Why Specialized Care Matters for Depression Recovery
Depression recovery center services offer specialized, structured treatment for major depressive disorder, chronic depression, and co-occurring conditions. By providing multiple levels of care—from 24/7 residential to flexible outpatient programs—these centers combine evidence-based therapies, medication management, and holistic approaches to create a comprehensive path to wellness.
Key features include:
- Multiple levels of care: Inpatient, PHP, IOP, and outpatient programs.
- Evidence-based therapies: CBT, DBT, and EMDR.
- Advanced treatments: TMS, ketamine therapy, and medication management.
- Dual diagnosis support: Integrated care for co-occurring substance use or anxiety disorders.
- Accredited facilities: Joint Commission or CARF accreditation to ensure quality.
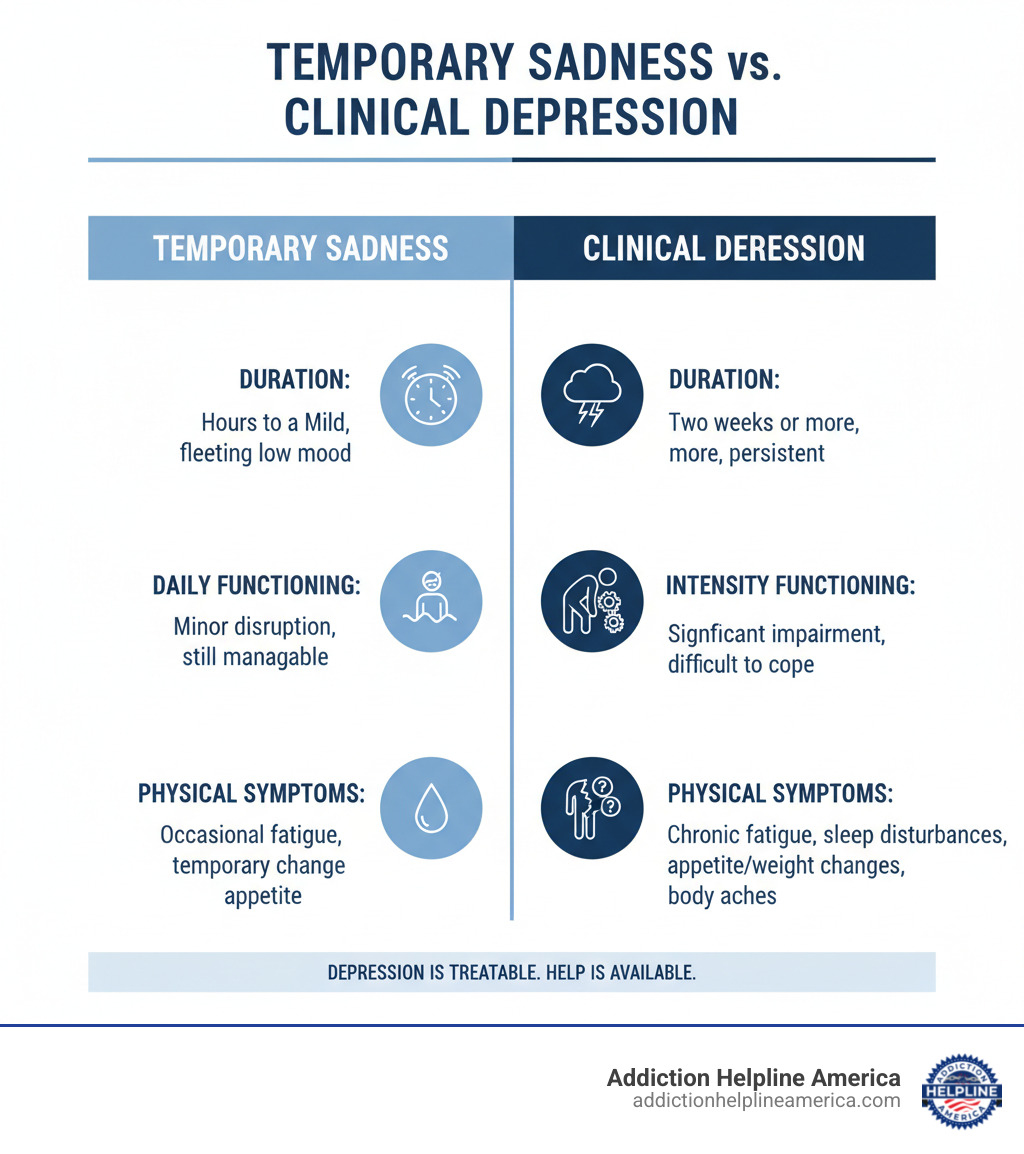
Depression is more than just sadness; it’s the leading cause of disability worldwide. Unlike temporary low moods, clinical depression persists for weeks and fundamentally changes how you think, feel, and function, making even simple tasks feel impossible.
