
When a Joyful Time Feels Overwhelming: Understanding Treatment Options
CBT for postpartum depression is an evidence-based, short-term therapy (typically 12-16 sessions) that helps new mothers identify and change negative thought patterns, improve mood through behavioral activation, and develop practical coping skills to manage the challenges of early motherhood.
Quick Answer: What You Need to Know About CBT for Postpartum Depression
- What it is: A structured therapy that connects thoughts, feelings, and behaviors to reduce depression symptoms
- How effective: Medium to large effect in reducing symptoms compared to usual care alone
- Duration: Usually 12-16 sessions
- Key techniques: Identifying negative thoughts, behavioral activation, problem-solving, relaxation strategies
- Delivery options: Individual therapy, group sessions, or online formats with professional guidance
- Who benefits: Mothers experiencing PPD symptoms lasting more than 2 weeks
- Evidence: Research shows significantly lower depression and anxiety symptoms, with benefits lasting 6+ months
Postpartum depression affects 1 in 5 to 1 in 6 mothers after childbirth. It’s not a weakness but a real medical condition that responds well to treatment. Many new mothers feel intense pressure to be happy, but the reality of PPD can feel isolating and shameful, as one mother shared on the Giving Voice to Depression podcast: “I wanted to be pregnant—then I just wanted to die.”
Depression distorts how we see everything, making challenges feel impossible and whispering lies about our worth. CBT breaks that silence with practical tools. It teaches you to recognize when depression is clouding your thoughts, take small actions to lift your mood, and manage stress while caring for your baby. Research shows mothers who receive CBT have significant reductions in depression and anxiety symptoms, with improvements lasting well beyond treatment.
At Addiction Helpline America, we understand that seeking help for postpartum depression is overwhelming when you’re exhausted. Our team connects mothers with qualified mental health professionals specializing in CBT for postpartum depression. We’re here 24/7 to help you find resources and guide you toward recovery—because you and your baby deserve support.

Know your cbt for postpartum depression terms:
Understanding Postpartum Depression: Symptoms, Risks, and What It’s Not
Becoming a parent changes everything. Alongside the joy, you’re navigating sleep deprivation, hormonal shifts, and a transformed identity. For many, these challenges go beyond normal adjustment. Postpartum depression (PPD) is a genuine mood disorder that can begin during pregnancy or anytime within the first year after delivery. It’s a medical condition, not a sign of weakness.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
PPD affects 1 in 5 to 1 in 6 new mothers, meaning millions of mothers across states like Alabama, California, Florida, New York, and Texas face this challenge annually. Without treatment, PPD can affect the baby’s development and the mother-infant bond. The good news is that effective treatments like CBT for postpartum depression help mothers recover. For more general information on PPD, you can visit MedlinePlus.
Common Symptoms of PPD
PPD symptoms vary, but if you experience several of the following for more than two weeks, it’s time to seek help:
- Persistent sadness, emptiness, or loss of interest in activities you once enjoyed.
- Difficulty bonding with your baby or feeling disconnected.
- Withdrawing from your partner, family, and friends.
- Significant changes in appetite or sleep patterns (insomnia or sleeping too much).
- Intense irritability, anger, or severe mood swings.
- Feelings of worthlessness, shame, or excessive guilt about being a “bad” mother.
- Difficulty concentrating, remembering things, or making decisions.
- Thoughts of harming yourself or your baby, which require immediate professional help. If you have these thoughts, call 988 (the Suicide and Crisis Lifeline) or contact a healthcare provider right away.
“Baby Blues” vs. Postpartum Depression
It’s crucial to know the difference between the “baby blues” and PPD.
- Baby Blues: Affects up to 80% of new mothers. Involves mild sadness, weepiness, and anxiety that starts 2-3 days after birth and resolves on its own within two weeks. It’s uncomfortable but doesn’t significantly interfere with daily life and doesn’t require treatment.
- Postpartum Depression: A more severe and persistent condition. It can begin anytime in the first year, with symptoms lasting for weeks or months if untreated. PPD significantly interferes with your ability to care for yourself and your baby and always requires professional intervention for recovery.
Key Risk Factors for Developing PPD
While any new mother can develop PPD, certain factors increase the risk. Recognizing them can help in seeking early support.
- History of depression or anxiety: A personal or family history is one of the strongest predictors.
- Stressful life events: Financial difficulties, job loss, or other major life changes.
