Your Right to Choose: Understanding Mental Health Treatment Decisions
Can I refuse mental health treatment? Yes, in most circumstances you have the legal right to refuse mental health treatment. However, there are specific situations where treatment may be provided without your consent, particularly when you pose a danger to yourself or others, or when you’re deemed incapable of making treatment decisions.
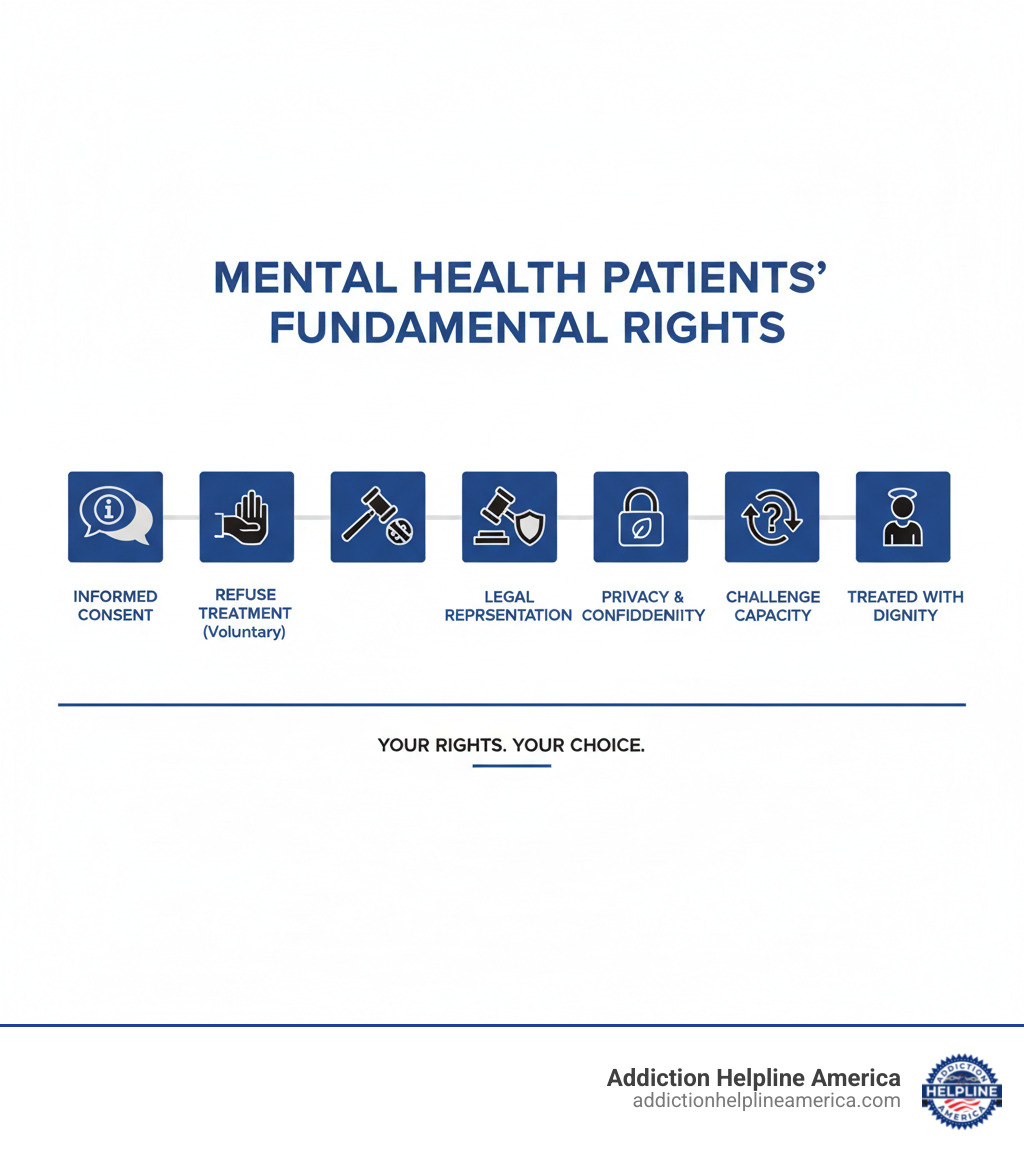
Quick Answer: Your Rights at a Glance
- Voluntary patients: Can refuse any treatment and leave the hospital
- Involuntary patients: May be treated without consent under specific legal criteria
- Capacity required: You must understand treatment information and consequences
- Emergency exceptions: Treatment may be given to prevent immediate harm
- Legal recourse: You can challenge decisions through the Consent and Capacity Board
- Age considerations: No specific age limit – capacity is assessed individually
The question of refusing mental health treatment sits at the heart of medical ethics and personal autonomy. As one legal expert notes, “patients’ right to refuse treatment has been not nearly so hard for clinicians to live with as they had feared.”
