Understanding Buprenorphine Naloxone: A Lifeline for Opioid Use Disorder
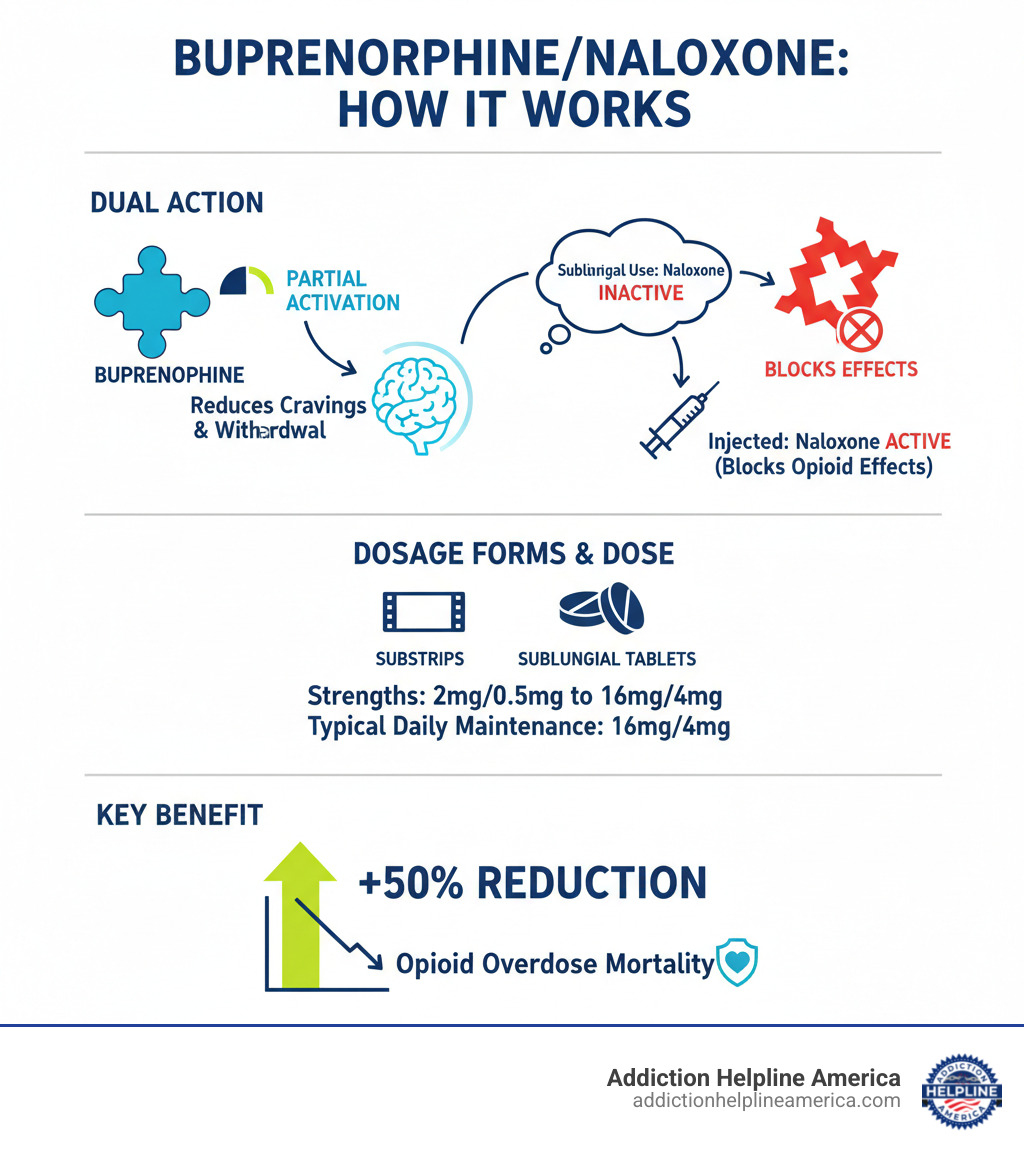
Buprenorphine naloxone is a combination medication for treating opioid use disorder (OUD). It reduces cravings and prevents withdrawal symptoms, giving people a real chance at recovery.
Quick Facts About Buprenorphine Naloxone:
- What it is: A combination of buprenorphine (a partial opioid agonist) and naloxone (an opioid antagonist).
- How it works: Reduces cravings and withdrawal without a full opioid high.