- Lack of social support: Feeling isolated or lacking practical and emotional help from a partner, family, or friends.
- Complications during pregnancy or birth: A traumatic birth experience, premature delivery, or a baby with health issues.
- Relationship difficulties: Conflict with a partner or family members.
- Biological factors: The rapid drop in hormones after childbirth and chronic sleep deprivation.
- Unrealistic expectations about motherhood: The pressure to be a “perfect” mother clashing with the messy reality of parenthood.

Understanding these risk factors isn’t about blame; it’s about recognizing when extra support is needed.
How Does CBT for Postpartum Depression Work?
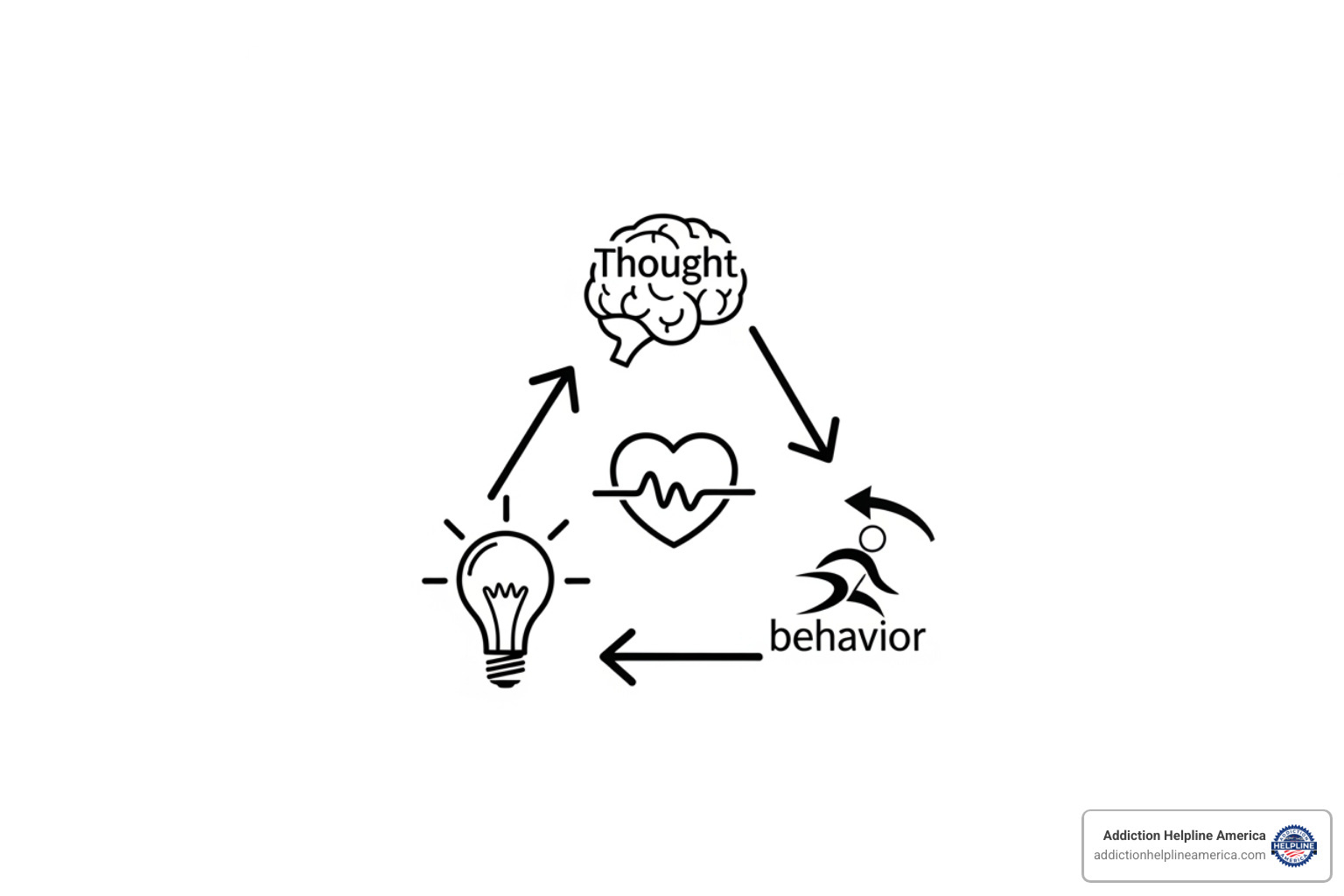
Cognitive Behavioral Therapy (CBT) is a powerful, evidence-based therapy for PPD. It focuses on the connection between your thoughts, emotions, and actions. When you have PPD, you might have distorted thoughts like, “I’m failing as a mother,” which trigger feelings of guilt and sadness, leading you to withdraw from others.
