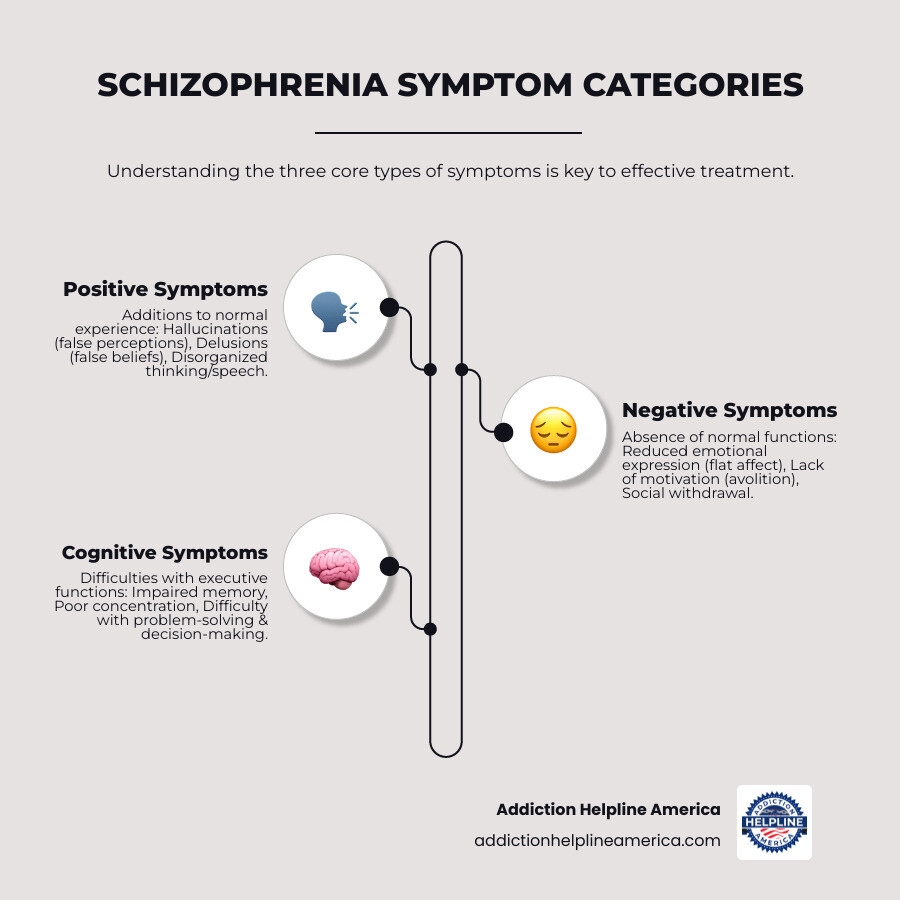
Schizophrenia is a serious brain disorder causing hallucinations, delusions, and disorganized thinking. Early treatment is crucial for improving long-term outcomes. Without proper medication, individuals face higher risks of disability, hospitalization, and premature death, with nearly 5% dying by suicide.
The good news is that medication works. Antipsychotics have been used since the 1950s, and modern options are more effective with fewer side effects. While not a cure, medication is an essential tool that, combined with therapy and support, helps many people lead productive lives.
At Addiction Helpline America, we know navigating treatment can be overwhelming, especially with co-occurring substance use. Our specialists connect people with comprehensive programs that address both psychiatric conditions and addiction, ensuring you receive the coordinated care needed for recovery.