- Forms available: Sublingual films and tablets that dissolve under the tongue.
- Typical dose: 16 mg/4 mg daily for maintenance.
- Key benefit: Reduces opioid overdose death risk by up to 50%.
- Brand names: Suboxone, Zubsolv, Bunavail, and generics.
If you or a loved one is struggling with opioid addiction, there is hope. Buprenorphine naloxone is a “gold standard” treatment that helps people break free from opioid dependence while significantly reducing the risk of a fatal overdose.
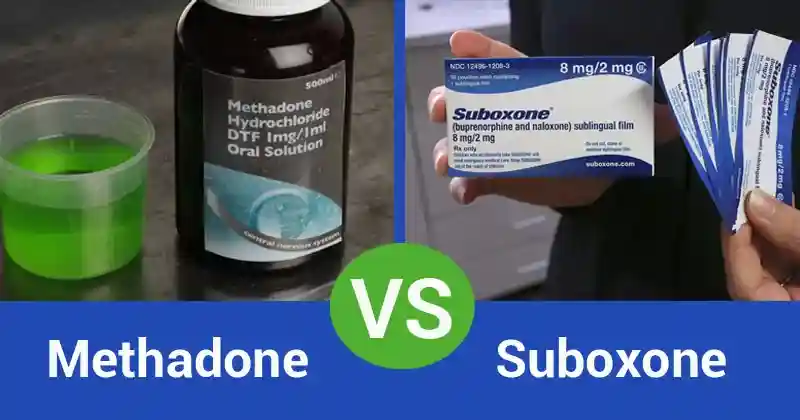
Unlike methadone, which often requires daily clinic visits, buprenorphine naloxone can be prescribed by qualified providers for at-home use. This accessibility allows people to maintain their daily lives while pursuing recovery.
The medication’s dual-action approach is key. Buprenorphine partially activates the brain’s opioid receptors, relieving withdrawal and cravings without causing an intense high. Naloxone is added as a safety measure; it’s inactive when taken as directed (under the tongue) but blocks opioid effects and can cause immediate withdrawal if injected, deterring misuse.
At Addiction Helpline America, we guide individuals and families through the complexities of OUD treatment, including buprenorphine naloxone therapy. Our team provides clear, compassionate information to help you steer your options.
This guide covers how buprenorphine naloxone works, how to use it safely, potential side effects, and its role in a comprehensive recovery plan. You’ll find practical, evidence-based answers for yourself or a loved one.
The Science Behind Buprenorphine/Naloxone in OUD Recovery
Understanding how buprenorphine naloxone works can be empowering. It’s a carefully designed tool that works with your brain chemistry to support recovery.
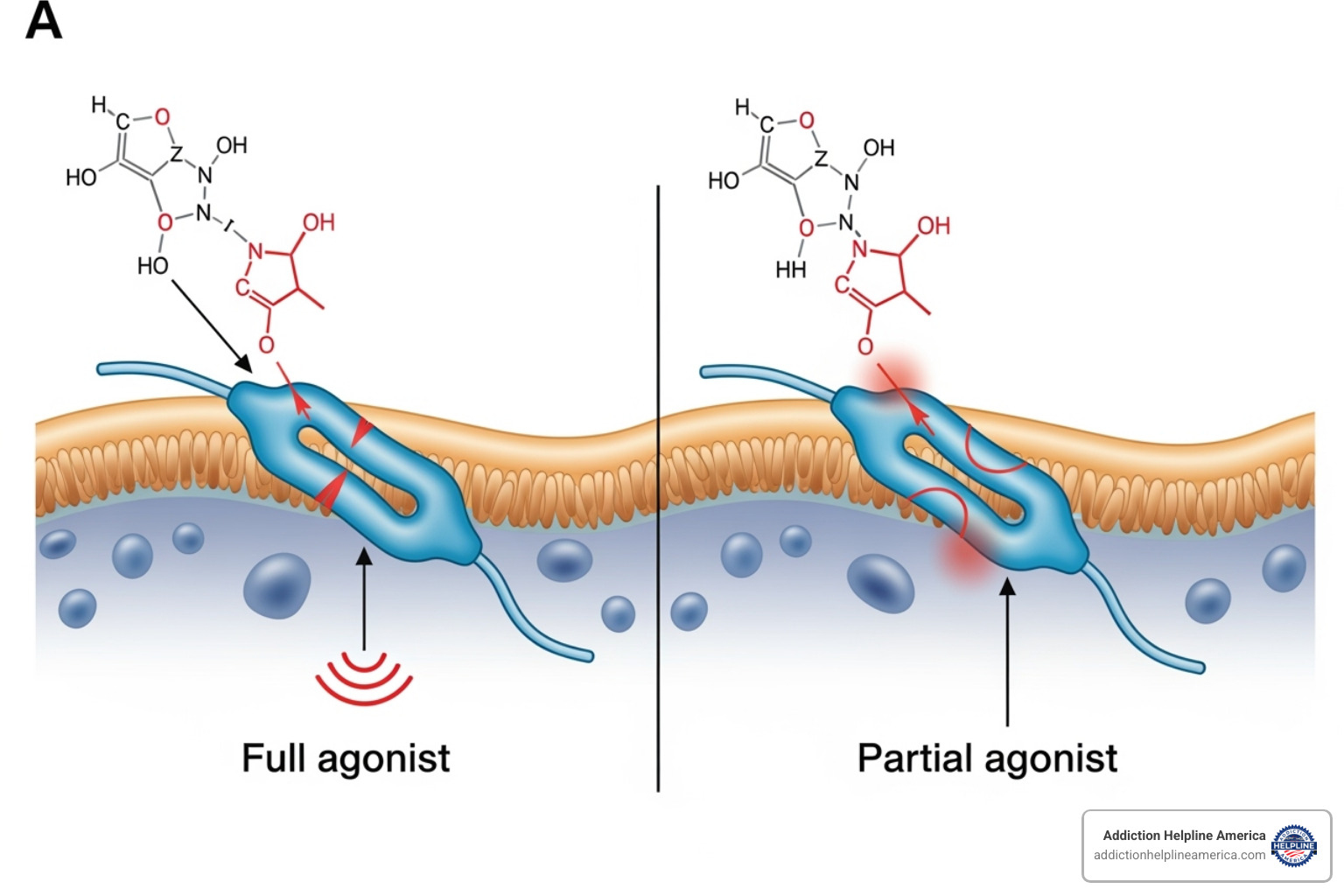
Think of your brain’s opioid receptors as locks. Full opioids like heroin or fentanyl are keys that turn the lock completely, causing intense effects. Buprenorphine is a partial mu-opioid receptor agonist—a key that only turns the lock partway. This partial activation is enough to stop cravings and withdrawal but not enough to cause a dangerous high. It stabilizes your brain, breaking the cycle of intoxication and crash.