CBT for postpartum depression breaks this cycle by teaching you practical skills to recognize these patterns and respond differently. The therapy is typically short-term (12-16 sessions) and goal-oriented, so you’re actively learning coping strategies to use in your daily life.
The CBT Model for PPD
Your therapist will help you understand how depression distorts your thoughts, feelings, and behaviors. The model involves:
- Identifying negative thought patterns: Learning to catch automatic, self-critical thoughts like “You should be grateful, not miserable” that depression fuels.
- Challenging unhelpful beliefs: Questioning unrealistic expectations about motherhood, such as the belief that “good mothers never feel frustrated.”
- Changing behaviors to improve mood: Using a technique called behavioral activation to gradually re-engage in pleasant or meaningful activities, which counteracts the withdrawal that worsens depression.
- Increasing maternal self-efficacy: Building confidence by learning practical problem-solving skills for real challenges like sleep deprivation or asking for help.
What Specific Techniques Are Used in CBT for PPD?
CBT uses several practical tools to address the unique challenges of PPD:
- Cognitive restructuring: Learning to examine the evidence for negative thoughts and replace harsh self-criticism with more realistic, compassionate perspectives.
- Behavioral activation: Intentionally scheduling small, positive activities (like a 10-minute walk or listening to music) to improve your mood, even when you lack motivation. Action often comes before motivation.
- Problem-solving skills: Breaking down overwhelming challenges into manageable steps to find practical solutions for issues like getting more sleep or managing household tasks.
- Scheduling pleasant activities: Making time for small moments of enjoyment to balance out stress and remind you that you are more than just a mother.
- Relaxation techniques: Using tools like deep breathing exercises or progressive muscle relaxation to manage the physical symptoms of anxiety and stress.
- Communication skills training: Practicing how to clearly express your needs, set boundaries, and ask for help from your partner and family to build a strong support system.
These techniques empower you to become your own therapist, equipped with tools that last long after your sessions end. At Addiction Helpline America, we can help you find a therapist trained in CBT for postpartum depression to guide you through this process.
Evidence and Formats for CBT Treatment
When you’re struggling, you need a treatment that works. CBT for postpartum depression is a first-line therapy recommended for mild to moderate PPD because it is backed by decades of strong research.
Evidence Supporting CBT for Postpartum Depression
Research consistently shows that mothers who receive CBT for postpartum depression experience significant improvements.
- Studies show a medium-to-large effect size in reducing depressive symptoms compared to usual care alone.
- The benefits are long-lasting, with improvements holding steady six months or more after treatment ends.
- Mothers who complete CBT are less likely to experience future depressive episodes.
- The therapy not only reduces depression and anxiety but also increases maternal confidence, psychological flexibility, and self-compassion.
For more information on the effectiveness of CBT, you can refer to relevant research on CBT for PPD. To explore more about mental health treatment options, please visit our mental health services page.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Different Ways CBT is Delivered
A major advantage of CBT is its flexibility. It can be delivered in multiple formats to fit the life of a new mother.
- Individual therapy: Traditional one-on-one sessions with a therapist for a highly personalized approach.
- Group therapy: A supportive environment to connect with other mothers, reducing isolation and learning from shared experiences.
- Online or internet-based CBT: A flexible option that delivers therapy through digital platforms, ideal for overcoming barriers like childcare or transportation. It is most effective when it includes professional guidance.
- Blended therapy: A combination of online modules and face-to-face or video sessions with a therapist.
- In-home CBT: Therapy sessions conducted in the comfort of your home, removing the need to travel.

Benefits and Limitations of CBT
Understanding the pros and cons of CBT for postpartum depression helps set realistic expectations.
Benefits: CBT is highly effective, skill-building, and empowering. Its short-term nature (typically 12-16 sessions) allows for relatively quick progress. You learn lifelong tools to manage not just depression but also anxiety, becoming an active participant in your recovery.
Limitations: CBT requires motivation and active practice between sessions, which can be difficult when exhausted. For severe PPD or postpartum psychosis, it may need to be combined with medication or more intensive care. Finding a trained perinatal therapist can also be a barrier, and it’s a process, not a quick fix.