The good news? Depression is highly treatable. With proper care, 70% to 90% of people respond well to treatment. Specialized depression recovery centers provide the structured support and medical expertise that make this recovery possible.
At Addiction Helpline America, we connect individuals to effective depression recovery centers nationwide. We help you steer insurance, treatment levels, and find the right fit for your unique situation. We understand that this first step is overwhelming, and we’re here to provide confidential guidance.
Depression recovery center word roundup:
- treatment for depression and anxiety
- therapist for depression and anxiety
- bipolar depression treatment
Understanding the Levels of Care for Depression
Depression recovery centers offer a clear pathway to healing with different levels of support designed to meet you where you are. Treatment often follows a step-down model: you start with intensive care when symptoms are severe and gradually move to less intensive programs as you build coping skills. This flexible approach ensures you always have the right amount of support.
You might begin in a 24/7 residential setting and later transition to a partial hospitalization program (day treatment), then an intensive outpatient program that fits your schedule, and finally to weekly therapy for maintenance. For more on these approaches, see our guide on inpatient vs outpatient care.
Here’s how the main levels of care compare:
| Level of Care | Intensity | Living Arrangements | Ideal Candidate |
|---|---|---|---|
| Inpatient/Residential | 24/7 medical/clinical supervision | Live at the facility | Severe depression, safety concerns, co-occurring disorders, need for stabilization |
| Partial Hospitalization (PHP) | 20+ hours/week, structured day treatment | Live at home or sober living | Stepping down from inpatient, needing high support but not 24/7 supervision |
| Intensive Outpatient (IOP) | 9-20 hours/week, structured therapy | Live at home | Balancing treatment with work/school, less severe symptoms, after inpatient |
| Standard Outpatient | Weekly sessions, flexible schedule | Live at home | Mild depression, maintenance, aftercare, strong support system |
Inpatient or Residential Treatment
When depression is severe, inpatient or residential treatment provides round-the-clock medical supervision in a safe, structured environment. By removing you from daily stressors, these programs allow you to focus entirely on healing. 24/7 monitoring is crucial for individuals with thoughts of self-harm or co-occurring substance use disorders. The primary goal is stabilization through intensive therapy, medication management, and holistic activities. For those needing extended support for co-occurring issues, long-term residential rehab can be beneficial.
Partial Hospitalization Programs (PHP)
Partial Hospitalization Programs (PHPs) offer intensive treatment without living at the facility. You attend structured therapy for 20+ hours per week but return home each evening. This model is ideal for those stepping down from residential care or for individuals who need daily intervention but not 24/7 supervision. A PHP helps bridge the gap between a protected inpatient environment and independent living.
Intensive Outpatient Programs (IOP)
Intensive Outpatient Programs (IOPs) provide structured therapy for 9 to 20 hours per week, offering flexibility to balance treatment with work, school, or family. Sessions often include individual, group, and family therapy and may be scheduled on evenings or weekends. IOPs are well-suited for moderate depression or as a step-down from a higher level of care, allowing you to apply new skills in your daily life while still receiving robust support.
Standard Outpatient Programs
Standard outpatient care typically involves weekly sessions with a therapist and regular medication management check-ins. This level of care is effective for mild depression or for maintaining progress after completing a more intensive program. It serves as the maintenance phase of recovery, providing regular tune-ups to reinforce skills and address challenges as they arise. Learn more about this option on our page about outpatient treatment.
At Addiction Helpline America, we can help you determine the right level of care and connect you with a depression recovery center that meets your needs.
Key Therapies and Treatments in a Depression Recovery Center
A quality depression recovery center creates individualized treatment plans that address your unique symptoms and goals. The best centers treat the whole person by combining evidence-based psychotherapy, medication management, and holistic approaches.
