Understanding Medications for Bipolar Disorder
A drug for bipolar disorder is a cornerstone of treatment, helping manage the extreme mood swings of this lifelong condition. Here are the key takeaways:
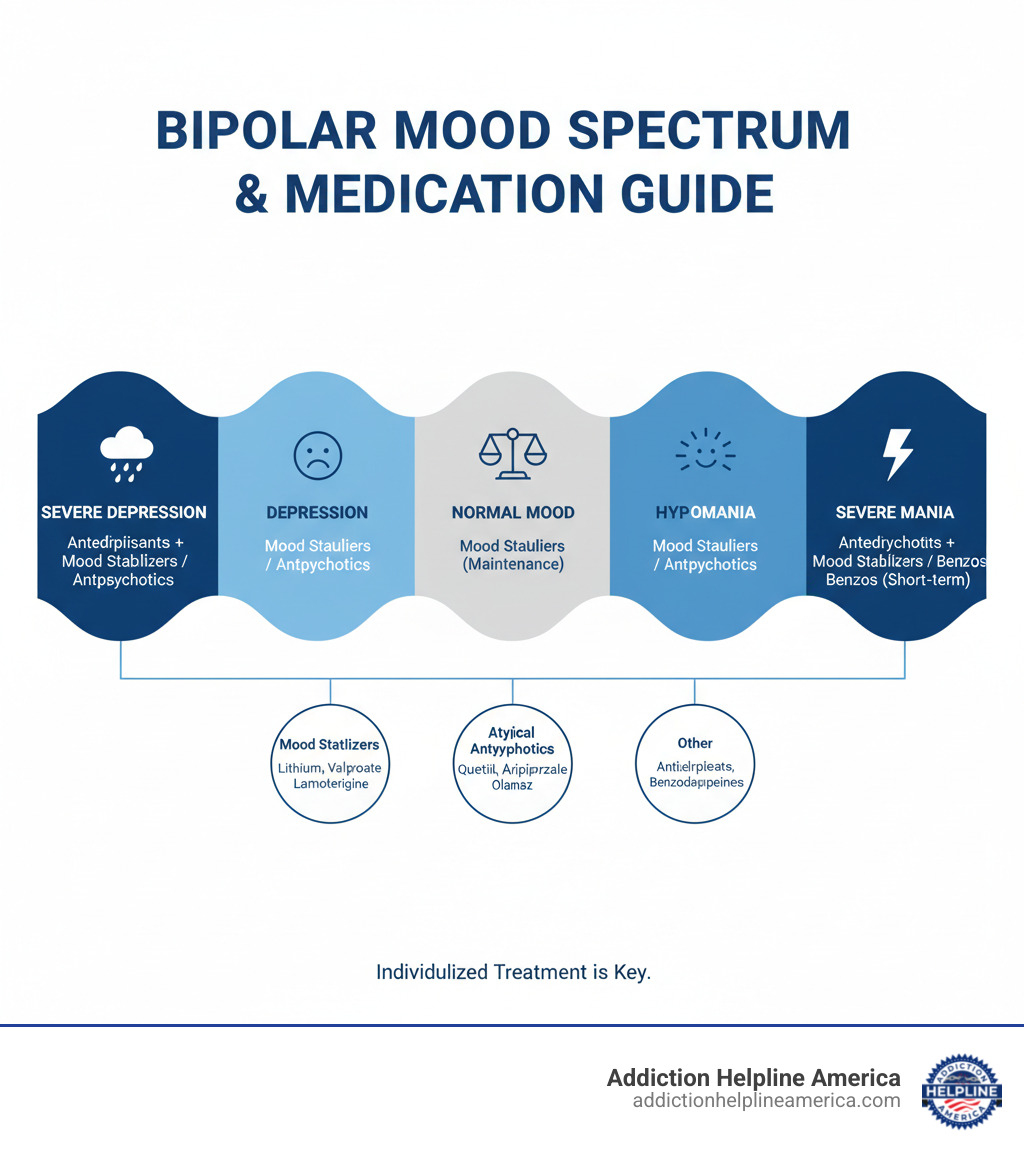
Main Drug Classes:
- Mood Stabilizers: Lithium, valproate (Depakote), lamotrigine (Lamictal)
- Atypical Antipsychotics: Quetiapine (Seroquel), aripiprazole (Abilify), olanzapine (Zyprexa)
- Antidepressants: Used cautiously with a mood stabilizer for bipolar depression.