Accessing Treatment and Other Support
You don’t have to steer postpartum depression alone. Recognizing you need help and knowing where to find it are powerful first steps. Many mothers wait too long, hoping it will get better on its own, but PPD rarely resolves without support.
If your symptoms have lasted more than two weeks, it’s time to talk to someone. This is especially true if you’re feeling worse, struggling to care for yourself or your baby, or having any thoughts of harming yourself or your child. These are emergencies that require immediate professional help.
For additional support groups and resources, visit our resources page.
Other Support Options for PPD
While CBT for postpartum depression is highly effective, it works best within a comprehensive support system. Consider these additional options:
- Support groups: Connect with other mothers online or in person to reduce feelings of isolation and realize you’re not alone.
- Partner-inclusive interventions: Involving your partner in therapy can strengthen your relationship and ensure you both feel supported.
- Self-care strategies: Prioritizing sleep (even in short stretches), nutrition, and gentle movement are essential for recovery.
- Medication: Antidepressants, many of which are safe for breastfeeding, can be very effective for moderate to severe PPD, especially when combined with therapy.
- Community resources: Look for local home visiting programs, parenting classes, or other services for new parents that can reduce stress.

How to Find a CBT Therapist
Finding the right therapist can feel like another overwhelming task, but there are clear paths forward:
- Ask your doctor or OB/GYN: They can provide referrals to trusted perinatal mental health specialists.
- Use online therapist directories: Websites like Psychology Today or the Association for Behavioral and Cognitive Therapies (ABCT) allow you to filter for therapists specializing in PPD.
- Contact local mental health clinics: These often have programs for new parents and may offer sliding-scale fees.
- Check university psychology departments: They sometimes offer reduced-cost therapy with supervised graduate students.
At Addiction Helpline America, we know taking the first step is hard. We connect individuals across all 50 states—from Alabama to Wyoming—to qualified mental health treatment centers, free and confidentially. Whether you need CBT for postpartum depression or other services, we can help you find providers in your area. You can contact us 24/7 to find the care you deserve.
Frequently Asked Questions about CBT for PPD
How long does CBT take to work for postpartum depression?
Most courses of CBT for PPD involve 12 to 16 sessions. Many mothers begin to notice improvements within just a few weeks as they start applying new strategies. The goal of CBT is to build lasting skills for managing your thoughts and behaviors, so the benefits often continue long after therapy ends.
Can CBT help with postpartum anxiety too?
Yes, absolutely. Postpartum anxiety often co-occurs with depression, affecting as many as 1 in 6 new mothers. CBT is highly effective for both because it targets the same underlying negative thought patterns and behaviors that fuel both conditions. Research confirms CBT’s effectiveness for perinatal anxiety, helping you challenge racing thoughts, reduce worry, and calm your nervous system.
Is online CBT as effective as in-person therapy for PPD?
Yes, research shows that online CBT with professional guidance is very effective for PPD. It offers huge practical advantages, eliminating barriers like childcare and travel. You can attend sessions from home, which increases access to care, especially for those in rural areas or with limited mobility. While some prefer in-person connection, online and blended formats can be just as impactful. The best therapy is the one you can attend consistently.
At Addiction Helpline America, we understand that every mother’s situation is unique. Whether you’re searching for in-person or online CBT for postpartum depression, we can help connect you with qualified providers who offer the format that fits your needs. Contact us anytime for personalized guidance in
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
finding the right support.
Conclusion
The journey through postpartum depression is challenging, but you don’t have to face it alone. CBT for postpartum depression is a practical, empowering, and evidence-based approach that gives you concrete tools to manage your thoughts, change your behaviors, and build lasting skills. It helps you challenge your inner critic, take small steps toward feeling better, and learn to care for yourself while caring for your baby. Help is available in various formats, including in-person, group, and online therapy, to fit your life.
You are not weak for struggling; you are experiencing a treatable medical condition. Seeking support is a sign of strength for both you and your baby.
At Addiction Helpline America, our mission is to make finding help easier. We provide free, confidential support 24/7, connecting you with qualified perinatal mental health professionals across all 50 states. If you’re ready to take the next step, or just need to talk about your options, we’re here to listen and guide you toward the personalized support you deserve.
Find personalized mental health support
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.