Evidence-Based Psychotherapy
Psychotherapy, or “talk therapy,” is the foundation of depression treatment. At a depression recovery center, these therapies are backed by research.
- Cognitive Behavioral Therapy (CBT) helps you identify, challenge, and replace the negative thought patterns that fuel depression. It provides practical tools for long-term use.
- Dialectical Behavior Therapy (DBT) is effective for managing intense emotions and self-harm urges. It teaches skills in mindfulness, emotion regulation, interpersonal effectiveness, and distress tolerance.
- Eye Movement Desensitization and Reprocessing (EMDR) is helpful for depression linked to trauma. Through guided eye movements, EMDR helps the brain process traumatic memories and reduce their emotional impact.
These are just a few of the many types of treatment programs available.
Medication and Interventional Psychiatry
Medication is often an essential part of recovery, especially for moderate to severe depression. Antidepressants work by balancing brain chemicals that affect mood. The most common are SSRIs (Selective Serotonin Reuptake Inhibitors), which research shows are highly effective. Finding the right medication and dosage may take time under a doctor’s supervision.
For treatment-resistant depression (TRD), where traditional antidepressants fail, interventional psychiatry offers advanced options:
- Transcranial Magnetic Stimulation (TMS) is a non-invasive procedure that uses magnetic fields to stimulate mood-regulating nerve cells in the brain. It’s done in an outpatient setting without anesthesia.
- Ketamine therapy offers rapid relief for severe depression, often within hours or days. Administered as an IV or nasal spray (esketamine) in a clinical setting, it acts on different brain receptors than traditional antidepressants.
- Electroconvulsive Therapy (ECT) is a safe and highly effective modern treatment for severe depression when other methods haven’t worked. It is performed under general anesthesia.
The Importance of Treating Co-Occurring Disorders
Depression often co-exists with other mental health conditions or substance use disorders, known as a dual diagnosis. About 20.4 million American adults experienced a co-occurring disorder last year.
- Depression and substance use can create a vicious cycle of self-medication, where using substances to numb pain ultimately worsens depression.
- Depression and anxiety frequently appear together, creating a combination of deep sadness and racing, anxious thoughts.
Integrated treatment that addresses all conditions simultaneously is far more effective. A specialized depression recovery center understands this complexity and builds comprehensive treatment plans. Learn more from our resources on co-occurring disorders. At Addiction Helpline America, we help you find quality, integrated care.
How to Choose the Right Depression Recovery Center for You
Finding the right depression recovery center is about finding the place where you feel safe, understood, and equipped to heal. While the decision can feel overwhelming, focusing on these key factors can help you move forward with confidence.
1. Verify Accreditation and Licensing
First, ensure the center meets quality and safety standards. Look for accreditation from respected organizations like The Joint Commission (the gold standard in healthcare) or CARF (Commission on Accreditation of Rehabilitation Facilities). These signify that a center has met rigorous standards for patient care and effectiveness. Also, confirm the center has state licensing, which is a legal requirement to operate.
2. Assess Treatment Philosophy and Specializations
Find a center whose approach matches your needs. A quality center will always create an individualized care plan. Consider whether you prefer a program focused on evidence-based therapies like CBT and DBT, or one that blends these with holistic practices like yoga and art therapy. If you have a history of trauma, look for a center that is trauma-informed. Also, consider specializations for groups like executives, LGBTQ+ individuals, or veterans, as they may better understand your unique challenges.
3. Evaluate Amenities and Environment
The physical environment contributes to healing. Decide what setting is best for you. Some people prefer a luxury setting with private rooms and spa-like services, while others are comfortable in a simpler environment. Executive programs may offer private accommodations and limited tech access for professionals. Look for amenities that support recovery, such as fitness centers, yoga studios, and nutritional support. Also, inquire about tech-friendly policies if staying connected to family is a priority.
4. Inquire About Aftercare and Relapse Prevention
Recovery is an ongoing process. A quality depression recovery center will create a continuing care plan with you before you leave, outlining ongoing therapy, medication management, and local resources. Ask about alumni programs, which provide a community of support after treatment. Connections to support groups like those offered by NAMI or the Depression and Bipolar Support Alliance are also valuable. The NIMH offers helpful resources that many centers use in aftercare planning.
At Addiction Helpline America, we help you consider all these factors. We’ll ask the right questions and connect you with centers that fit your needs, so you don’t have to do it alone.