Relevant articles related to drug treatment for schizophrenia:
Understanding Antipsychotic Medications and How They Work
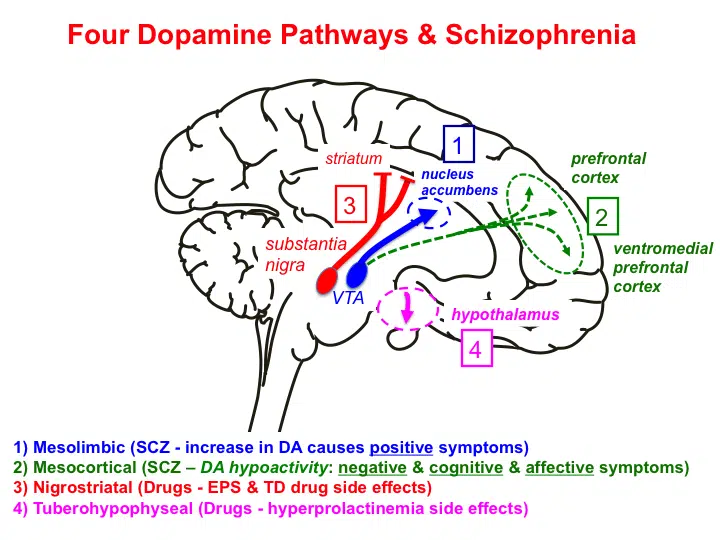
Antipsychotic medications are the primary drug treatment for schizophrenia. They work by restoring balance to brain chemistry, specifically targeting neurotransmitters like dopamine and serotonin.
The leading theory, the dopamine hypothesis, suggests that an excess of dopamine in certain brain areas causes positive symptoms like hallucinations and delusions. Antipsychotics work by blocking dopamine receptors, effectively “turning down the volume” on these experiences. Newer medications also interact with serotonin receptors, which helps address a wider range of symptoms with fewer side effects.
While some relief from agitation may occur in days, it typically takes four to six weeks for medications to significantly reduce core symptoms like hallucinations. Finding the right medication and dose is a process that requires patience and communication with your doctor.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Main Classes of Medications for Schizophrenia
Understanding the main categories of antipsychotics can help you have more informed conversations with healthcare providers.
- First-generation antipsychotics (FGAs): These older, or “conventional,” drugs primarily block dopamine D2 receptors. They are effective for positive symptoms but have a higher risk of movement-related side effects.
- Second-generation antipsychotics (SGAs): Known as “atypical” antipsychotics, these are the current standard of care. They block dopamine and also interact with serotonin receptors, resulting in a lower risk of movement side effects and potential improvement in negative symptoms (e.g., emotional flatness, lack of motivation).
- Third-generation antipsychotics: This newer class (e.g., aripiprazole) acts as a dopamine stabilizer. They block dopamine where it’s too high and stimulate it where it’s too low, offering a unique side effect profile.
- Long-acting injectables (LAIs): These are not a separate class but a delivery method. Available for both FGAs and SGAs, LAIs are administered every few weeks or months, providing steady medication levels and eliminating the need for daily pills. This can be life-changing for those who struggle with medication adherence.
- Treatment-resistant options: For the 30% of individuals who don’t respond to standard treatments, clozapine is often the most effective option, though it requires regular blood monitoring for safety.
How Antipsychotics Manage Symptoms
Antipsychotics work to stabilize brain activity and reduce psychosis. By blocking dopamine D2 receptors, they reduce the overactivity that drives hallucinations and delusions. The interaction with serotonin receptors, particularly in SGAs, helps lessen movement problems and may improve negative and cognitive symptoms. The ultimate goal is to restore clearer, more organized thinking and a stronger connection to reality.
At Addiction Helpline America, we know that understanding medication is just one piece of the puzzle. Our team can connect you with specialists who take the time to explain your options and find the right fit. Recovery is about comprehensive care that addresses all aspects of healing.
