
Understanding When Inpatient Care for Depression Becomes Necessary
Inpatient centers for depression offer 24/7 medical and therapeutic care in a structured setting for individuals with severe depressive symptoms. These facilities are designed for people who:
- Are at risk of harming themselves or others
- Cannot function in daily life (work, self-care, relationships)
- Have not improved with outpatient treatment
- Need crisis stabilization and constant monitoring
- Struggle with co-occurring conditions like anxiety or substance use
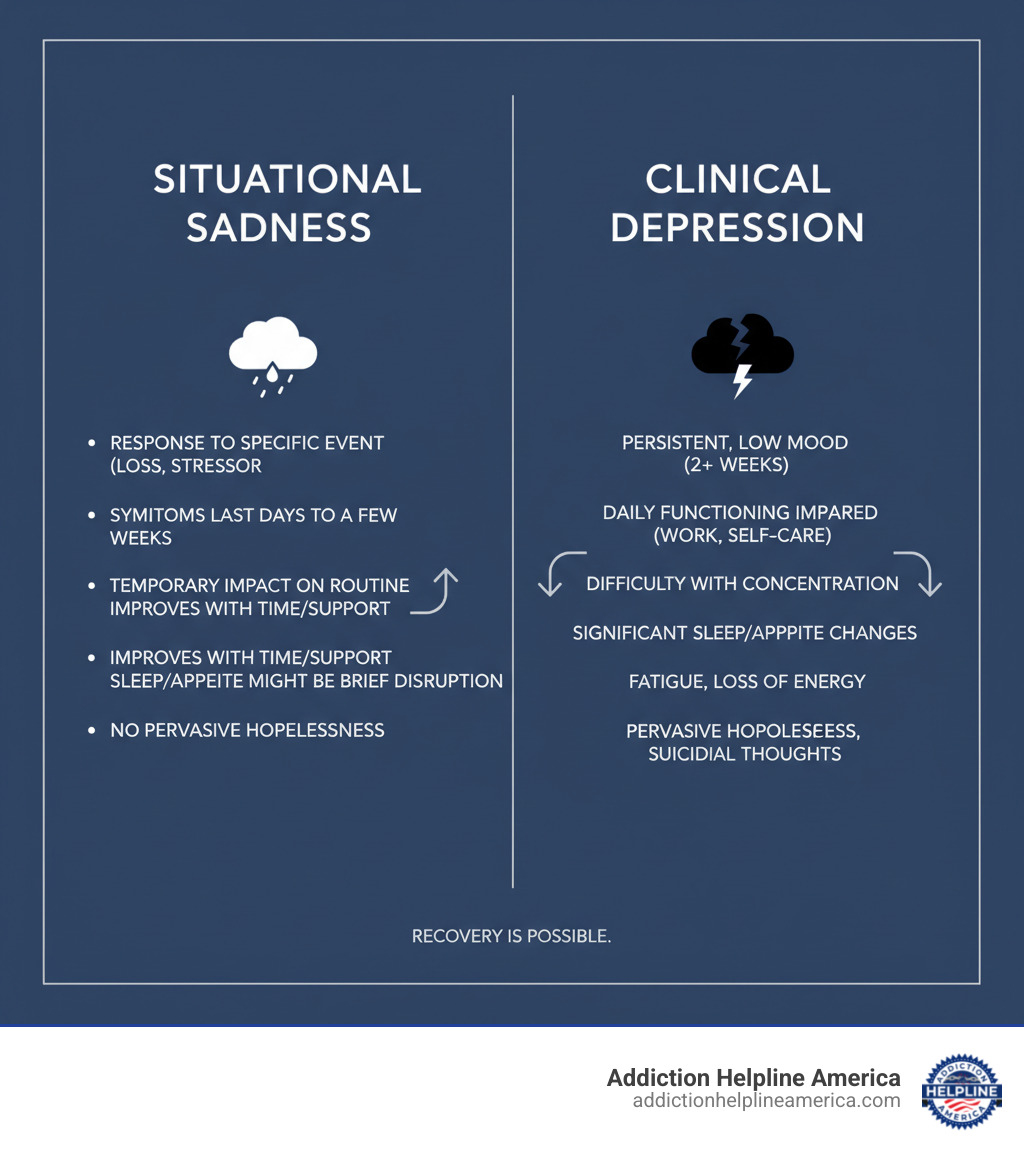
Depression is the leading cause of disability worldwide. While many experience temporary sadness, clinical depression involves persistent symptoms that impair daily functioning. The good news? Recovery is possible, and inpatient treatment offers intensive care for those who need it most.