Buprenorphine also has a “ceiling effect” on respiratory depression (slowed breathing), the main cause of fatal opioid overdoses. Unlike full agonists, its effect on breathing plateaus at higher doses, making it significantly safer. This feature helps reduce the risk of opioid overdose death by up to 50%.
How Buprenorphine Works
Buprenorphine is highly effective because it binds very tightly to mu-opioid receptors, more so than other opioids. This high affinity allows it to push other opioids off the receptors and block their effects. It also dissociates slowly, meaning it stays attached for a long time. This is why a single daily dose is usually enough to provide stability, reduce cravings, and ease withdrawal symptoms.
By satisfying the brain’s need for opioid stimulation without causing a high, buprenorphine gives you a chance to stabilize and focus on recovery. Dosing is targeted to manage symptoms and block the effects of other opioids. A maintenance dose of 16 to 24 mg daily is often the sweet spot where the brain feels stable and protected.
The Role of Naloxone
Naloxone, an opioid antagonist, is included purely as an abuse deterrent. When you take buprenorphine naloxone as directed (dissolving it under your tongue), very little naloxone is absorbed, and it has no effect.
However, if someone tries to inject the medication, the naloxone becomes fully active. It immediately blocks all opioid receptors, triggering sudden and severe withdrawal symptoms in an opioid-dependent person. This unpleasant effect strongly discourages misuse. The standard 4:1 ratio of buprenorphine to naloxone is designed to be safe when used correctly but effective as a deterrent, allowing for at-home use.
How Buprenorphine/Naloxone Fits into Recovery
Buprenorphine naloxone is most effective as part of Medication Assisted Treatment (MAT), which combines medication with counseling and behavioral support. The medication stabilizes your brain chemistry, creating the mental space to address the underlying causes of addiction.
This comprehensive approach has proven benefits:
- Lower overdose risk: By reducing the use of unpredictable street drugs.