- Anti-anxiety Medications: Benzodiazepines for short-term relief.
Key Facts:
- Treatment is highly individualized.
- Medications can take up to 8 weeks to show full effects.
- Most people need long-term treatment to prevent relapse.
- Medication works best when combined with therapy and lifestyle changes.
Bipolar disorder causes dramatic shifts between manic episodes (high energy, euphoria, irritability) and depressive episodes (sadness, hopelessness, fatigue). Medications act like eyeglasses, helping to correct the mood distortions the disorder creates.
Finding the right medication requires patience and collaboration with your doctor. Some drugs treat acute episodes, while others provide maintenance to prevent future ones. Success depends on consistent adherence, open communication about side effects, and regular monitoring.
At Addiction Helpline America, we know navigating treatment is overwhelming, especially when substance use is involved. We connect people with care that addresses both mental health and addiction, helping you find the right drug for bipolar disorder and support for lasting recovery.
Simple drug for bipolar disorder word guide:
Primary Classes of Medication for Bipolar Disorder
There’s no single magic pill for bipolar disorder. Your treatment will be unique, shaped by your symptoms and how your body responds. Most people find a combination of medications works best to stabilize mood and reduce the frequency and severity of episodes. Working closely with a psychiatrist is essential.
Mood Stabilizers: The Foundation of Treatment
Mood stabilizers are the cornerstone of bipolar treatment, helping to prevent the extreme highs of mania and lows of depression.
Lithium: One of the oldest and most trusted options, lithium is effective for managing acute mania and preventing future episodes. It requires regular blood tests to monitor levels and check thyroid and kidney function.
Anticonvulsants: Originally for seizures, these are also highly effective. Divalproex sodium (Depakote) works well for acute mania and mixed states but carries risks of liver damage and birth defects. Lamotrigine (Lamictal) is particularly helpful for bipolar depression and preventing future depressive episodes. It’s started at a low dose and increased slowly to minimize the risk of a serious skin rash. Carbamazepine (Tegretol) is another option that requires blood monitoring.
Atypical Antipsychotics: Managing Acute Symptoms and Psychosis
Also called second-generation antipsychotics, these medications are vital for managing acute manic or mixed episodes and providing long-term stability. They are especially helpful when psychosis (hallucinations or delusions) is present. Common options include olanzapine (Zyprexa), risperidone (Risperdal), quetiapine (Seroquel), and aripiprazole (Abilify).
Your doctor might prescribe an atypical antipsychotic alone or with a mood stabilizer. Some are also FDA-approved for bipolar depression. However, common side effects include significant weight gain and metabolic changes, increasing the risk of diabetes and high cholesterol. Drowsiness and other side effects can also occur. Some of these medications carry black box warnings about increased suicidal thinking in young adults, highlighting the need for close monitoring.
The Role of Antidepressants: A Cautious Approach
Antidepressants are used with caution in bipolar disorder because they can trigger manic or hypomanic episodes. To reduce this risk, they are almost always prescribed alongside a mood stabilizer or antipsychotic. Using an antidepressant alone (monotherapy) is generally not recommended. Common types include SSRIs like fluoxetine (Prozac) and SNRIs like duloxetine (Cymbalta). This decision requires strict professional guidance.
Other Supportive Medications
Your doctor may use other medications for short-term symptom management.
Benzodiazepines like lorazepam (Ativan) can provide rapid, short-term relief from severe agitation, anxiety, or insomnia during acute episodes. However, because they carry a risk of dependence, abuse, and addiction, they are typically prescribed only for limited periods as a temporary bridge while primary medications take effect.
The Journey to Finding the Right Drug for Bipolar Disorder
Finding the right medication for bipolar disorder is a process, not a one-time fix. It requires patience, persistence, and honest communication with your healthcare team. Your doctor can make educated recommendations, but your individual response is unique.
The ‘Trial and Error’ Process
This process can feel frustrating, but it’s necessary. Some medications might work for mania but be too sedating; others might lift depression but cause side effects. A crucial point to remember is that it can take up to 8 weeks to see the full effects of a bipolar medication as it builds to therapeutic levels in your system.