This guide explains what inpatient depression treatment involves, when it’s necessary, and how to find the right center for your needs.
At Addiction Helpline America, we connect individuals with treatment resources for mental health and co-occurring disorders, including inpatient centers for depression. We understand the urgency that comes with severe depression and are here to provide clear, compassionate guidance.
Glossary for inpatient centers for depression:
What is Inpatient Treatment for Depression?
When depression becomes severe enough to threaten your safety or make daily life impossible, inpatient centers for depression offer the most intensive level of care. It is a protective environment where you can focus entirely on healing, away from daily pressures and triggers.
Unlike outpatient care, where you live at home, inpatient treatment means you stay at a specialized facility full-time, surrounded by medical professionals and support staff. Every part of your day is intentionally planned to support your healing, from therapy sessions and group activities to medical care. This immersive, structured environment provides crisis stabilization and intensive treatment when it’s needed most.
This level of care is necessary when outpatient therapy and medication haven’t provided relief, you’re experiencing suicidal thoughts, or you’re dealing with co-occurring disorders like anxiety or substance use. According to the WHO fact sheet on depression, intensive treatment can make the difference between crisis and recovery.
Here’s how different levels of mental health care compare:
| Level of Care | Description |
|---|---|
| Inpatient (Hospitalization) | You live at the facility 24/7, receiving constant medical supervision and intensive therapy. Best for severe symptoms and safety concerns. |
| Partial Hospitalization Program (PHP) | You spend 20+ hours per week at the facility but return home each night. A step-down from inpatient care. |
| Intensive Outpatient Program (IOP) | You attend 9-20 hours of treatment weekly while living at home. More structured than standard outpatient care. |
| Outpatient Care | You attend scheduled therapy or medication appointments, typically weekly or bi-weekly, while living at home. |
Signs You Might Need Inpatient Care
Recognizing when you need immediate help isn’t always easy, as depression can distort your perspective. If you’re wondering whether you need help, that question itself deserves attention.

Persistent feelings of hopelessness: This is more than a bad week; it’s a feeling of being trapped in darkness for weeks or months, with no hope for improvement.
Inability to function in daily life: Basic self-care, like getting out of bed or showering, feels impossible. You may be missing work or school and letting relationships suffer.
Significant changes in sleep or appetite: This includes severe insomnia, sleeping excessively, or dramatic weight changes from not eating or compulsive eating.
Social withdrawal: You’ve completely isolated yourself from friends and family, which can deepen the depressive spiral.
Increased substance use: Using alcohol, drugs, or misusing medication to numb emotional pain indicates a need for integrated treatment for co-occurring disorders.
Risk to self or others: This is the clearest signal. If you’re having suicidal thoughts or making plans to harm yourself, seek help immediately. The 988 Suicide & Crisis Line is available 24/7, and inpatient centers for depression are equipped to keep you safe.
When outpatient treatment hasn’t worked, it’s not a failure. It’s a sign that you need a higher level of care. Inpatient treatment provides the intensive, round-the-clock support that can break through when other approaches haven’t been enough.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
The Treatment Experience at Inpatient Centers for Depression
You’re entering a place designed entirely around your healing. What makes inpatient treatment so powerful is the multidisciplinary treatment team surrounding you. This group of specialists works together on your behalf and typically includes doctors, psychiatrists, therapists, nurses, and case managers.
These professionals meet regularly to discuss your progress and create your care plan with you, not for you. Your individualized recovery plan reflects your unique story, struggles, and goals. This holistic approach supports your mental, emotional, and physical well-being.

Therapies and Holistic Care in an Inpatient Center for Depression
Therapeutic work at inpatient centers for depression goes beyond traditional talk therapy. You’ll engage with evidence-based therapies in both individual and group settings.
Cognitive Behavioral Therapy (CBT) helps you recognize and challenge the negative thought patterns that fuel depression, replacing them with more balanced perspectives.
Dialectical Behavior Therapy (DBT) teaches concrete skills for managing intense emotions, including mindfulness, distress tolerance, and emotion regulation.
Group therapy breaks through the isolation of depression. Sharing experiences with others who understand creates a powerful sense of connection and mutual support.
Family therapy can be included to improve communication and build a stronger support network for when you return home.