Navigating Costs, Insurance, and Time Off for Treatment
The practical questions of cost and time off work are often major barriers to seeking treatment. Fortunately, care is more accessible than you might think, and legal protections are in place to help you get the help you need.
Finding a Depression Recovery Center That Accepts Your Insurance
Under the Affordable Care Act, mental health treatment is an essential health benefit, meaning your insurance plan likely covers depression recovery center services. Understanding in-network versus out-of-network providers is key to managing costs; in-network centers have negotiated rates with your insurer, resulting in lower out-of-pocket expenses for you.
The most important step is to verify your coverage. Call your insurance provider to ask about your deductible, co-pays, and any pre-authorization requirements for mental health services. Navigating this can be confusing, which is why Addiction Helpline America offers to verify your insurance benefits for you, confidentially and free of charge.
Payment Options and Financial Assistance
If you have out-of-pocket costs or no insurance, you still have options. Many centers offer private pay rates, and some non-profits provide sliding scale fees based on your income. Don’t hesitate to ask about financial assistance. Another option is healthcare financing through companies like CareCredit, which offer payment plans for medical expenses. Our team can help you explore these financing options.
Taking Time Off Work for Treatment
Federal law protects employees who need time off for mental health care. The Family and Medical Leave Act (FMLA) allows eligible employees to take up to 12 weeks of unpaid, job-protected leave for serious health conditions, including clinical depression. Your employer must also maintain your health benefits during this leave.
To qualify, you generally must have worked for your employer (with 50+ employees) for at least 12 months and 1,250 hours. Speak with your Human Resources department to understand the process; you only need to state that you require medical leave for a serious health condition. The Department of Labor provides detailed information on FMLA eligibility.
At Addiction Helpline America, we help people steer these practical challenges every day. Our guidance is free, confidential, and designed to remove barriers to recovery.
Frequently Asked Questions about Depression Recovery
Is depression a highly treatable condition?
Yes, absolutely. Depression is highly treatable, with 70% to 90% of people responding well to treatment. The most effective approaches often combine psychotherapy (like CBT or DBT) with medication. With consistent, professional care from a depression recovery center, recovery is not only possible but probable.
What is the difference between major depression and chronic depression?
The main difference is severity and duration.
- Major Depressive Disorder (MDD) involves severe symptoms that significantly impair daily functioning for at least two weeks.
- Chronic depression (Persistent Depressive Disorder or dysthymia) involves less severe but longer-lasting symptoms, present for at least two years in adults. As the National Institute of Mental Health explains, its persistence can significantly impact quality of life.
Both forms are serious and respond well to professional treatment.
How do I know if a treatment center is reputable?
Choosing a trustworthy depression recovery center is crucial. Here are key indicators of a reputable facility:
- Accreditation and Licensing: Look for accreditation from The Joint Commission or CARF and ensure the center is licensed by the state.
- Evidence-Based Therapies: The program should be founded on scientifically proven approaches like CBT, DBT, and EMDR.
- Qualified Staff: The clinical team (psychiatrists, therapists) should be licensed, experienced, and qualified.
- Independent Reviews: Check unbiased platforms for feedback from former patients and their families.
- Transparency: A reputable center will be open about its programs, costs, and policies, and will answer your questions clearly.
At Addiction Helpline America, we vet treatment centers to ensure they meet these standards, helping you find quality care you can trust.
Conclusion: Take the First Step on Your Path to Healing
If you’re reading this, you’ve already taken a courageous step by learning about depression recovery center options. We want you to know that recovery is possible. Research shows that 70% to 90% of people who seek treatment for depression experience significant improvement. You are not alone in this struggle, and healing is within reach.
Depression can make you feel isolated, but millions have walked this path and found their way back to a life worth living, often through the structured support of a specialized depression recovery center. The right combination of therapy, medication, and holistic care makes all the difference.
At Addiction Helpline America, we specialize in connecting people to effective treatment. The process of finding help—navigating insurance, choosing a program, asking the right questions—can be overwhelming. That’s why we’re here. Our team provides free, confidential, and personalized guidance to help you find a program that fits your unique situation.
You don’t have to carry this weight by yourself. Find professional help today and start your journey toward lasting healing. Your path to recovery begins with a single call, and we’re here to help you take that step.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
How Addiction Helpline America Supports Your Depression Recovery
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.