Dose adjustments are a normal part of this process. Your doctor will likely start you on a low dose and gradually increase it to find the right balance of benefits and side effects. Keeping your doctor informed about how you’re feeling is key to finding the right treatment plan more quickly.
Common Side Effects and How to Manage Them
Side effects are a common challenge. The ones you might experience depend on the specific drug for bipolar disorder you’re taking. Common issues include:
- Nausea and digestive issues (often helped by taking meds with food)
- Weight gain (a concern with many atypical antipsychotics and some mood stabilizers)
- Drowsiness or sedation
- Tremors (especially with lithium)
- Hair loss or sexual problems
In rare cases, lamotrigine can cause a severe skin rash (Stevens-Johnson syndrome), which is why the dose is increased very slowly. Contact your doctor immediately if you develop any new rash.
Always report side effects to your doctor. They can often help you manage them, adjust your dose, or suggest an alternative. Never stop taking a medication abruptly without your doctor’s approval. Doing so can trigger withdrawal or a rapid return of severe mood episodes. For some medications like lithium, regular blood tests are essential for safety and effectiveness.
Tailoring Treatment: Bipolar I vs. Bipolar II Disorder
Treatment approaches differ based on your specific diagnosis.
Bipolar I Disorder: Treatment focuses on controlling severe manic episodes and preventing their return. Mood stabilizers (lithium, valproate) and atypical antipsychotics are the foundation, especially when psychosis is present.
Bipolar II Disorder: The primary struggle is often with prolonged, debilitating depressive episodes. Therefore, treatment emphasizes managing depression and preventing its recurrence. Lamotrigine is often a first-line choice due to its effectiveness for bipolar depression. Mood stabilizers and antipsychotics can also be used to manage hypomania.
Your doctor will create an individualized plan based on your diagnosis, symptom patterns, and medical history to give you the best chance at achieving lasting stability.
Long-Term Management and Special Considerations
Bipolar disorder is a lifelong condition that requires ongoing care. With consistent treatment, you can build a stable, fulfilling life. This is less about winning a single battle and more about tending to your health over the long term.
The Importance of Maintenance Therapy
Once an acute episode is controlled, maintenance therapy begins. Its goal is not to fix a crisis but to prevent the next one. Staying on your drug for bipolar disorder helps prevent relapse and reduces the frequency and severity of future mood episodes.
Many people feel better on medication and wonder if they still need it. This feeling of wellness is often because the medication is working. Stopping medication is a major risk factor for relapse. For most, treatment is a lifelong commitment—an investment in your health, relationships, and future.
Medications to Avoid or Use with Caution with a drug for bipolar disorder
Some substances can worsen bipolar disorder or interact dangerously with medications. Be cautious with:
- Antidepressants alone: Using them without a mood stabilizer can trigger mania.
- Stimulants: Medications for ADHD can worsen manic symptoms.
- Over-the-counter drugs and supplements: St. John’s Wort, SAMe, and others can trigger mania or interact with your prescriptions. NSAIDs like ibuprofen can increase lithium levels to toxic ranges.
- Alcohol and illicit drugs: These can destabilize your mood, interfere with medications, and worsen side effects.
Be completely honest with your healthcare provider about everything you take—prescriptions, supplements, alcohol, and other substances. At Addiction Helpline America, we specialize in connecting people with integrated programs that address both mental health and substance use without judgment.
Bipolar Medication and Pregnancy
Planning for pregnancy while managing bipolar disorder requires a careful balance of risks. Untreated bipolar disorder during pregnancy increases health risks for both mother and baby, including a higher chance of postpartum episodes.
However, some medications carry risks for a developing fetus:
- Valproate (Depakote) is contraindicated as it significantly increases the risk of birth defects and can lead to lower IQ scores.
- Lithium carries a low but increased risk of a specific heart defect and requires careful monitoring.
- Lamotrigine is often considered a relatively safer option for managing bipolar depression during pregnancy.
This is a complex decision that should be made with a specialist, such as a perinatal psychiatrist. They can help you create a plan that protects your mental health while minimizing risks to your baby.
A Holistic Approach: Medication and Beyond
While a drug for bipolar disorder is essential, it works best as part of a comprehensive plan. Therapy, healthy habits, and strong support systems are the other legs of the table that keep you stable.
The Vital Role of Psychotherapy
Talk therapy provides practical tools to manage the emotional and behavioral challenges of bipolar disorder. It works in partnership with medication.