Many centers also offer experiential therapies like art, music, or yoga to help you connect your mind and body. The holistic approach also addresses overall wellness, including nutrition, fitness, and reestablishing routines for personal care.
Addressing Co-Occurring Disorders
Depression rarely travels alone. Many people entering inpatient centers for depression also deal with anxiety, bipolar disorder, or substance use issues. This is known as a dual diagnosis or co-occurring disorder.
Quality inpatient programs use an integrated treatment model, where your entire plan considers how your conditions interact. This coordinated approach is far more effective than treating each issue in isolation.
- Anxiety disorders are often treated with specific strategies for managing worry and fear.
- Bipolar disorder treatment focuses on mood stabilization and recognizing warning signs of mood shifts.
- Substance use disorders require special attention. For some, medical detox—a medically supervised withdrawal process—is the first step to provide a stable foundation for therapy.
Medication Management and Treatment Duration
Medication is often an important part of recovery. A psychiatrist oversees this aspect of your care, evaluating whether medications like antidepressants or mood stabilizers might help. The inpatient setting allows for close monitoring and adjustment to find the right medication and dosage for you, which is safer and often faster than in outpatient care.
The typical duration of stay varies. Some people need short-term stabilization lasting a few days or weeks to manage an acute crisis. Others with chronic depression or severe co-occurring disorders may benefit from long-term programs lasting 30, 60, or 90 days. Your treatment team will work with you to determine the right length of stay to ensure you are stable and equipped with effective coping skills. For more information about chronic depression, visit the NIMH resource on depression.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Your Journey Through Treatment: Admission, Progress, and Aftercare
When you arrive at an inpatient center for depression, you step into a structured healing environment. The predictable rhythm of the day allows you to focus entirely on getting better, free from the stress of daily life.

Your days will have a natural flow, including individual and group therapy, meals, recreational activities like yoga, and time for reflection. Throughout your stay, you and your team will focus on goal setting and tracking your progress. Many centers use measurement-based care to regularly check on your symptoms and well-being, ensuring your treatment evolves with you.
The Admission and Discharge Process
Getting into treatment should be a straightforward process.
- Assessment and Insurance: You’ll have a thorough initial assessment to discuss your mental and physical health. At the same time, the admissions team will help with insurance verification to clarify your coverage and costs.
- Intake: The intake process involves paperwork and getting oriented to the facility, its schedule, and its staff. You’ll be advised on what to bring, which usually includes comfortable clothing and personal items.
- Discharge Planning: Your team starts planning for your transition home from day one. In collaboration with you and your family, they develop a continuing care plan that outlines your next steps, such as outpatient therapy, medication management, and support groups. The goal is to provide a clear roadmap for your ongoing recovery.
Developing Skills for Lasting Wellness
Inpatient centers for depression don’t just help you feel better temporarily; they teach you how to stay better. The skills you develop become tools you’ll use for the rest of your life.
You’ll learn practical coping mechanisms and stress management techniques to handle difficult emotions and triggers. A major focus is on relapse prevention, where you learn to recognize your personal warning signs and create a proactive plan for addressing them.
Building a support system with peers and family is a natural part of treatment. After you leave, aftercare programs become your next chapter. This continuing care might include outpatient therapy, support groups, or for those with co-occurring substance use, supportive living environments. Some centers also have alumni groups for ongoing peer connection. At Addiction Helpline America, we believe in helping you build a life you genuinely want to live.
How to Choose and Afford an Inpatient Depression Center
Choosing a facility that fits your needs is a critical step in your recovery. Here’s what to look for and how to make treatment affordable.
When evaluating facilities, check for accreditation from organizations like CARF or the Joint Commission, which indicates high standards for quality and safety. The credentials and experience of the staff also matter; look for licensed professionals who specialize in treating depression. Finally, ensure the center’s treatment philosophy—whether it’s clinical, holistic, or a blend—aligns with what feels right for you.
Here are essential questions to ask a potential inpatient center for depression:
- What is your specific approach to treating depression?
- Are your treatment methods evidence-based?
- What are the credentials of your clinical staff?
- How do you involve family members in treatment?
- What does a typical day look like, and what is the average length of stay?
- How do you provide discharge planning and aftercare support?
- What accreditations do you hold?
The cost of treatment varies, but understanding your insurance coverage and payment options can make it accessible. The Mental Health Parity and Addiction Equity Act (MHPAEA) and the Affordable Care Act (ACA) require most insurance plans to cover mental health treatment as an essential health benefit. You can learn more about mental health & substance abuse coverage through the ACA.