Your right to make decisions about your own body and mind is fundamental. Yet mental health law creates a complex balance between respecting your autonomy and ensuring safety when judgment may be impaired by illness.
Understanding the legal landscape is crucial. Laws vary significantly by location, and what applies in one province or state may not apply in another. This guide uses Ontario’s legal framework as a detailed example, but the principles often mirror those found across North America.
At Addiction Helpline America, we’ve helped thousands of individuals and families steer complex mental health and addiction treatment decisions, including situations where someone asks can I refuse mental health treatment. Our experience shows that understanding your rights empowers better decision-making and often leads to more successful treatment outcomes.
The Foundation of Treatment Decisions: Consent and Capacity
Think of medical consent like making any important life decision – you wouldn’t buy a house without understanding the terms, right? Can I refuse mental health treatment becomes much clearer when you understand how consent actually works in healthcare.
In Ontario, your rights as a mental health patient are protected by two key pieces of legislation: the Health Care Consent Act and the Mental Health Act. These laws ensure that you have the same fundamental rights as any other patient – the right to be treated with respect, to make informed decisions about your care, and to have your privacy protected.
Your healthcare providers aren’t just being polite when they explain treatments to you – they’re legally required to respect these rights. It’s their professional and legal obligation to make sure you understand what’s happening with your care.
What is ‘Informed Consent’ for Mental Health Treatment?
Imagine ordering dinner at a restaurant. You’d want to know what’s in the dish, how spicy it is, and what your other options are, especially if you have allergies. Informed consent for mental health treatment works the same way, but with much higher stakes than your dinner choice.
For your consent to be legally valid, your healthcare provider must explain several key things to you. First, they need to describe the nature of the treatment – whether it’s medication, therapy, or a specific procedure. You deserve to know exactly what they’re proposing.
Next, they must explain the benefits and risks involved. What positive changes can you expect? What side effects or complications might occur? This includes both common issues and serious problems that might be rare but important to know about.
Your provider should also discuss alternative options available to you. There’s often more than one way to approach mental health treatment, and you have the right to know about different paths you could take.
They must explain the consequences of refusal too. What might happen if you decide not to go with the recommended treatment? This isn’t meant to pressure you – it’s about helping you make a fully informed choice.
Most importantly, you have the right to ask questions – as many as you need. Think of this as a conversation, not a lecture. Your healthcare provider should answer honestly and thoroughly until you feel comfortable with your understanding.
For more detailed information about these requirements, you can review A guide to the Health Care Consent Act.
How is Capacity to Consent Determined?
Here’s something that surprises many people: capacity isn’t like eye color – it’s not something fixed that you either have or don’t have. Instead, it’s more like a skill that can change depending on the situation and even from day to day.
When healthcare providers assess your capacity, they’re looking at two main things. Can you understand the information about your treatment? And can you appreciate the consequences of either agreeing to or refusing that treatment?
This assessment varies by treatment complexity. You might have the capacity to decide about weekly therapy sessions but not about a complex medication regimen. Or you might be able to make decisions about some treatments but not others. That’s completely normal.
Age is not the sole factor in determining capacity. While maturity matters, it’s not about hitting a magic birthday. The law focuses on your actual ability to understand and appreciate the consequences, regardless of how old you are.
Here’s something reassuring: you’re always presumed to have capacity unless proven otherwise. The burden is on your healthcare provider to assess and determine if you lack capacity – you don’t have to prove that you’re capable.
It’s also important to know that capacity is not a fixed state. Mental health conditions can affect your ability to make decisions, and this can fluctuate. You might have full capacity one day but not the next, and that’s okay. The assessment should reflect your abilities at the time the decision needs to be made.
What About Children and Youth?
When it comes to young people and mental health treatment, Ontario takes a thoughtful approach. There’s no specific age of consent written into law. Instead, each young person is assessed individually using the same capacity test that applies to adults.
A teenager could be found capable of making their own treatment decisions if they understand the relevant information and can appreciate the consequences. This means a 15-year-old might be able to consent to their own therapy, while an 18-year-old might not have capacity for a particular decision, depending on their individual circumstances.
When a young person is found incapable of making treatment decisions, a substitute decision-maker (usually a parent or guardian) steps in. However, this person must make decisions based on the young person’s best interests while still considering the youth’s own wishes and preferences.