A Deep Dive into Antipsychotic Types: Conventional vs. Atypical
When exploring drug treatment for schizophrenia, it’s crucial to understand the two main categories: first-generation (conventional) and second-generation (atypical) antipsychotics. They both reduce psychotic symptoms but have different approaches and side effect profiles.
| Feature | First-Generation (Conventional) Antipsychotics (FGAs) | Second-Generation (Atypical) Antipsychotics (SGAs) |
|---|---|---|
| Mechanism of Action | Primarily dopamine D2 receptor blockade | Dopamine D2 and serotonin 5-HT2A receptor interaction |
| Primary Target Symptoms | Positive symptoms (hallucinations, delusions) | Positive, negative, and cognitive symptoms |
| Movement Side Effects | Higher risk (EPS, tardive dyskinesia) | Lower risk |
| Metabolic Side Effects | Lower risk | Higher risk (weight gain, diabetes, hyperlipidemia) |
| Examples | Haloperidol, Chlorpromazine, Fluphenazine | Olanzapine, Quetiapine, Risperidone, Aripiprazole |
| First-Line Treatment | Less common, often reserved for specific cases | Usually preferred |
Choosing a medication involves considering your unique situation and preferences. Concerns about weight gain versus movement problems, or a preference for a daily pill versus a long-acting injection, are important factors in finding the right fit.
More info about addiction and mental health treatment.
First-Generation (Conventional) Antipsychotics
First-generation antipsychotics (FGAs) like chlorpromazine and haloperidol were in the 1950s. They are effective for positive symptoms but carry a higher risk of movement-related side effects, known as extrapyramidal symptoms (EPS). These can include muscle stiffness, restlessness, and tremors.
The most serious risk is tardive dyskinesia, which involves involuntary, repetitive movements (e.g., lip-smacking, grimacing) that can become permanent. Due to these risks, FGAs are now less commonly used as a first-line treatment, but they remain an important option.
Second-Generation (Atypical) Antipsychotics
Second-generation antipsychotics (SGAs) are the current standard of care. This class includes aripiprazole (Abilify), olanzapine (Zyprexa), quetiapine (Seroquel), and risperidone (Risperdal). They were developed to reduce the risk of movement disorders. The risk of tardive dyskinesia is significantly lower with SGAs.
However, SGAs come with a trade-off: a higher risk of metabolic side effects. These include significant weight gain, increased blood sugar leading to type 2 diabetes, and high cholesterol. Because of this, regular monitoring of weight, blood sugar, and lipids is essential. Despite these risks, their effectiveness and better tolerability regarding movement make them the preferred choice for most individuals starting treatment.
More info about finding the right rehab program.
Managing Side Effects and Long-Term Use of Drug Treatment for Schizophrenia
Long-term drug treatment for schizophrenia requires careful management of side effects to ensure the medication works for your life. This involves regular monitoring and open communication with your doctor to find the right balance between effectiveness and tolerability.
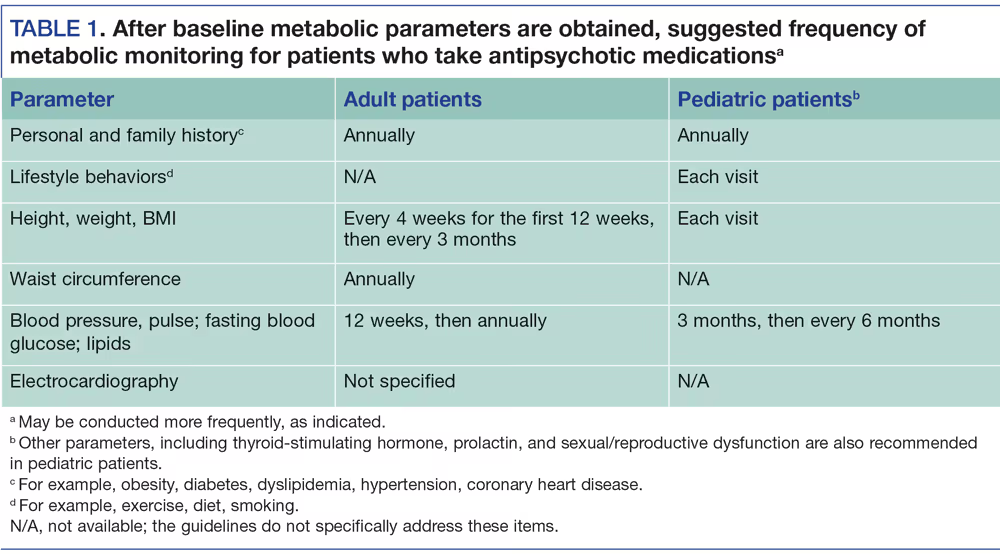
Regular monitoring is your safety net. For atypical antipsychotics, this means checking weight, blood sugar, and cholesterol to catch metabolic changes early. For clozapine, it involves critical blood tests to monitor for a rare but serious drop in white blood cells.