Contact your insurance provider to verify your specific coverage, including in-network vs. out-of-network benefits, deductibles, and copays. Many treatment centers have specialists who can help you with this process. If you lack insurance, many centers offer payment options like self-pay plans or sliding scale fees based on income.
If you’re employed, the Family and Medical Leave Act (FMLA) may provide up to 12 weeks of unpaid, job-protected leave for serious health conditions like depression, allowing you to focus on recovery without fear of losing your job. You can look online for more information on FMLA to understand your rights.
Finding the Right Inpatient Center for Depression for Your Needs
Not all inpatient centers for depression are the same. Many offer specialized programs for specific populations, such as:
- Adolescents: Programs that address the unique developmental and social pressures of young people.
- Seniors: Programs that consider the health concerns and life transitions common in older adults.
- First responders and veterans: Trauma-focused programs that create a community of peers with shared experiences.
- LGBTQ+ individuals: Affirming care environments where you can be your authentic self without fear of judgment.
Consulting with a therapist or doctor who knows your history is a great first step. They can provide valuable recommendations custom to your clinical needs.
At Addiction Helpline America, we specialize in connecting people with the right treatment. Our team provides free, confidential guidance to help you find a facility that matches your needs, accepts your insurance, and offers the specialized care you deserve. We’re here to answer your questions and support you through every step of finding the right center.
Frequently Asked Questions about Inpatient Depression Treatment
Considering inpatient treatment brings up many questions. We’re here to answer the most common ones clearly and honestly.
Can I be forced to go to an inpatient center?
Most people enter inpatient centers for depression voluntarily. However, in a crisis, someone can be admitted involuntarily. Involuntary commitment is a legal process that occurs when a person is deemed a danger to themselves or others or is gravely disabled (unable to provide for their basic needs) due to a mental illness. State-specific laws exist to protect people during their most vulnerable moments. While it can feel frightening, it is a caring act of last resort to ensure safety and stabilization.
What is a typical day like in an inpatient program?
A typical day is highly structured to create a peaceful and supportive healing environment. Your schedule will include:
- Morning routines like meditation or goal-setting.
- Individual and group therapy sessions focused on evidence-based practices like CBT.
- Scheduled meals to help reestablish routine and proper nutrition.
- Recreational or holistic activities such as yoga, art therapy, or gym time.
- Evening reflection or support groups to process the day.
This structure removes the burden of decision-making, allowing you to focus entirely on recovery. Staff are available 24/7 for medical and emotional support.
Will my insurance cover inpatient treatment for depression?
Yes, most insurance plans are required to cover inpatient mental health care as an essential health benefit under the ACA. However, coverage details vary. You will likely have deductibles and copays, and your out-of-pocket cost depends on your plan.
We recommend you verify coverage with your provider to understand your benefits for in-network vs. out-of-network facilities. Most inpatient centers for depression require pre-authorization from your insurance company, and their admissions team can help you with this process. The Mental Health Parity and Addiction Equity Act (MHPAEA) ensures that insurance companies cannot impose stricter limits on mental health benefits than they do on medical ones. For more information, visit the official resource on mental health & substance abuse coverage.
If you don’t have insurance, many facilities offer payment plans or sliding scale fees. At Addiction Helpline America, we can help you understand your options.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Take the First Step Towards Healing
Living with severe depression is an immense burden, but you don’t have to carry it alone. Inpatient centers for depression provide a safe space where you can set that burden down and begin to heal. This isn’t just about managing symptoms—it’s about building a foundation for the life you deserve.
These centers offer hope for a brighter future through comprehensive care and 24/7 support. You will learn effective coping skills, connect with others who understand, and find that recovery is within your reach. We’ve seen countless individuals who felt hopeless reconnect with joy and build thriving lives. This is what recovery looks like with the proper support.
Taking the first step can feel overwhelming, but every person who has found healing had to take that same step. At Addiction Helpline America, we’re here to make it easier. We provide free, confidential guidance to help you understand your options and connect with the right treatment center from our nationwide network.
Your journey to healing doesn’t require you to have it all figured out—it just requires you to reach out. Explore different types of treatment programs to learn more, or contact us directly for immediate, compassionate guidance. The life you’re hoping for is possible, and it starts now.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Overview of Inpatient Depression Treatment Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.