Young patients have several important rights: the right to privacy about their health information if they’re capable, the right to refuse treatment when they have capacity, the right to disagree with recommendations and have their concerns heard, the right to a rights adviser if they’re under 16 and found incapable regarding psychiatric facility admission, and the right to have alternatives explored rather than being forced into decisions they don’t understand or agree with.
At Addiction Helpline America, we often work with families navigating these complex situations. Understanding these rights helps both young people and their families make better decisions about mental health care.
Can I Refuse Mental Health Treatment? Understanding Your Rights
The core question—can I refuse mental health treatment?—touches the very heart of personal autonomy in healthcare. Your answer depends largely on whether you’re receiving care voluntarily or have been placed on an involuntary hold, and whether you’re deemed capable of making your own treatment decisions.
As a mental health patient, you possess robust rights that are carefully protected by law. Your privacy and confidentiality are fundamental—your personal health information generally cannot be shared without your consent, except in specific legal circumstances like court orders or situations where there’s a duty to warn someone of potential harm.
However, these rights can be limited in certain situations, particularly when there are serious concerns about your safety or the safety of others. Understanding when and how these limitations apply is crucial for anyone navigating the mental health system.
The distinction between voluntary and involuntary status shapes your rights significantly:
| Feature | Voluntary Patient | Involuntary Patient |
|---|---|---|
| Right to refuse treatment | Can refuse any treatment offered | Limited ability to refuse; treatment may be given without consent under specific criteria |
| Right to leave | Can leave the hospital at any time | Cannot leave until legally discharged or hold is lifted |
| Consent requirements | Must provide informed consent for all treatments | Treatment may proceed without consent if deemed incapable or in emergency situations |
| Legal representation | Can seek legal counsel if desired | Entitled to rights advice and legal representation |
| Appeal options | Can challenge capacity findings | Can appeal involuntary status and treatment decisions through the Consent and Capacity Board |
When Can I Refuse Mental Health Treatment?
If you’re a voluntary patient, your right to refuse treatment is quite strong. You entered care willingly, and you maintain the right to leave the hospital whenever you choose. You also have the right to refuse any treatment that’s recommended to you.
This doesn’t mean healthcare providers will simply accept your refusal without discussion. They have a professional obligation to help you understand the potential consequences of refusing treatment. Exploring alternatives with your care team is often the most productive approach—perhaps there’s a different medication, therapy approach, or treatment schedule that feels more acceptable to you.
When you do refuse treatment, healthcare providers are required to document your refusal properly. This protects both you and them, ensuring there’s a clear record of your informed decision.
When Can Treatment Be Given Without Consent?
The landscape changes significantly for patients on involuntary admission. In these situations, treatment may be provided without your consent under specific legal criteria.
Emergency situations represent the most common exception to consent requirements. When you pose an immediate danger to yourself or others, healthcare providers may administer treatment to prevent serious harm. This might include emergency medications to manage severe agitation or psychosis.
The concept of grave disability also comes into play—if your mental health condition severely impairs your ability to care for yourself, treatment may be provided without consent to prevent serious deterioration in your health or safety.
Sometimes a Substitute Decision-Maker (SDM) may consent to treatment on your behalf if you’re found incapable of making treatment decisions. This person—often a family member or appointed guardian—must make decisions based on your previously expressed wishes or, if those aren’t known, your best interests.
What is a Community Treatment Order (CTO)?
A Community Treatment Order represents a middle ground between voluntary outpatient care and involuntary hospitalization. Think of it as supervised community care with legal teeth.
The purpose of a CTO is to allow individuals with serious mental illness to live in the community while ensuring they receive necessary treatment. It’s designed for people who have a pattern of stopping treatment and subsequently requiring hospitalization.
Criteria for issuance are quite specific. You must have a serious mental disorder, have been hospitalized for psychiatric treatment at least twice in the previous three years, and be likely to cause serious harm to yourself or others or suffer substantial mental deterioration without continued treatment.
Under a CTO, you receive community-based supervision from a treatment team. You’re required to follow a treatment plan that might include taking medication, attending appointments, or living in a specific residence.
Consequences of non-compliance can be serious. If you don’t follow the CTO requirements, you may be apprehended and returned to the hospital for assessment. However, the renewal process requires regular review—CTOs aren’t permanent and must be justified at each renewal period.
Understanding these nuances helps you steer what can feel like an overwhelming system. At Addiction Helpline America, we’ve seen how knowledge of your rights can transform the treatment experience, often leading to better cooperation with care teams and more successful outcomes.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.