- Improved treatment retention: Higher doses (16 to 32 mg) help people stay in treatment longer.
- Restored daily function: Stability allows you to focus on employment, relationships, and rebuilding your life.
- Reduced health risks: Lowers the risk of HIV, hepatitis C, and other complications.
Unlike methadone’s daily clinic visits, buprenorphine naloxone can be prescribed in an office setting and taken at home, making treatment more accessible. This flexibility is a key advantage for many people.
At Addiction Helpline America, we’ve seen MAT transform lives. We can help you find the right combination of medication, counseling, and support for your unique situation.
Your Guide to Using Buprenorphine Naloxone Safely
Using buprenorphine naloxone correctly is key to its effectiveness and your safety. The medication is designed to dissolve in your mouth, and proper administration makes a significant difference.
Dosage Forms
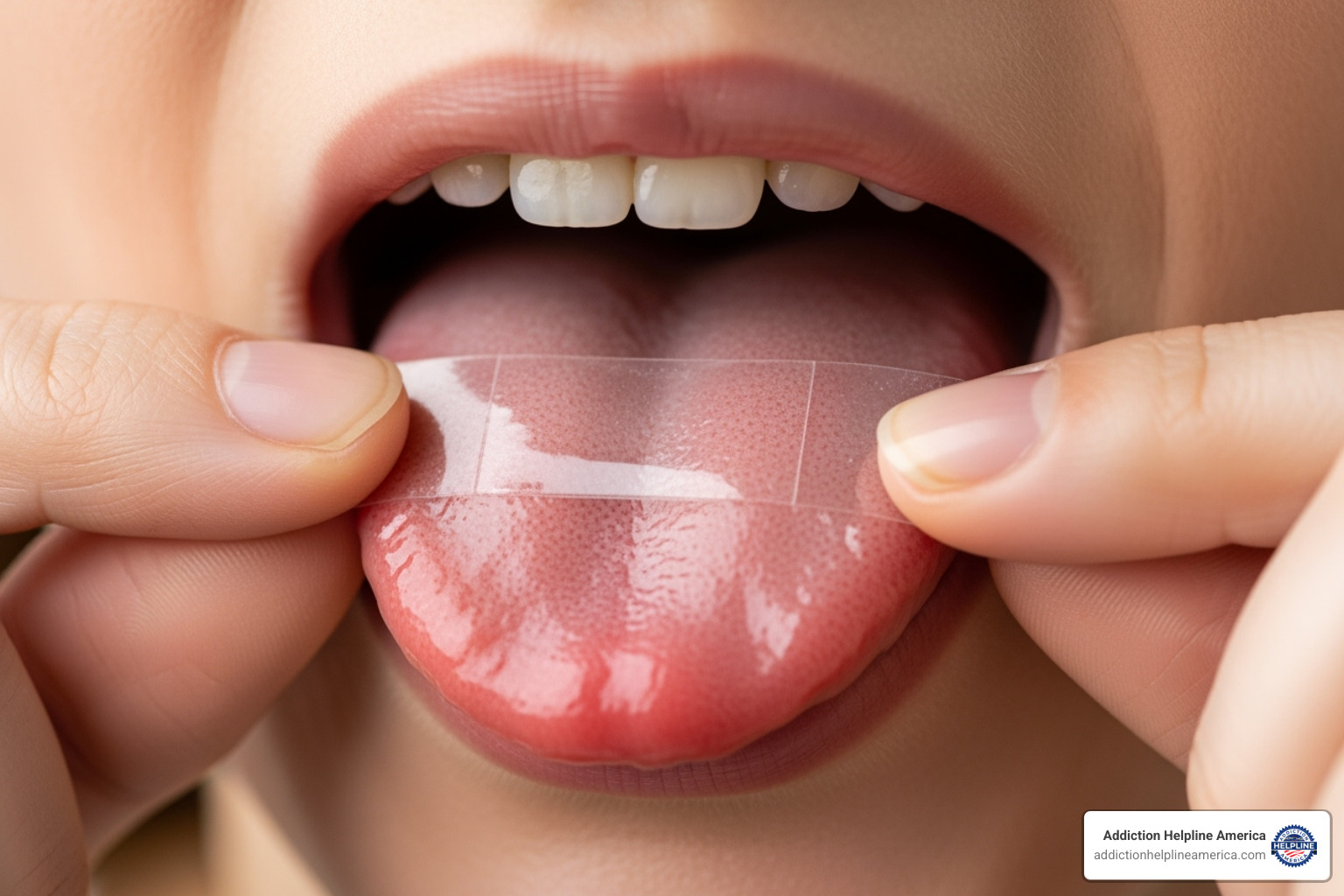
Buprenorphine naloxone is available as sublingual films (like Suboxone) or sublingual tablets that dissolve under the tongue. There are also buccal films placed inside the cheek. These forms come in various strengths.