Common Side Effects and How to Manage Them
Most side effects can be managed. Here are some common ones:
- Movement disorders (EPS): More common with older drugs, these include stiffness, tremors, and restlessness. Management may involve dose adjustments, switching medications, or adding another drug to counteract the effects.
- Tardive dyskinesia (TD): This serious condition involves involuntary movements and can be permanent. Regular screening by your doctor is crucial for early detection.
- Metabolic changes: Weight gain, high blood sugar, and cholesterol issues are common with newer drugs. Management requires a team approach, including diet, exercise, and consistent monitoring.
- Other common effects: Drowsiness, dizziness, dry mouth, and constipation can often be managed with simple strategies like taking medication at night, rising slowly, using sugar-free gum, and increasing fiber and water intake. Sexual dysfunction is also common and should be discussed with your doctor, as solutions are available.
- Rare but serious risks: Neuroleptic malignant syndrome (fever, muscle rigidity) and agranulocytosis (a drop in white blood cells, mainly with clozapine) are medical emergencies that require immediate attention.
At Addiction Helpline America, we connect people with providers who take these concerns seriously and work collaboratively to find solutions.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Benefits and Risks of Long-Term Antipsychotic Use
For most people, long-term medication is essential for stability.
Benefits:
- Relapse Prevention: Continuing medication reduces relapse risk from 60-80% to 18-32%.
- Reduced Hospitalizations: Preventing relapse keeps people out of the hospital and living their lives.
- Improved Quality of Life: Stability allows individuals to engage in therapy, work, and relationships.
Risks:
- Persistent Side Effects: Long-term use can lead to permanent tardive dyskinesia or chronic conditions like diabetes and heart disease from metabolic changes.
- Adherence Challenges: Up to 60% of people struggle to take medication consistently. Long-acting injectables (LAIs) are an effective solution for this, providing steady medication levels without daily pills.
The decision to continue long-term treatment is a personal one, made by weighing the powerful benefits against the potential risks in conversation with your doctor.
Scientific research on long-acting vs oral antipsychotics shows that LAIs can be highly effective for maintaining treatment adherence and preventing relapse.
Modern and Complementary Treatment Strategies
Medication is foundational, but the most successful drug treatment for schizophrenia combines it with therapy and support. This holistic approach addresses both the biological and practical aspects of recovery.
Coordinated Specialty Care (CSC) is a highly effective model that integrates medication management, psychotherapy, family education, and employment/education support. It helps people stick with treatment and improves their quality of life. Other key strategies include:
- Long-acting injectables (LAIs): These injections, given every few weeks or months, are a practical solution for those who struggle with daily pills, ensuring consistent medication levels and preventing relapse due to missed doses.
- Electroconvulsive Therapy (ECT): This medical procedure can be remarkably effective for treatment-resistant schizophrenia when multiple medications have failed.

Newer Medications and Future Directions in Drug Treatment for Schizophrenia
The field of drug treatment for schizophrenia is evolving. For decades, all antipsychotics targeted dopamine. A recent breakthrough, Cobenfy (xanomeline-trospium), is the first FDA-approved treatment that works differently, by activating muscarinic receptors. This offers a new option that may avoid some of the metabolic side effects (like weight gain) associated with traditional antipsychotics.