- Cognitive Behavioral Therapy (CBT) helps you identify and change negative thought patterns.
- Psychoeducation teaches you about your condition, including triggers and early warning signs.
- Family-focused therapy improves communication and support within your family.
- Interpersonal and Social Rhythm Therapy (IPSRT) focuses on maintaining stable daily routines for sleep, meals, and social activity to support mood regulation.
Combining therapy with medication consistently leads to better long-term outcomes.
Diagnosis and Emerging Treatments
An accurate diagnosis from a psychiatrist is the first step. This involves a comprehensive mental health assessment, a physical exam to rule out other medical causes (like thyroid problems), and a detailed discussion of your symptom history. Mood charting—keeping a daily record of moods and sleep—can provide invaluable insight. For more information on symptoms and diagnosis, you can consult resources from the National Institute of Mental Health (NIMH).
The field of treatment is always evolving. For severe or treatment-resistant bipolar disorder, emerging options offer hope. Ketamine is being studied for rapid relief of severe bipolar depression. Electroconvulsive Therapy (ECT) is a safe and highly effective option when other treatments fail. Repetitive Transcranial Magnetic Stimulation (rTMS) is another non-invasive option for treatment-resistant depression.
Lifestyle and Support Systems
Your daily choices are powerful tools for managing bipolar disorder.
- Maintain a regular routine: Consistent sleep and wake times help regulate your body’s internal clock.
- Eat a healthy diet and exercise regularly: These improve mood and overall well-being.
- Avoid alcohol and illicit drugs: Substances can destabilize mood and interfere with medication.
- Find a support group: Connecting with others who understand provides comfort and practical advice.
- Continue mood charting: This helps you and your doctor track patterns and identify triggers.
At Addiction Helpline America, we connect you with programs that address all aspects of your health, including co-occurring substance use, to ensure you get complete support.
Frequently Asked Questions about Bipolar Disorder Drugs
Navigating bipolar disorder treatment brings up many questions. Here are answers to some of the most common concerns.
What is the most common drug prescribed for bipolar disorder?
There is no single “most common” drug, as treatment is highly individualized. However, mood stabilizers like lithium are considered foundational due to their long track record of success. Atypical antipsychotics are also prescribed very frequently for acute episodes and long-term maintenance.
Many people take more than one drug for bipolar disorder (combination therapy), as this is often more effective. The best medication is the one that works for you with manageable side effects.
How long do you have to be on bipolar medication?
Bipolar disorder is a chronic, lifelong condition, similar to diabetes or high blood pressure. For most people, this means medication is a long-term or lifelong commitment. The goal of this maintenance therapy is to prevent future mood episodes and maintain stability. Stopping medication, even when you feel well, is a major risk for relapse.
Can you treat bipolar disorder without medication?
While psychotherapy and healthy lifestyle changes are vital parts of treatment, medication is considered the cornerstone for stabilizing the extreme mood swings of bipolar disorder. Therapy and lifestyle habits are much more effective when built on the chemical stability that medication provides.
Attempting to manage bipolar disorder without medication is extremely challenging and often unsafe, as it increases the risk of severe episodes and hospitalization. The most effective and safest approach combines medication with therapy and healthy habits. If you have concerns about your medication, talk to your doctor about adjusting your plan rather than stopping treatment.
Conclusion: Taking the Next Step in Your Recovery
We’ve covered how a drug for bipolar disorder is a powerful tool for stabilizing mood swings. From mood stabilizers and antipsychotics to the cautious use of other medications, treatment is a personal journey. Finding the right medication can take patience—sometimes up to 8 weeks to see full effects—but the reward is a stable, clearer life.
Medication is just one piece of the puzzle. It works best with psychotherapy, a healthy lifestyle, and a strong support system. Hope and stability are achievable, and you don’t have to steer this path alone.
If you’re struggling with bipolar disorder, especially if substance use is also a concern, finding the right help can feel overwhelming. Addiction Helpline America provides free, confidential guidance to connect you with treatment programs that address both challenges together. Our team is here to listen and help you find the support you deserve.
Taking the next step is a brave move toward recovery. Whether for yourself or a loved one, reaching out is the start.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
24/7 Confidential Helpline for Bipolar Disorder Medication Support
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.