Different brands and forms are not always interchangeable. For example, films may have higher bioavailability than tablets, meaning your body absorbs more of the medication. Never switch brands or forms without consulting your doctor, as your dose may need to be adjusted. Insurance coverage can also vary, with generic films often being the most accessible. Our team at Addiction Helpline America can help you steer these questions.
Proper Use of Sublingual Formulations
Correct use is crucial for effectiveness and dental health. The FDA has warned about dental problems like tooth decay and cavities if the medication is not used carefully.
- Moisten your mouth with a sip of water.
- With dry hands, place the film or tablet under your tongue (or inside your cheek for buccal forms).
- Let it dissolve completely without talking, chewing, or swallowing. This can take up to 10 minutes. If taking multiple doses, place them on opposite sides.
- Once dissolved, take a large sip of water, swish gently, and swallow to rinse your mouth.
Because the medication is acidic, it can harm your teeth over time. Wait at least one hour after your dose before brushing your teeth. See your dentist regularly and inform them you are taking this medication. Report any tooth pain or sensitivity to your doctor or dentist immediately. For more information, see the FDA’s guidance on protecting dental health.
Recommended Dosing for Buprenorphine Naloxone
Treatment occurs in two phases: induction and maintenance.
The induction phase is when you begin treatment, and timing is critical. You must be in mild to moderate withdrawal before your first dose. Taking it too soon can cause precipitated withdrawal—a sudden, severe onset of withdrawal symptoms. Your doctor will use a tool like the Clinical Opiate Withdrawal Scale (COWS) to determine if you’re ready. This typically means waiting 12 hours after short-acting opioids (heroin) or 48-72+ hours after long-acting ones (methadone, fentanyl).
Induction is best done under medical supervision. Your doctor will start you on a low dose (e.g., up to 4-8 mg) and increase it over the first couple of days.
Once stable, you enter the maintenance phase. The target dose for most people is 16 mg buprenorphine / 4 mg naloxone once daily, though some may need up to 24 mg. The goal is to eliminate cravings and withdrawal without sedation. Take your dose at the same time each day. Never adjust your dose or stop taking the medication without your doctor’s guidance, as a gradual taper is needed to prevent withdrawal.
Potential Side Effects, Interactions, and Risks
While most people tolerate buprenorphine naloxone well, it’s important to be aware of potential side effects, interactions, and risks. Knowing what to watch for ensures you can use this medication safely and effectively.
Common and Serious Side Effects
Common side effects are often mild and may improve as your body adjusts. These include:
- Headache, nausea, and constipation
- Increased sweating or trouble sleeping
- Numbness or redness in the mouth where the medication dissolves
- Mild opioid withdrawal symptoms if the dose is too low or started too soon
Serious side effects are rare but require immediate medical attention. Call your doctor or 911 if you experience:
- Trouble breathing: Slow, shallow, or stopped breathing is a medical emergency.
- Signs of liver problems: Yellowing skin or eyes, severe stomach pain, or dark urine.
- Adrenal insufficiency: Severe fatigue, weakness, or persistent dizziness.
- Allergic reaction: Rash, itching, or swelling of the face or throat.
- Heart rhythm changes or symptoms of serotonin syndrome (agitation, fever, rapid heartbeat) if taking certain antidepressants.
Dangerous Drug Interactions
Mixing buprenorphine naloxone with certain substances can be life-threatening.
The most dangerous combination is with other central nervous system (CNS) depressants like benzodiazepines (Xanax, Valium), alcohol, and other sedatives. This mix can cause severe respiratory depression, coma, and death. Be completely honest with your doctor about any alcohol or other drug use.
Other significant interactions include:
- MAO inhibitors: A class of antidepressants that should not be used within 14 days of buprenorphine naloxone.
- CYP3A4 inhibitors/inducers: Certain antibiotics, antifungals, and seizure medications can alter buprenorphine levels in your body, requiring a dose adjustment.