Researchers are also exploring other novel mechanisms, such as TAAR-1 agonists, which show promise for treating the negative and cognitive symptoms that are often harder to manage. This innovation offers hope for more effective treatments with fewer side effects.
The Lancet study on Cobenfy’s efficacy.
The Role of Other Medications in a Comprehensive Drug Treatment for Schizophrenia
Antipsychotics are the primary medication, but other drugs may be used to manage co-occurring symptoms. A psychiatrist might add mood stabilizers for mood swings, antidepressants for co-occurring depression, or short-term anti-anxiety medications for acute distress. This requires careful management by a specialist to ensure a safe and effective combination.
More info on antidepressants for related disorders.
How Psychosocial Therapies Complement Medication
Medication can reduce symptoms, but therapy teaches life skills. These interventions are essential for a full recovery.
- Cognitive Behavioral Therapy (CBT) helps individuals change problematic thought patterns and develop coping strategies for symptoms.
- Social skills training teaches practical skills for interacting with others, reducing isolation.
- Family therapy educates families, improves communication, and creates a supportive home environment.
- Vocational rehabilitation helps people find and maintain employment, which builds self-esteem and structure.
- Psychoeducation and support systems (family, friends, peer groups) provide crucial encouragement and help individuals stay engaged in their treatment.
Combining medication with these therapies creates the conditions for genuine recovery and a better quality of life. At Addiction Helpline America, we connect people with programs that offer this integrated approach.
Frequently Asked Questions about Schizophrenia Medication
Navigating drug treatment for schizophrenia brings up many questions. Here are answers to some of the most common concerns.
How long does it take for schizophrenia medication to work?
It varies by symptom. Relief from acute agitation can begin within a few days. However, for core psychotic symptoms like hallucinations and delusions, it typically takes 4 to 6 weeks to see significant improvement. Finding the right medication and dose is a process that requires patience and open communication with your doctor, as responses vary from person to person.
Is lifelong medication necessary for schizophrenia?
For the vast majority of individuals, yes, lifelong medication is recommended. Schizophrenia is a chronic condition, and continuous treatment is the most effective way to manage symptoms and prevent relapse. The evidence is compelling:
- With maintenance therapy, the relapse rate is 18% to 32%.
- For those who stop medication, the relapse rate jumps to 60% to 80%.
Any decision to reduce or stop medication must be made in close consultation with a psychiatrist, as the risk of relapse is substantial.
What happens if you miss a dose of antipsychotic medication?
Missing a single dose is unlikely to cause a crisis, so don’t panic. However, consistency is crucial. These medications work best when they maintain a steady level in your system. Frequently missed doses can lead to a return of symptoms and increase the risk of a full relapse.
If you struggle to remember daily pills, talk to your doctor. Long-acting injectable (LAI) antipsychotics, given every few weeks or months, are an excellent option to ensure consistent medication levels and improve adherence. If you miss a dose, contact your doctor or pharmacist for guidance instead of double-dosing.
At Addiction Helpline America, we help you find providers who can offer practical solutions, including LAIs, to support your long-term recovery.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Finding the Right Path to Recovery
Finding the right drug treatment for schizophrenia can be complex, but recovery is possible. You do not have to steer this journey alone.
Medication is a powerful tool that controls symptoms and prevents hospitalization, creating the stability needed to build the life you want. When combined with therapy and a supportive treatment team, it becomes the foundation for hope and recovery. The best treatment is personalized, respecting your goals and concerns about side effects.
At Addiction Helpline America, we connect individuals and families across all fifty states with comprehensive treatment programs. We specialize in finding care for co-occurring disorders, such as schizophrenia and substance use, treating the whole person.
Our services are free, confidential, and personalized. We listen to your situation and help you find the specialized care you need, whether it’s a specific type of therapy or a psychiatrist who understands your unique challenges. Many people with schizophrenia lead fulfilling, independent lives. With the right support, that future is within reach.
Find professional help for mental health and addiction.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.