- Other opioids: Taking other opioids can lead to unpredictable effects and increased overdose risk.
- Naltrexone: This medication will block buprenorphine and cause severe withdrawal.
Always tell your doctor about every medication, supplement, and over-the-counter drug you take.
Overdose Symptoms and Long-Term Health Concerns
Overdose is possible, especially when buprenorphine naloxone is mixed with other substances. Signs of an overdose include extreme sleepiness, confusion, pinpoint pupils, and very slow or stopped breathing. If you suspect an overdose, call 911 immediately and administer naloxone (Narcan) if available.
Long-term health considerations include:
- Dental problems: The acidity of sublingual medication can cause tooth decay. Regular dental visits and rinsing your mouth with water after each dose are crucial.
- Hormonal changes: Long-term opioid use can affect hormone levels. Talk to your doctor about any changes in energy, mood, or sexual function.
- Physical dependence: Your body will become physically dependent on the medication, meaning you will experience withdrawal if you stop suddenly. Discontinuation must be done under a doctor’s supervision with a gradual taper.
Special Populations and Safety Considerations
Treatment with buprenorphine naloxone must be custom to the individual. Certain circumstances, such as pregnancy, age, or specific health conditions, require special consideration to ensure safety and effectiveness.
Use During Pregnancy and Breastfeeding
For pregnant women with OUD, the benefits of treatment with buprenorphine generally outweigh the risks of untreated addiction. Untreated OUD poses severe risks to the baby, including preterm birth and stillbirth. While a baby may experience Neonatal Opioid Withdrawal Syndrome (NOWS) after birth, this condition is expected and treatable. Research suggests buprenorphine may lead to less severe NOWS compared to methadone. Some doctors may prescribe buprenorphine without naloxone during pregnancy.
Regarding breastfeeding, buprenorphine passes into breast milk in very low amounts. While caution is advised, many mothers can safely breastfeed. It’s important to monitor the infant for unusual sleepiness or feeding difficulties and discuss the decision with your healthcare provider.
Understanding Use in Special Populations
Adjustments may be needed for different populations to ensure safe and effective treatment.
- Naloxone sensitivity: A small number of people may experience side effects like headaches or nausea from the naloxone component. In these rare cases, a switch to a buprenorphine-only product may be necessary.
- Elderly patients: May be more sensitive to the medication and often require lower starting doses and closer monitoring.
- Hepatic impairment (liver problems): Since the liver processes buprenorphine, the medication is not recommended for those with severe liver impairment and must be used cautiously in those with moderate issues. Liver function should be monitored.
| Population | Key Considerations for Buprenorphine/Naloxone Use |
|---|---|
| Pregnant Women | Treatment benefits typically outweigh risks of untreated OUD; NOWS is expected but treatable; buprenorphine may cause less severe neonatal withdrawal than methadone; some providers prefer buprenorphine mono-product to avoid naloxone exposure; close medical supervision essential throughout pregnancy |
| Breastfeeding Mothers | Minimal buprenorphine transfer to breast milk (less than 1% of maternal dose); monitor infant for unusual sleepiness, feeding difficulties, or breathing problems; benefits often outweigh risks; discuss with healthcare provider |
| Elderly Patients | May require lower starting doses; increased sensitivity to medication effects; closer monitoring needed; age-related changes in liver, kidney, and heart function require consideration |
| Patients with Liver Problems | Not recommended for severe hepatic impairment; use with caution in moderate impairment; liver function tests required before and during treatment; dose adjustments may be necessary |
| Naloxone-Sensitive Patients | Rare but possible adverse reactions to naloxone component even when taken sublingually; symptoms include nausea, headache, anxiety after dosing; may benefit from switching to buprenorphine mono-product; maintaining therapeutic alliance is crucial |
Legal and Safety Risks of Misusing Buprenorphine Naloxone
Buprenorphine naloxone is a Schedule III controlled substance, meaning it has potential for misuse. Diversion—sharing or selling your medication—is illegal and dangerous. What is safe for you could be harmful to someone else.
Accidental exposure to children is a critical risk. A single dose can be fatal to a child. To prevent this:
- Store your medication safely in its original packaging, in a locked cabinet or box, out of sight and reach of children and pets.
- Count your doses to know if any are missing.
- Dispose of unused medication properly through a take-back program or by following FDA guidelines.
Understanding these risks helps protect you, your family, and your community.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.